Fetal MR Imaging Analysis of Sirenomelia with Clinico Radiographic Correlation: A Case Report
Madhavi Nori1, Raghavendra G. Prasad2, Arvind K Reddy3, Sandeep Reddy Cheguri4
1 Associate Professor, Department of Radiology, Deccan College of Medical Sciences, Hydearbad, India.
2 Professor, Department of Pediatric Surgery, PEH, Deccan College of Medical Sciences, Hyderabad, India.
3 Junior Resident, Department of Radiology, PEH, Deccan College of Medical Sciences, Hyderabad, India.
4 Junior Resident, Department of Radiology, PEH, Deccan College of Medical Sciences, Hyderabad, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Madhavi Nori, Associate Professor, Department of Radiology, PEH, Deccan College of Medical Sciences, Hyderabad-500 002, India.
E-mail: madhavi_dr@hotmail.com
Sirenomelia is a social curiosity, a medical and diagnostic challenge prenatally compounded by varied diagnostic difficulties. Prenatal diagnosis of sirenomelia was and continues to be a challenge although von klippel et al., described a case at 10 weeks of gestational age. However, they needed a second imaging at 12th week for confirmation. First trimester or early second trimester anatomic survey on ultrasound and MRI is accurate for the diagnosis thereby avoiding unnecessary complex pregnancy. We report a case of second trimester diagnosed sirenomelia, with detailed analysis of image findings on ultrasound and fetal MRI.
Case Report
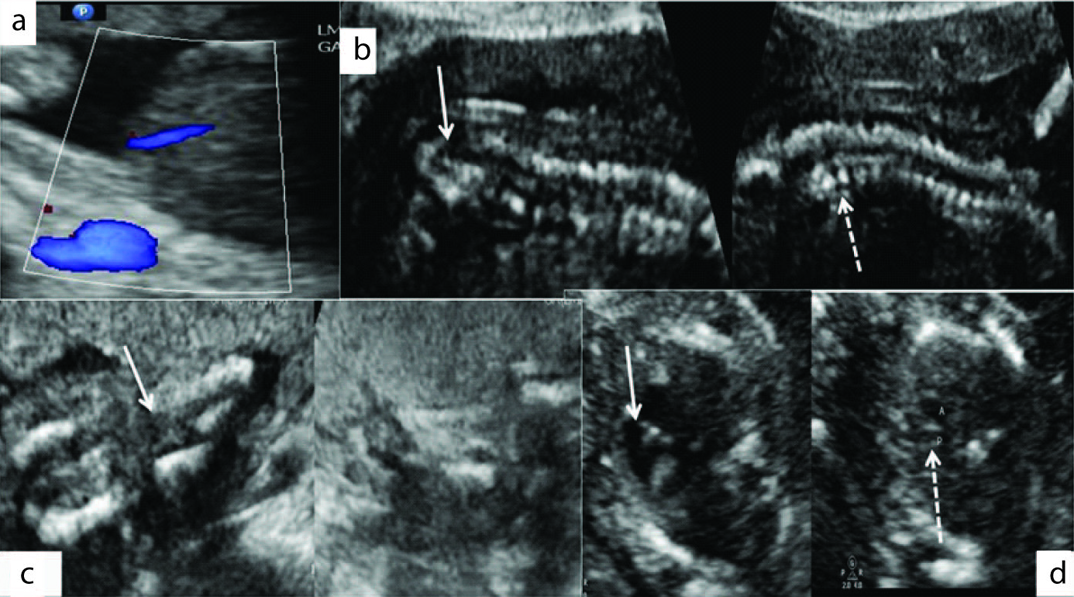
A 27-year-old, primi, had a early pregnancy scan at 7 weeks LMP showing concordant US biometry (CRL). There was no personal or family history for diabetes mellitus. Targetted Imaging for Fetal Anomalies (TIFFA) performed during this pregnancy at 20 weeks GA revealed small for gestational age fetus corresponding to fetal size of 17 weeks GA with anhydramnios. Colour Doppler survey along anterior abdominal wall revealed single umbilical artery coursing along right side. Aortic bifurcation was not present. Both kidneys and urinary bladder were not visualized [Table/Fig-1a]. In addition the spine showed deformity in the lower half with absent sacral tapering and multiple hemi vertebrae [Table/Fig-1b]. The limb survey revealed convergent femoral bones not changing with time with two tibial bones within a single soft tissue and muscular compartment with absence of fibular bones in the legs ending into feet which were fused and non descript [Table/Fig-1c]. Fetal heart survey revealed asymmetry in chamber sizes (right ventricular dilatation) with abnormal three vessel view showing narrow pulmonary artery [Table/Fig-1d]. Presumptive diagnosis of sirenomelia was made.
