Congenital Giant Teratoma Arising from the Hard Palate: A Rare Clinical Presentation
Kandukuri Mahesh Kumar1, Indira Veligandla2, A.R.Vijaya Lakshmi3, Vanita Pandey4
1 Assistant Professor, Department of Pathology, Malla Reddy Institute of Medical Sciences, Suraram, Hyderabad, Telangana, India.
2 Professor and Head, Department of Pathology, Malla Reddy Institute of Medical Sciences, Suraram, Hyderabad, Telangana, India.
3 Professor and Head, Department of Gynaecology and Obstetrics, Malla Reddy Institute of Medical Sciences, Suraram, Hyderabad, Telangana, India.
4 Assistant Professor, Department of Pathology, Malla Reddy Institute of Medical Sciences, Suraram, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kandukuri Mahesh Kumar, H.No.7-1-390, Flat No 503, Sri Sai Residency, Balkampet, Sanjeeva Reddy Nagar, Hyderabad, Telangana State (TS)- 500038, India.
E-mail: doctormaheshgoud@gmail.com
Teratomas are rare tumours which originate from all 3 germs cell layers namely endoderm, mesoderm and ectoderm, with varying proportions of each component. The most common site of teratoma is in the sacro-coccygeal region. Teratomas are generally benign and have well appreciable clinical and histopathological features. Incidence of congenital teratoma is 1 in 4000. In head and neck region congenital teratomas usually associated with other anomalies like cystic hygroma and cleft palate with an incidence of 1 in 400. The approximately reported incidence of palatal teratoma is 1 in 35000 to 40000 live-births. Upper airway difficulty causes anticipated functional problems at hypopharynx.
