Case Report
A 30-year-old female patient presented with a complaint of a small growing mass in lower front teeth in Local Private Dental Clinic, Raichur, Karnataka, India. The growth started two months ago, as a small sessile painless growth that progressively increased to attain the size of 3×3cm at the time of presentation. On provocation, the growth showed profuse bleeding. The past medical history was non-contributory and assessment of the head and neck region revealed no cervical or submandibular lymph node enlargement.
Intraoral examination revealed full complement of teeth. However, there was a soft sessile growth arising from the labial gingiva in relation to 31 and 41 on the labial aspect extending distal to 32 [Table/Fig-1]. Palpatory findings revealed swelling measuring 3×3cm which was soft to firm in consistency. Also, mobility was seen in relation to 31 and 41. Intraoral periapical radiograph in relation to 31 and 41 revealed loss of alveolar crestal bone interproximally [Table/Fig-2]. With the above said findings, a provisional diagnosis of pyogenic granuloma on the labial gingiva in relation to 31 and 41 was established. Peripheral giant cell granuloma and peripheral fibroma were considered in the differential diagnosis.
Clinical photograph showing a soft sessile painless growth arising from the labial gingiva in relation to 31 and 41.

Intraoral periapical radiograph in relation to 31, 32, 41 and 42 revealed loss of alveolar crestal bone interproximally.

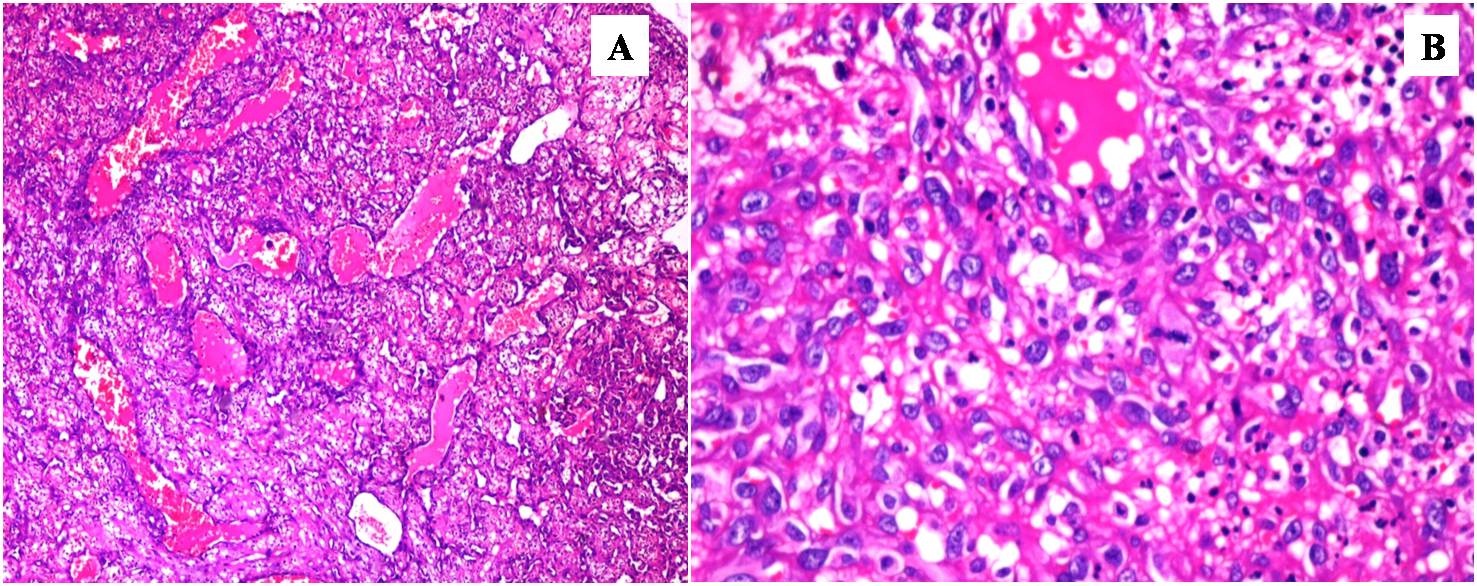
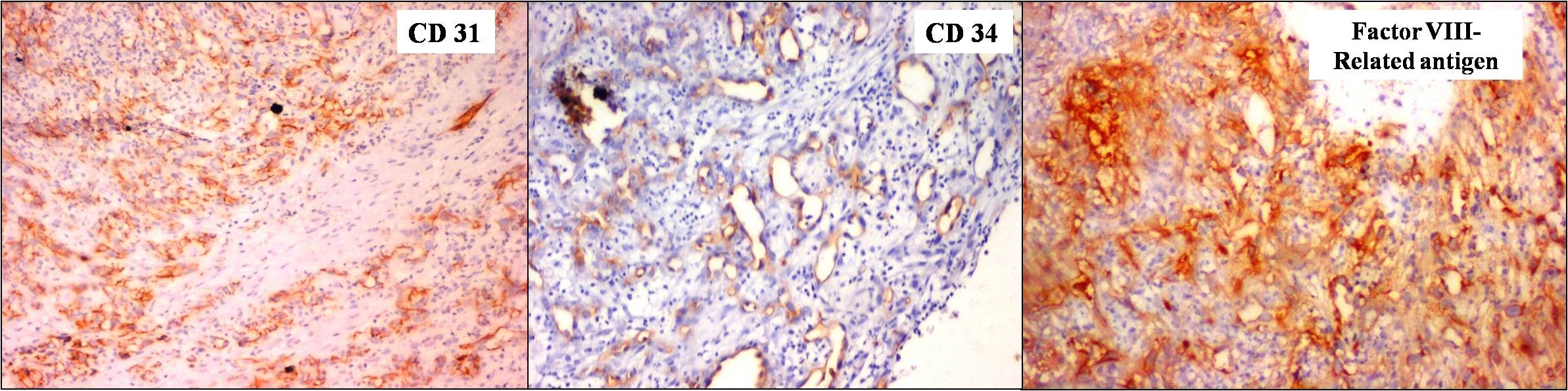
A local surgical excision was carried out under local anaesthesia and excisional biopsy was sent to Department of Oral Pathology, Navodaya Dental College, Raichur, Karnataka, India, for histopathological analysis. Serial sections revealed different microscopic aspects which confirmed that the lesion was pleomorphic. We observed large areas with distinctive vascular lumens, sometimes anastomosed. The tumour consisted of spindle to polygonal cells with hyperchromatic nuclei and conspicuous nucleoli with intracytoplasmic vacuoles and mitotic figure were also scattered [Table/Fig-3a,b]. Immunohistochemical staining revealed that the tumour cells were positive for CD1, CD34 and Factor VIII-related antigen [Table/Fig-4a-c]. A final histopathological diagnosis of angiosarcoma was given.