USG revealed SGA fetus corresponding to 17 weeks size with no measurable pocket of amniotic fluid. UB was not visualized. Colour Doppler revealed single umbilical artery (1a). Spine showed absent sacral tapering and multiple hemi vertebrae (1b). Limb survey revealed convergent femoral bones with two tibial bones within a single soft tissue compartment ending into feet which were fused and nondescript (1c). Fetal thorax revealed asymmetry in chambers with right ventricular dilatation and narrow pulmonary artery (1d).
In view of multisystem involvement, Fetal MR was performed 1 week later to further investigate the visceral anomalies to assist with prognostication and further counselling.
T2-weighted Half-Fourier Acquisition Single-Shot Turbo Spin-Echo (HASTE) sequences were obtained in the axial, coronal and sagittal planes with respect to the fetus. Sequences were monitored in real time and manipulated to determine optimal imaging planes during the scan, as fetal orientation is unpredictable and often changes during acquisitions. In addition to the standard orthogonal planes, oblique planes were acquired for demonstrating the relationship to surrounding structures.
Liquor was significantly reduced rendering the suboptimal image quality and hence the MR fetal anatomy was compared with gestational age matched normal fetus. Diagnosis of sirenomelia sequence was confirmed based on the following findings.
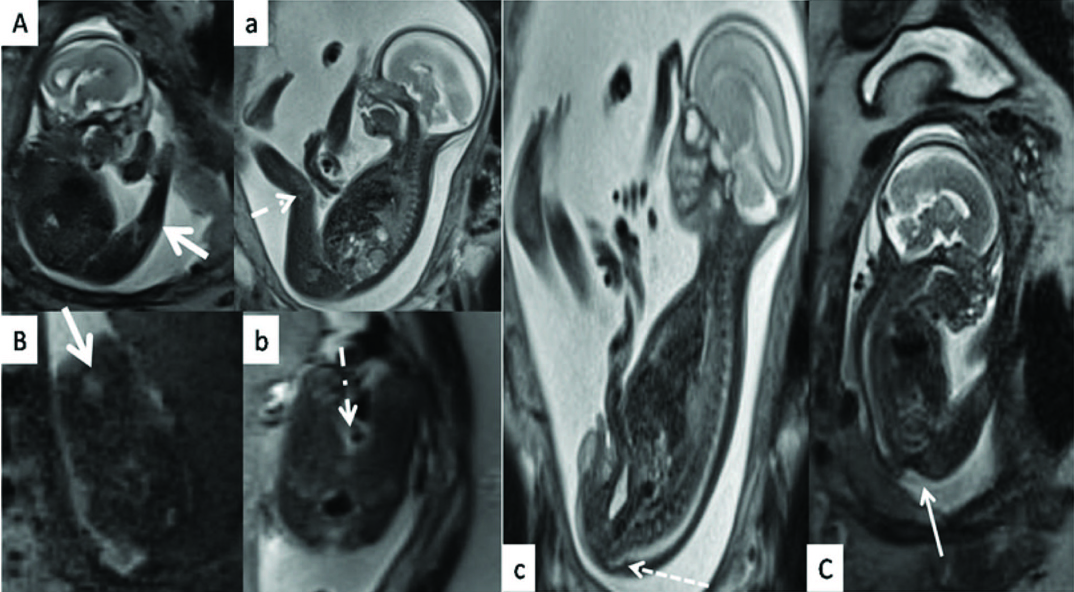
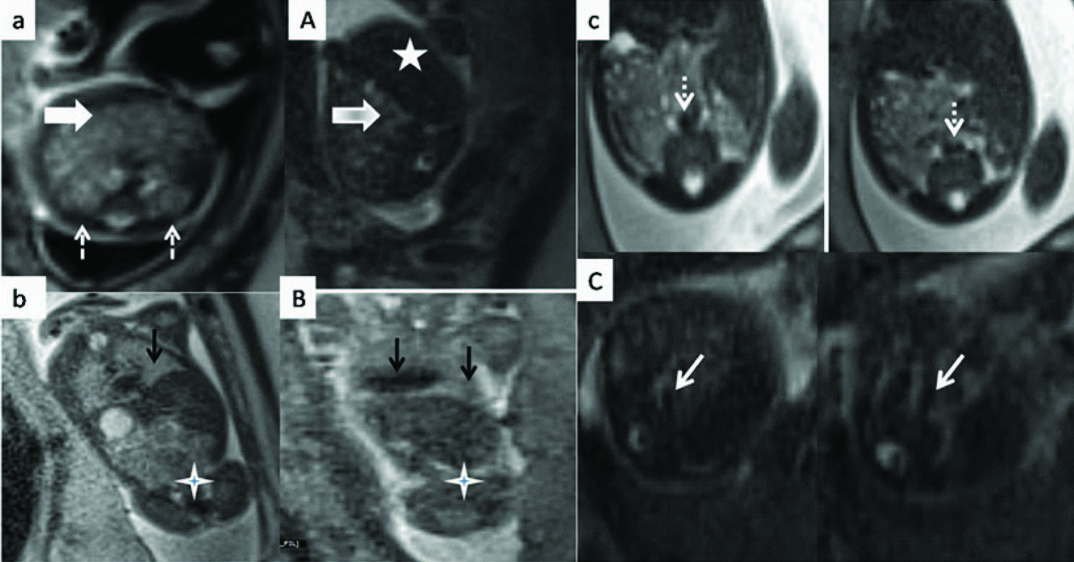