The prognosis of palatal teratoma mostly depends on the risk and extent of neonatal respiratory distress. We present a rare case of congenital teratoma arising from the hard palate in a new born girl. The outcome in this case was bad due to the large mass causing respiratory difficulty and bleeding from the ruptured cystic areas leading to hypovolemic shock. After two hours of delivery, baby expired.
Epignathus teratoma, Resuscitation, Ultrasonography
Case Report
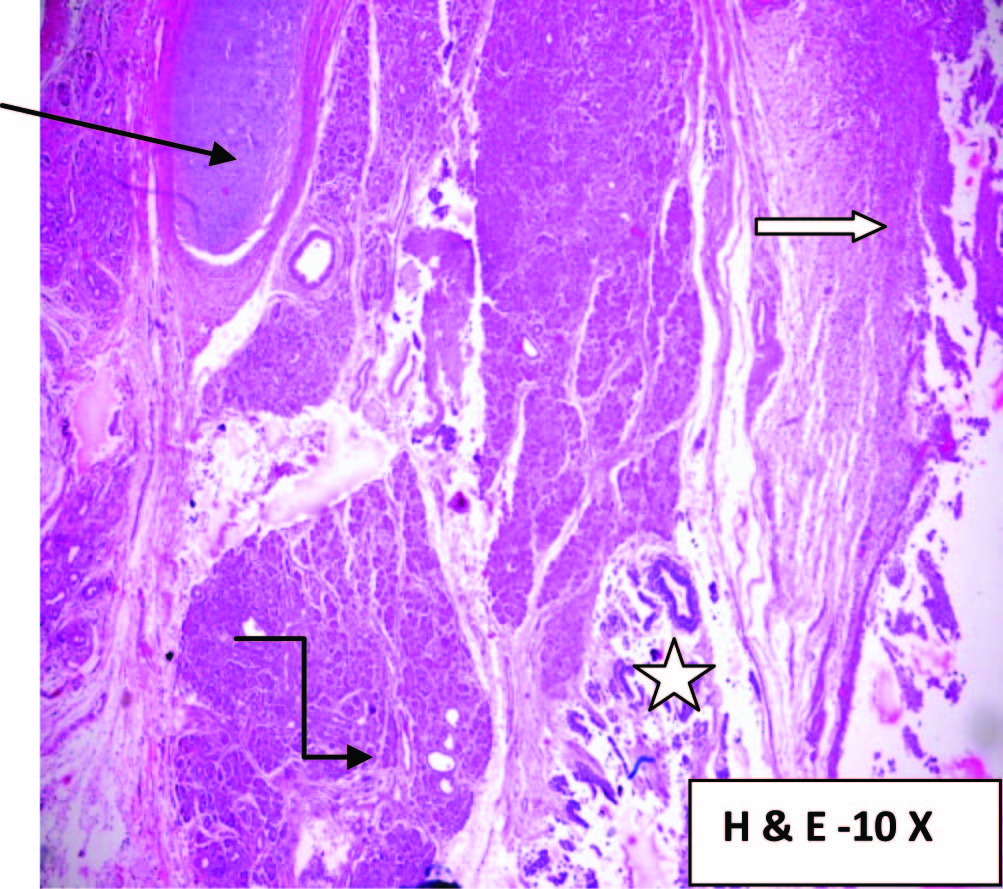
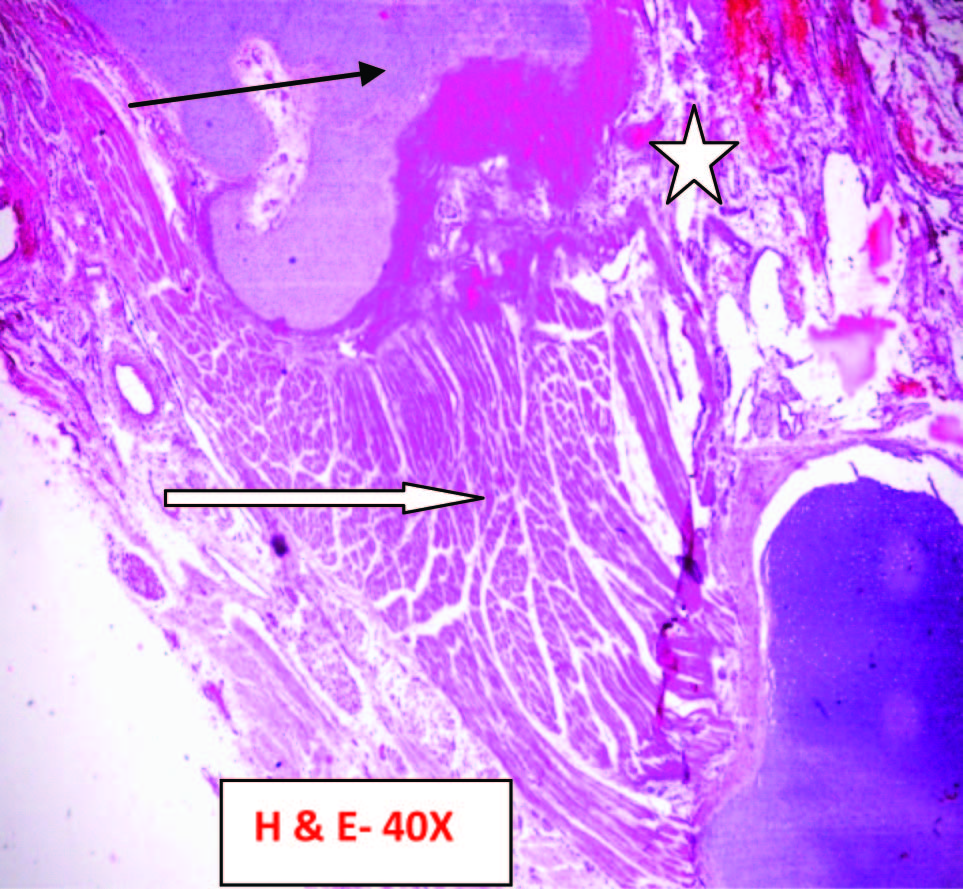
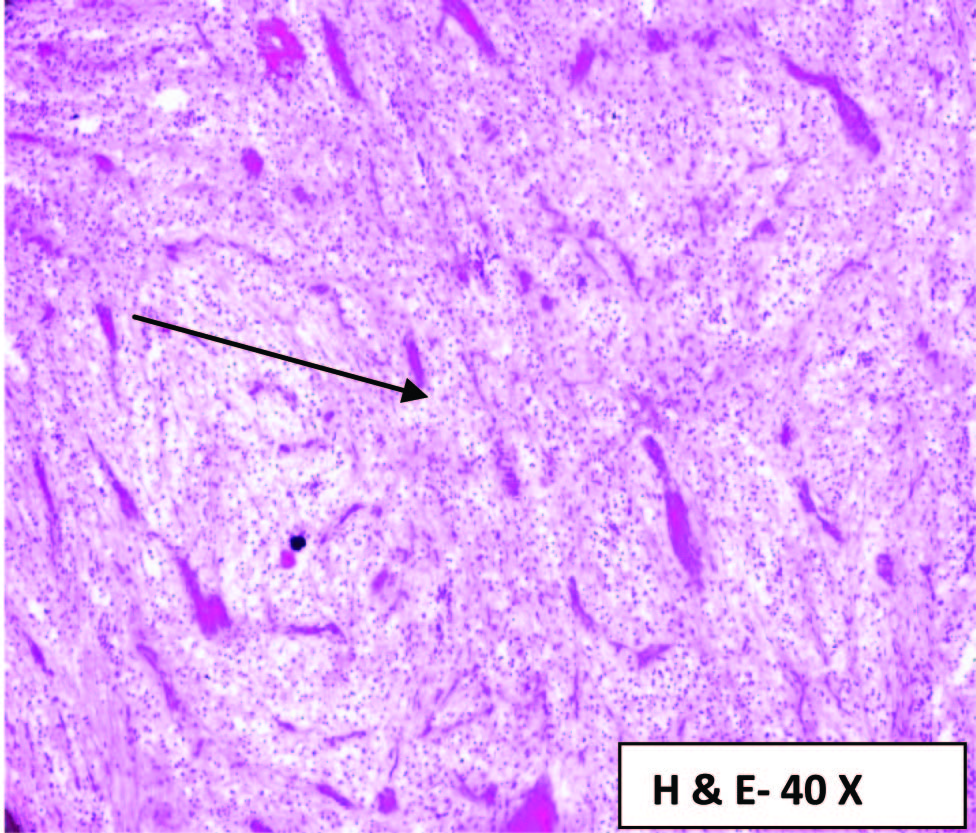
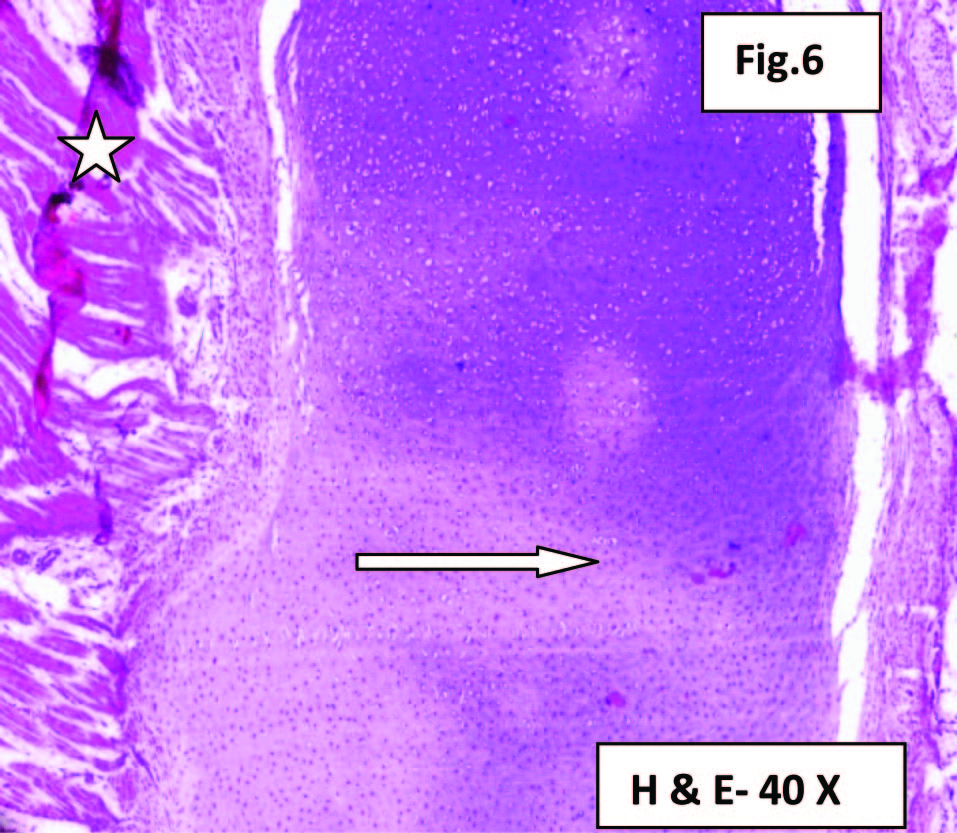
A female infant was delivered through Lower Segment Caesarian Section (LSCS) by a 20-year-old gravida 2 after 32 weeks of gestation. Weight of the new born along with a pedunculated mass from the palate is 2.95 kg. Her first pregnancy aborted in 5th month, there was no clear evidence of the cause for the abortion. The mother underwent only one ultrasound scanning at gestational age of 8 weeks. No other prenatal scanning and procedures were done before reporting to our hospital in the second and third trimesters. Her present pregnancy was not documented/unbooked case. Immediately after admission a scan was done at 32 weeks gestation which