a) A photomicrograph showing large areas of distinctive vascular lumens, sometimes anastomosed (H & E, 10x). b) The tumour consisted of spindle to polygonal shaped cells with hyperchromatic nuclei and conspicuous nucleoli with intracytoplasmic vacuoles and mitotic figures are also seen (H & E, 20x).
Immunohistochemical staining revealed that the tumour cells were positive for CD31, CD34 and Factor VIII-related antigen (10x).
After two months, patient reported back with the same chief complaint. The growth was a soft exophytic nodular mass, with well-defined limits and a maximum diameter of 8 mm [Table/Fig-5]. The tumour was soft, white to pink in colour, with easy bleeding. A standard uptake value of 5.5 was observed during a PET scan examination (full body scan) and the report showed no metastasis to other areas. CT scan showed small soft tissue density lesion involving lower anterior teeth [Table/Fig-6]. Based on clinical, radiographic and histopathological findings, a recurrence of angiosarcoma was given. The operation was performed with about a 20-mm surgical margin that was negative for tumour invasion along with extraction of 31, 32, 33 and 41, 42, 43. The postoperative course was uneventful. So far, after a two-year follow-up, no recurrence and metastatic lesions were found [Table/Fig-7].
Clinical photograph of recurrence seen as a soft exophytic sessile mass, with well-defined limits and a maximum diameter of 8 mm with easy bleeding.

CT scan showing small soft tissue density lesion involving lower anterior teeth and PET examination (Full body scan) showed no metastasis to other areas.

Follow-up photograph after two years showing uneventful postoperative course with no recurrence.

Discussion
Angiosarcoma is a malignant mesenchymal tumour with a differentiation into vascular endothelium. Angiosarcomas constitute less than 1% of all malignant mesenchymal lesions. Although angiosarcoma can occur at any location, the most common sites are soft tegument areas and in the superficial soft tissues [1].
The angiosarcomas involving oral cavity and salivary glands correspond to 1% of all angiosarcomas reported in the literature and hence considered as particularly rare. This tumour can occur at any age, especially in elderly age group and affects males predominantly. Most of the time patients report at advanced stages with signs and symptoms of pain, tiredness, weight loss, bone pain, abnormal bleeding, intraoral lesion, anemia, enlarged lymph nodes, chest pain, pathologic fractures and difficulty in breathing [2].