Fused lower extremities, hyperextension at the knee, nondescript feet [Table/Fig-2a]; Absence of the soft tissue cleft /separation [Table/Fig-2b]; Absent sacral tapering with prominent gluteal concavity [Table/Fig-2c]; absent kidneys with relative paucity of small bowel loops and apparent prominent liver [Table/Fig-3a]; Cardiomegaly with hypo plastic lungs and absent large bowel on coronal section [Table/Fig-3b]. Abdominal aorta showed aberrant course anteriorly towards the umbilicus without bifurcation [Table/Fig-3c]. Upper limbs were not detailed, No intracranial anomalies were present.
MRI of aberrant lower extremity and spine(Upper case) compared with normal age matched fetus (lower case): 2A) Fused lower extremities, hyperextension at the knee (arrow). Feet are nondescript. Normal separation with concavity at the knee (dashed arrow) (2a). Absence of the soft tissue cleft /separation (2B) between the thighs as compared with normal cleft (2b). Sacral tapering is absent with prominent gluteal concavity (arrow) (2C) in contrast to the normal sacral tapering with convex gluteal contour (dashed arrow) (2c).
MRI of abdomen (Upper case) compared with normal age matched fetus(lower case) Absent kidneys with relative paucity of small bowel loops (arrow) and apparent prominent liver(Star) (3A). Normal kidneys (dashed arrows) and small bowel loops(3a) (arrow). (3B)Cardiomegaly with hypo plastic lungs (arrows) and absent large bowel (star) on coronal. Terminal large bowel in the midline (3b) (star). Abdominal aorta (3C) shows aberrant course anteriorly towards the umbilicus without bifurcation (arrows), normal aorta and its branching (3c)(dashed arrows).
Multiple anomalies incompatible with life and poor fetal prognosis was explained and the couple opted for termination of pregnancy at 21-22 weeks. Mother did not have any postpartum complications. Autopsy was declined.