indicated a parasitic twin or a possibility of omphalocele. Patient was posted for emergency LSCS. Newborn Apgar score at one minute was 6 and at 5 minutes were 3. The newborn was immediately intubated. There was bleeding from cystic areas of the hard palate mass. Resuscitation by pediatricians and anesthetics for 3 hours could not save the newborn [Table/Fig-1]. Fetal autopsy was performed on the Day 3 with consent from the parents and after the approval of the ethical committee of the institute. Grossly, a pedunculated mass was seen arising from the roof of the hard palate measuring 17x11x6cm, partly solid and cystic [Table/Fig-2]. Focally, translucent and haemorrhagic areas seen. Cut section of the mass show focal cystic spaces filled with clear to mucoid fluid and gritty areas. No Intracranial extension noted. No similar swellings in the body noted. The origin is confirmed as hard palate on thorough dissection. Bits were taken from representative areas and processed for histopathological examination. Fetal autopsy did not reveal any other congenital anamoly. Histopathology revealed tissues from all the three germ cell layer which included glial tissue, muscle tissue, cartilage, bone, skin, respiratory epithelium and gastric glands [Table/Fig-3,4,5 and 6].
New born baby under resuscitation.

Gross examination of the new born with hard palate mass before the autopsy.

Photomicrograph showing cartilage (Straight arrow- black), Pancreatic acini (Right Angled arrow), glandular Epithelium (White Star) and fibrocollagenous tissue (White arrow) (Hematoxylin and Eosin Stain- H & E).
Photomicrograph showing cartilage (Black Arrow), muscle bundles (White Arrow), vascular channels (White Star) (H & E Stain).
Tissue sections showing glial tissue (Black Arrow) (H & E Stain).
Tissue sections showing cartilage (White Arrow) and muscle bundles (White Star) (H & E Stain).
Discussion
The word Teratoma was first coined and defined by the famous scientist Virchow in the first edition of his book on tumours published in 1863. Teratomas range from benign to malignant, solid to cystic. Teratoma arises from totipotent cells; the cells which give rise to ectoderm, endoderm and mesoderm, these tumours typically are midline or paraxial. The most common location is sacrococcygeal (57%). Cystic teratomas occasionally occur in sequestered midline embryonic cell rests [1,2] and can be mediastinal (7%), retroperitoneal (4%), cervical (3%), and intracranial (3%). Tumour arising from hard and soft palate and Rathke’s pouch are known as epignathus teratomas.
Teratomas have diversified aetiology; chromosomal abnormalities are associated with the cases of congenital teratomas which commonly include trisomy 13, ring X-chromosome, mosaicism with inactive ring X-chromosome, gonosomal pentasomy 49, gene mutations or abnormalities in early embryonic development.