Intraorally, angiosarcomas most of time present as well or ill-defined, polypoid nodular bluish or violet mass, reddish and soft to firm in consistency. Mucosal ulceration is not rare and is also related with bleeding on palpation and edema. Histopathologically, these tumours imitate the normal endothelial features and their appearance varies greatly, from the well-differentiated forms, similar with haemangiomas, to low differentiated forms- heavy to differentiate from the carcinomas or achromatic melanomas [3].
Angiosarcoma affecting oral cavity especially gingiva is particularly rare; there are only a few case reports and clinical review series in the literature [4]. Therefore, this case reports an epulis-like angiosarcoma of the anterior gingiva of mandible.
Angiosarcomas seen in oral cavity may occur in a range of tissues, for instance oral soft tissue, minor salivary glands and bones. Fanburg-Smith et al., in his review reported 22 cases of primary angiosarcoma seen in oral cavity and salivary glands. Among the cases nine were in the tongue, four in the parotid gland, four in the lip, three in the submandibular gland and one case in the palate [5].
A review of the English-language literature on oral angiosarcoma involving gingiva revealed only 16 cases with detailed histopathological confirmation were found. The clinical features, treatment and prognosis of these previously reported cases, together with the current case, is summarized in [Table/Fig-8] [1,3–18].
A review of clinical features, treatment and prognosis of angiosarcoma involving primarily gingiva that was previously reported, together with the present case.
| Sl. No | Author | Year | Age/ Sex | Location | PrimarySymptoms andSigns | Clinical findings | Treatment | Follow-up |
|---|
| 1. | Henny [6] | 1949 | 3mo/M | Anterior part of right maxilla | A small lump in anterior partof the right maxilla for onemonth | Firm, well-circumscribed mass with extension posteriorly to the palate and laterally to the cheek | Initial Incision Later:Electorocaguation | No recurrenceafter 2 yearsand 3 month |
| 2. | Blake and Blake [7] | 1956 | 26y/M | First molar areaof leftmandible | A lesion on the ridge of firstmolar area in the leftmandible no pain for onemonth | A soft tissue mass of thefirst molar area in theleft mandible lobularin appearance, roundin shape, red in colour | Initial: Incision Later: "Removal | No recurrenceafter 2 yearsand 4 mo |
| 3. | Quinn et al., [8] | 1970 | 65 y/M | Maxillary andmandiblargingiva | Multiple lesionsin the oralcavity for 1month | Multiple pedunculatedsuperficially ulceratedlarge hemorrhagicfriable lesion in the gingiva, painless | Excision, Radiotherapy | Died after 1 mo and 3Weeks (unknown) |
| 4. | Albright et al., [9] | 1970 | 34 y/M | Anterior part ofrightmandible | A gingival massin the rightmandible for three month | An elevated hyperemic lobulated tumour on the lingual gingiva between themandiblar rightcanine and premolar teeth | Initial: excision Later: wide removal | No recurrence after 6 months |
| 5. | Piscioli et al., [10] | 1986 | 86 y/F | Gingiva of theleftmandibular molar area | A gingival massfor one week | A soft hemorrhagicnodule on the gingival of left mandibular molar area | Excision | Died after 1 month (heart failure) |
| 6. | Carr and Green [11] | 1986 | 66 y/M | Right maxillarygingiva | Bleeding from the gingival for 10 days | A large rubbery friablehemorrhagic mass on a broad base arising from the edentulous alveolus between the upper right canine and second molar teeth | Unknown | Died (metastases) |
| 7. | Kashima et al., [12] | 1994 | 39 y/M | Anterior part ofrightmandible | Pain for 10 months | Ulcer between the lowerright central inclsorand the right lateral incisor | Mandibulectomy | Died after 3 years and 1 mo(metastasis) |
| 8. | Kashima et al., [12] | 1994 | 7 y/F | Left mandible | A painless mass for one month | Mass between the lowerleft lateral incisor andfirst molar teeth, dark violet in colour | Initial: Excision Later:Mandibulectmy | Died after 1 year and 1 month(metastasis) |
| 9. | Margiotta et al., [13] | 1994 | 62 y/M | Right mandible | A mass in therightmandible | An ovoid, sessile, ill-definedmass, painless | Excision | Unknown |
| 10. | Muffoz et al., [14] | 1998 | 68 y/M | Right mandible | A mass in the right retromolartrigone for one week | A non-ulcerated sessile slightly painful massin the right retromolartrigone, brown in colour | Partial mandibulectomy | Died(recurrence) |
| 11. | Abdullah et al., [15] | 2000 | 60 y/F | Mandibluargingiva | A slight elevated reddish-blue nodule in the oral cavity | A reddish-blue nodular mass on the lowerAnterior gingiva | Refusal | Unknown |