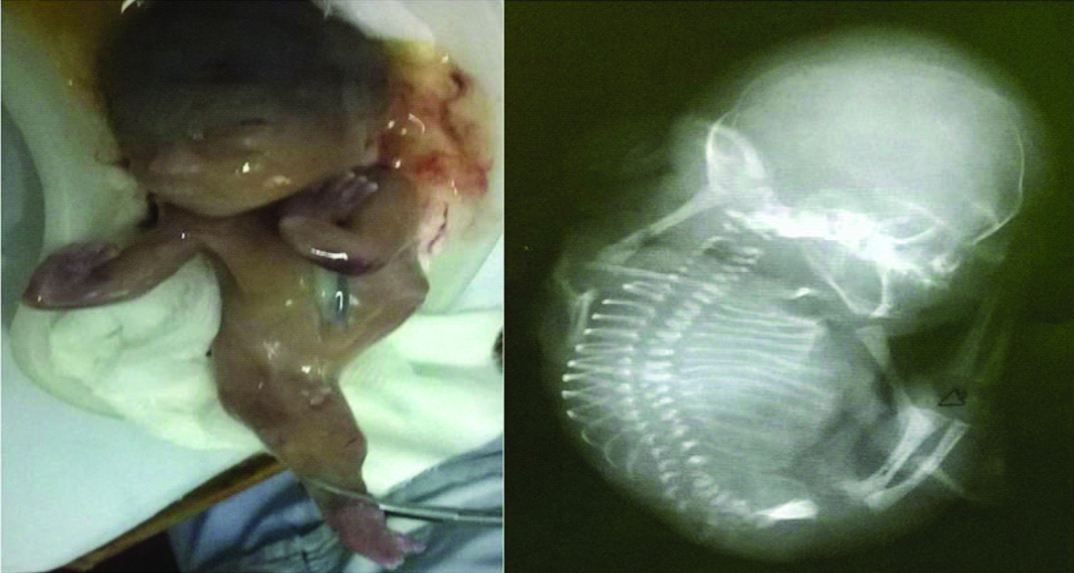
Clinical photograph [Table/Fig-4a] revealed potters facies, bilateral club hands with syndactyly, small pelvis and male external genitalia. Fused lower limbs, feet fused posteriorly and divergent anteriorly resembling the fins of a fish. Radiograph of the abortus in lateral view [Table/Fig-4b]. Axial skeleton revealed hypoplasia of iliac bones, sacral agenesis, and multiple vertebral segmentation defects. Appendicular skeleton revealed fusion of both lower limbs in midline with two femora and tibia and absent fibulae. Upper limbs revealed absent radius bilaterally with club hands.
Clinical photograph (4a) reveals potters facies, bilateral club hands with syndactyly, small pelvis and male external genitalia. Fused lower limbs, feet fused posteriorly and divergent anteriorly resembling the fins of a fish. Radiograph of the abortus in lateral view (4b). Axial skeleton reveals hypoplasia of iliac bones, sacral agenesis, multiple vertebral segmentation defects. Appendicular skeleton reveals fusion of both lower limbs in midline with two femora and tibia and absent fibulae. Upper limbs reveal absent radius bilaterally with club hands.
Discussion
Sirenomelia is a rare and lethal congenital anomaly in most of the countries and was first described in 16th century by Rocheus and Palfyn [1]. The various hypotheses put forth to explain sirenomelia represents inadequacy of each of them [2,3]. Sirenomelia has been classified based on number of factors such as limbs, bones, types of vasculature; associated anomalies [1–6]. This syndrome is not associated with chromosomal anomalies [7]. Hence chromosomal studies were not done in the index case.
As propagated by Stevenson [6], intrauterine vascular accident seems to explain most commonly associated abrupt vascular development of great vessels of abdomen with variable multiple organ system involvement, most consistent being single aberrant umbilical artery, malformation of urinary tract, musculoskeletal system, lower gastrointestinal tract and external genitalia.
The index case shows sirenomelia (legs fused by the skin with separate bones) in fetal position at 21 weeks with anhydramnios with involvement of vascular, genitourinary, sketelal, gastrointestinal, pulmonary and cardiac systems and was depicted based on ultrasound and MR findings.
Wide range of external morphological abnormalities was reported like absent anus, absent/ambiguous genitals, cord anomalies, facial anomalies [1–7]. Prominent epicanthal folds, low set abnormal ears as in Potters facies with bilateral inguinal gonads with penis was seen in the index case.