Clinically, a hard palate teratoma appears as a large single mass or multiple tiny lesions with a pedicle or sessile. Airway obstruction is the main complication and is related to the size and site of the lesion occurring in 80% to 100% of cases [3]. Clinical differential diagnoses of neonatal oral mass include: embryonic congenital rhabdomyosarcoma, retinoblastoma, nasal glioma, heterotopic thyroid, cystic lymphangioma of the oro or nasopharyngeal regions, and sphenoid meningoencephalocele [4].
In extensive search of literature, only three articles were reported so far. One by Mohsen Rouzrokh et al., arising from the soft palate reported in 2015, second case was reported by R Hu et al., arising from the soft palate with recurrence in the year 2013, third case was a nasopharyngeal teratoma reported by Alireza Mirshemirani et al., in year 2011 [5–7]. All the tumours were of smaller size and surgical intervention done.
The diagnosis can be made in-utero by non-invasive technique such as ultrasonography in the first or second trimester of pregnancy. A 3-Dimenional Ultrasonography and Magnetic Resonance Imaging (MRI) may enhance the accuracy of the antenatal diagnosis and may help in the selection of newborns requiring early intervention.
If antenatal diagnosis is made, two treatment procedures may be used: intrapartum treatment (EXIT) procedures [8] and operation on placental support (OOPS) [9].
In the EXIT procedure, after a low transverse uterine incision, the head and at least one hand of the fetus are delivered [10]. In the OOPS procedure, first the airway is secured by endotracheal intubation or tracheostomy, later the baby is completely delivered and the umbilical cord is clamped. In our case, the pregnant lady did not attend the ultrasonography scan in the second trimester. Third trimester scan indicated a parasitic twin or a possibility of omphalocele. LSCS was done and delivered a female child with a pedunculated mass arising from hard palate, immediately newborn was intubated and resuscitated but the efforts were not successful.
Conclusion
To conclude, congenital hard palate teratomas or epignathus teratomas are rare tumours which can be diagnosed during antenatal visits by a simple investigation modality such as ultrasonography and proper plan can be made to terminate the pregnancy in cases of large and untreatable lesions with high rate of mortality and morbidity.
[1]. Becker S, Schon R, Gutwald R, A congenital teratoma with a cleft palate: report of a caseBr J Oral Maxillofacial Surg 2007 45(4):326-27. [Google Scholar]
[2]. Barksdale EM Jr, Obokhare I, Teratomas in infants and childrenCurrent Opinion Pediatr 2009 21(3):344-49. [Google Scholar]
[3]. Bianchi B, Ferri A, Silini EM, Magnani C, Sesenna E, Congenital cervical teratoma: a case reportJ Oral Maxillofac Surg 2010 68:667-70. [Google Scholar]
[4]. He J, Wang Y, Zhu H, Nasopharyngeal teratoma associated with cleft palate in newborn: report of 2 casesOral Maxillofacial Surg 2010 109(2):211-16. [Google Scholar]
[5]. Rouzrokh M, Azizi F, Nilipour Y, Soft palatine mass with diagnosis of mature teratomaInternational Journal of Surgery Case Reports 2015 8:71-72. [Google Scholar]
[6]. Hu R, Jiang RS, The recurrence of a soft palate teratoma in a neonate: a case reportHead Neck Oncol 2013 5(2):16 [Google Scholar]
[7]. Mirshemirani A, Khaleghnejad A, Mohajerzadeh L, Samsami M, Hasas-Yeganeh S, Congenital Nasopharyngeal Teratoma in a NeonateIran J Pediatr 2011 21(2):249-52. [Google Scholar]
[8]. Myers LB, Bulich LA, Mizrahi A, Barnewolt C, Estroff J, Ultrasonographic guidance for the location of the trachea during the EXIT procedure for cervical teratomaJ Pediatr Surg 2003 38(4):E12 [Google Scholar]
[9]. Norris MC, Joseph J, Leighton BL, Anesthesia for perinatal surgeryAm J Perinatol 1989 6(1):39-40. [Google Scholar]
[10]. Midrio P, Zadra N, Grismondi G, Suma V, Pitton MA, EXIT procedure in a twin gestation and review of the literatureAm J Perinatol 2001 18(7):357-62. [Google Scholar]