| 12. | Florescu M [3] | 2005 | 70 y/M | Alveolar crest ofmandible | The tumour was soft, white-gray colour, withdisseminated areas of hemorrhage | A nodular mass, with undefined limits and maximum diameter of 4 cm. | Unknown | Unknown |
| 13. | Uchiyama et al., [4] | 2009 | 59 y/M | Left maxilla | Bleeding andswelling ofthe leftmaxillarygingiva for few months | A regular mass aroundthe left upper molararea, violet in color | Initial: maxillotomy and chemotherapy.Later: boron neutron therapy and lymphokineactivated killer cellstreatment | No recurrenceafter 3 y |
| 14. | Terada T [1] | 2011 | 77y/F | Mandibular gingivaposterior to the front tooth | - | Polypoid reddish mass measuring 1.5 x 1.5 x 1cm in the mandibular gingival posterior to the front tooth | Radical operation | Unknown |
| 15. | Sumida T [17] | 2012 | 55y/F | Anterior region of themandibular gingival | The epulis was a soft exophytic nodular mass, withwell defined limits and a maximum diameter of 10 mm | The tumour was soft, whitepink in colour, with easy bleeding. | The operation was performed with about a20-mm surgical margin that was negative for tumour invasion. | 4-year follow-up, nometastatic lesions have been found |
| 16. | Aditya A [18] | 2012 | 75y/F | Gingival growth in the right maxillary region | Pain waspresent for the last 15 days; however, she could not indicate the onset and duration of the growth. | A lobulated, sessile mass involvingthe gingival and alveolar mucosa in the maxillary right molar region. The mass was 3 cm, soft to firm inconsistency and slightly tender, with moderate bleeding. | The patient declined any therapy | Unknown |
| 17. | Present case | 2016 | 30 y/F | Mandibular anterior gingiva | The growth started 2 months ago, as a small sessile painless growth progressively increased to attain the size of 3×3 cm | soft sessile growth arising from the labial gingiva in relation to 31 and 41 on the labial aspect extending distal to 32 | The operation was performed with about a 20-mm surgical margin that was negative for tumor invasion | 2 years follow-up, no recurrence and metastatic lesions were found. |
Histopathologically, there can be varied appearance, from well differentiated forms with formation of vessels lined of atypical endothelia, to low differentiated forms, composed by proliferation of epithelial-like cells, with polymorphous, hyper chromatic nuclei, with frequent atypical mitosis [1].
Three main patterns of growth are seen in angiosarcomas i.e., a spindle shaped cell pattern, an angiomatous pattern with epithelioid cell features and an undifferentiated or solid pattern. All these patterns can be seen in the same tumour. In the present case of angiosarcoma, there was existence of a vascular tumour despite the relatively benign vascular proliferation. The neoplastic cells seen were round to polygonal in shape, tall, with intense eosinophilic cytoplasm and round to ovoid pleopmorphic hyperchromatic nuclei with numerous mitotic figures [6].
According to the definition, the tumour cell of angiosarcoma has to show some degree of vascular differentiation, either seen at the light microscopic level or by immunohistochemical marker postivity. Earlier, positivity to Factor VIII-related antigen and lectins helped to aid in the diagnosis. Recently, expression of another antigen, CD31, has been used as a specific diagnostic marker for this malignancy [7,8].
Florescu et al., reported that utilization of CD31 and CD34 is sufficient for the identification of the majority of angiosarcomas, including the low differentiated forms and is the best means to deal with the diagnosis of these vascular neoplasms [3]. Thus CD31, CD34 with factor related antigen was analysed in the present case.
In the present case, the intense membrane-based uniform positivity of lesional cells was seen on CD31 and CD34 showed focal moderate cytoplasmic staining, together with a Factor VIII related antigen which was strong diffuse cytoplasmic staining of tumour cells of angiosarcoma. Positivity for these markers confirms the endothelial phenotype that is found in malignant vascular tumours.
Angiosarcomas seen in elderly patients, are very destructive, have a propensity to recur locally, spread extensive, and have an elevated rate of lymph node and systemic metastases, with tumour related-death. There is an universal agreement that the occasion of the tumor detection can be one of the prognostic factors of angiosarcoma of the oral cavity. However, studies showed that prognosis is not influenced by the histologic grade and mitotic activity [7]. The present case was diagnosed at an early age of 30 years and also showed recurrence after complete surgical excision. A two years follow-up showed no second recurrence.