Prenatal diagnosis has been made by ultrasound mostly during the late second and third trimesters by ultrasound [2–4] but it is usually hampered by anhydramnios secondary to renal agenesis or dysgenesis. Prenatal Magnetic Resonance Imaging (MRI) complements the ultrasound findings and allows detailed exploration of visceral anatomy, external contoural abnormalities of the fetus owing to high soft tissue contrast independent of liquor. Various MR signs are described in literature [1,8,9].
In our case, ultrasound provided greater detail on sacral agenesis, Segmentation anomalies in lumbar spine, fused lower limbs, however the external morphometric anomalies resulting from skeletal system involvement were better detailed on fetal MRI. Visceral anomalies seen on MRI were non visualization of large bowel, paucity of small bowel loops and large liver extending to left.
In our case, the external gluteal concavity and the single large abdominal vessel coursing ventrally into the cord without branching into iliac vessels, which was pathognomic for prenatal diagnosis of this anomaly, was seen for the first time on fetal MRI. Additional abnormalities seen in our case postnatally were absent radius with club hands and syndactyly.
First trimester diagnosis is rarely reported [1,7] because though diagnostic ability of USG is very high owing to normal amniotic fluid, detailed anatomy of abdominal structures is less reliable on ultrasound and even more on MRI owing to small size of fetus in first trimester. Boopathy et al., reported continuous skin line on high resolution ultrasound as diagnostic criteria for the identification of fused limbs in first trimester [10]. However, in our case the patient reported to us in the second trimester.
Sirenomelics are usually fatal and die immediately after birth [5]. Reddy et al., described a case whom they operated for colonic atresia and baby died on 12th day [4]. Such futile cost incurring invasive procedures can be avoided by antenatal diagnosis.
Due to its rarity and varied presentation in the literature, sirenomelia sequence is an appropriate name to be used as seen in our case.
Conclusion
To conclude, we recommend that first trimester or early second trimester anatomic survey on ultrasound and MRI is accurate for the diagnosis thereby avoiding unnecessary complex pregnancy.
[1]. Van Keirsbilck J, Cannie M, Robrechts C, de Ravel T, Dymarkowski S, Van den Bosch T, First trimester diagnosis of sirenomeliaPrenatal diagnosis 2006 26(8):684-88. [Google Scholar]
[2]. Fadhlaoui A, Khrouf M, Gaigi S, Zhioua F, Chaker A, The sirenomelia sequence: a case historyClinical Medicine Insights. Case reports 2010 3:41 [Google Scholar]
[3]. Sahu L, Singh S, Gandhi G, Agarwal K, Sirenomelia: A case report with literature reviewInt J Reprod Contracept Obstet Gynecol 2013 2(3):430-32. [Google Scholar]
[4]. Reddy KR, Srinivas S, Kumar S, Reddy S, Prasad H, Irfan GM, Sirenomelia: A rare presentationJournal of Neonatal Surgery 2012 1(1) [Google Scholar]
[5]. Kshirsagar VY, Ahmed M, Colaco SM, Sirenomelia apus: A rare deformityJournal of Clinical Neonatology 2012 1(3):146 [Google Scholar]
[6]. Stevenson RE, Jones KL, Phelan MC, Jones MC, Barr M, Clericuzio C, Vascular steal: the pathogenetic mechanism producing sirenomelia and associated defects of the viscera and soft tissuesPediatrics 1986 78(3):451-57. [Google Scholar]
[7]. Akbayir O, Gungorduk K, Sudolmus S, Gulkilik A, Ark C, First trimester diagnosis of sirenomelia: a case report and review of the literatureArchives of Gynecology and Obstetrics 2008 278(6):589-92. [Google Scholar]
[8]. Sawhney S, Jain R, Meka N, Sirenomelia: MRI appearanceJournal of postgraduate medicine 2006 52(3):219-20. [Google Scholar]
[9]. Dong SZ, Zhu M, Mao JP, Zhong YM, Gu XH, Diagnosis of abnormalities of fetus with oligohydramnios by MRI [J]Journal of China Clinic Medical Imaging 2008 1:017 [Google Scholar]
[10]. Vijayaraghavan SB, Amudha AP, High-resolution sonographic diagnosis of sirenomeliaJournal of Ultrasound in Medicine 2006 25(4):555-57. [Google Scholar]