Conclusion
Angiosarcoma is a rapidly progressing malignancy that rarely affects the oral and pharyngeal mucosa. However this is the 17th case report in the literature arising in anterior mandibular gingiva. The generally advanced stage of the tumor at initial diagnosis leads to a poorer survival of patients with mucosal angiosarcomas as compared with patients seen in cutaneous angiosarcomas. Tumor size and metastases are related to the prognosis of the disease. Early detection, therefore, is important. Published cases and recognition of new ones may be helpful in establishing timely treatment and better prognosis of this rare pathology.
[1]. Terada T, Angiosarcoma of the mandibular gingivalInt J Clin Exp Pathol 2011 4(8):791-93. [Google Scholar]
[2]. Naikmasur VG, Sattur AP, Bhowmik B, Angiosarcoma of the Soft Palate - A Case ReportJ Cytol Histol 2015 S3(1):1-4. [Google Scholar]
[3]. Florescu M, Simionescu C, Margaritescu C, Georgescu CV, Gingival angiosarcoma: histopathologic and immunohistochemical studyRom J Morphol Embryol 2005 46:57-61. [Google Scholar]
[4]. Uchiyama Y, Murakami S, Kishino M, Furukawa S, A case report of primary gingival angiosarcomaOral Surg Oral Med Oral Pathol Oral Radiol Endod 2009 108:e17-21. [Google Scholar]
[5]. Fanburg-Smith JC, Furlong MA, Childers EL, Oral and salivary gland angiosarcoma: a clinicopathologic study of 29 casesMod Pathol 2005 16:263-71. [Google Scholar]
[6]. Henny FA, Angiosarcoma of the maxilla in a 3 month old infant: report of caseJ Oral Surg 1949 7:250-52. [Google Scholar]
[7]. Blake H, Blake FS, AngiosarcomaL report of a caseOral Surg Oral Med Oral Pathol 1956 9:821-25. [Google Scholar]
[8]. Quinn JH, McConnell HA, Leonard GL, Multifocal Angiosarcoma of the gingiva: report of caseJ Oral Surg 1970 28:215-17. [Google Scholar]
[9]. Albright CR, Shelton DW, Vatral JJ, Hobin FC, Angiosarcoma of the gingiva: report of caseJ Oral Surg 1970 28:913-17. [Google Scholar]
[10]. Piscioli F, Leonardi E, Scappini P, Cristofolini M, Primary angiosarcoma of the gingiva. Case report with immunohistochemical studyAm J Dermatopathol 1986 8:430-35. [Google Scholar]
[11]. Carr RJ, Green DM, Oral presentation of disseminated angiosarcomaBr J Oral Maxillofac Surg 1986 24:277-85. [Google Scholar]
[12]. Kashima K, Igakura Y, Komura M, Hamada M, Arima R, Sakoda S, Three gingival tumors derived from vascular endothelial cells: a case of hemangioendothelioma and two cases of angiosarcomaNihon Koku Shuyo Gakkaishi 1994 6:251-61. [Google Scholar]
[13]. Margiotta V, Florena AM, Giuliana G, Primary angiosarcoma of the alveolar mucosa in a haemodialysis patient: case report and discussionJ Oral Pathol Med 1994 23:429-31. [Google Scholar]
[14]. Muñoz M, Monje F, Alonso del Hoyo JR, Martín-Granizo R, Oral angiosarcoma misdiagnosed as a pyogenic granulomaJ Oral Maxillofac Surg 1998 56:488-91. [Google Scholar]
[15]. Abdullah BH, Yahya HI, Talabani NA, Alash NI, Mirza KB, Gingival and cutaneous angiosarcomaJ Oral Pathol Med 2000 29:410-12. [Google Scholar]
[16]. Loudon JA, Billy ML, DeYoung BR, Allen CM, Angiosarcoma of the mandible: a case report and review of the literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2000 89:471-76. [Google Scholar]
[17]. Sumida T, Murase R, Fujita Y, Ishikawa A, Hamakawa H, Epulis-like gingival angiosarcoma of the mandible: a case reportInt J Clin Exp Pathol 2012 5(8):830-33. [Google Scholar]
[18]. Aditya A, Lele S, A nodular growth on maxillary gingivaIndian J Dent Res 2012 23:116-19. [Google Scholar]