Asthma is a chronic inflammatory disorder of the airways associated with increased airway hyper-responsiveness, recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night/early morning [1]. Asthma causes limitations of daily activities, loss of work days, lung function impairment, reduced quality of life and an adverse socioeconomic burden. The prevalence of asthma in India is estimated to be 2.05% among those aged >15 years along with an estimated national burden of 18 million asthmatics [2].
Inadequate control of asthma has shown to hamper quality of life and leads to severe economic burden to the patient and health care establishments. Uncontrolled asthma can result in death also. Furthermore, in poorly controlled conditions, there is a risk of treatment-related complications. Hence, adequate control is the goal of asthma management. The measurement of asthma control includes periodic assessment of clinical and functional manifestations such as clinical symptoms and signs, use of rescue medication, activity limitation and pulmonary function [3].
Guidelines have been developed globally to measure the asthma control combining all of the above parameters accepted by physicians’ world over. Recent developments have resulted in formation of the Asthma Control Test (ACT) Questionnaire. However, despite guidelines and new therapeutic approaches many asthmatic patients do not achieve an acceptable asthma control [4].
Philippe LB et al., described a new method to quantify asthma control based on the percentage scores obtained with patient’s self-evaluation of asthma control and a validated Mini Asthma Quality of Life (MAQOL) questionnaire. Assessment of percentage control for symptoms, baseline expiratory flows and airway inflammation from induced sputum eosinophil count was possible in this study [5].
Not many studies have been conducted in India on measuring asthma control using objective parameters. The aim of the present study was to assess asthma control using modified MAQOL developed by Philippe LB et al., [5]. We also identified the probable risk factors that contributed to poor asthma control.
Materials and Methods
This cross-sectional study was conducted on patients attending the outpatient of Pulmonary Medicine at Vydehi Institute of Medical Sciences and Research Centre, Bangalore from June 2012 to December 2012. The study was conducted after obtaining Institutional Ethics Committee approval. Sixty patients of bronchial asthma were screened for the following inclusion and exclusion criteria:
Inclusion Criteria
Patients who were diagnosed with bronchial asthma as per ICD 10 guidelines, aged 18-55 years, under treatment for at least six months and patients using an inhaled corticosteroid and/or oral or inhaled β2 agonist and/oral montelukast were included in the study.
Exclusion Criteria
Patients with features of chronic obstructive pulmonary disorder, acute and chronic respiratory infections, chronic smokers and patients on systemic steroid therapy in the preceding 2 weeks were excluded from the study.
Those who fulfilled the criteria and volunteered to participate by giving a written informed consent were enrolled in the study. Detailed history was taken with the help of a modified questionnaire from the patients and they were assessed for asthma control with the MAQOL [Table/Fig-1].
Asthma control scoring system.
| Clinical Assessment |
| Symptoms score | 25% | 20% | 15% | 10% | 5% | Total score |
| Diurnal symptoms | None | <4 times/week | 4-7 times/week | >once/day | Severe | 15 |
| Nocturnal symptoms | None | <1 night/week | 1-3 nights/week | 4-7 nights/week | Severe | 20 |
| Beta-2 agonist on demand* | None | <4 doses/week | 4-7 times/week | >1 dose/day | >4 doses/day | 15 |
| Physical activity | None | Very little limitation | Some limitation | Moderate limitation | Severe limitation | 15 |
| Total score-65 |
| Physiological Assessment |
| Score (%) ** | 100 | 80 | 60 | 40 | 20 | Total score |
| FEV1 or PEF (% of predicted or optimal value | >90% | 80-89% | 70-79% | 60-69% | <60% | 60% |
| PEF variation | <10%>5 days/week | <10%>5 days/week | 10-15%>5 days/week | 16-25%>5 days/week | >25%>5 days/week | Not done |
| Inflammatory Assessment |
| Score (%) | 100 | 80 | 60 | 40 | 20 | Total score |
| Airway eosinophilia (%) | 0 | 2 or less | >2-5 | 5.1-8 | >8 | 60% |
*-excluding 1dose/day before exercise
**-score divided by 2 if the two criteria are used.
The asthma global score was calculated for each patient based on the following three parameters:
Respiratory symptoms and need for rescue inhalers.
Patient’s best measure of FEV1 in percentage of predicted value, measured with a spirometry machine and PEFR.
The percentage eosinophil count of induced-sputum samples.
The different elements were quantified as mentioned in [Table/Fig-1] and a global score was determined by calculating the sum of the mean for these three different types.
The severity of symptoms namely wheeze, cough, breathlessness and tightness of chest were given a score in the following way: mild-1; moderate-2; and severe-3. Therefore, adding the individual symptom scores, 0 was considered as the best score and 12 was considered as the poor score. The following investigations were also done: forced expiratory volume in 1st second (FEV1)-predicted and observed, peak expiratory flow rate (PEFR), sputum eosinophils, haemoglobin, total count, differential count and serum IgE levels. A global score of <80% was considered as poor control.
Procedure for Sputum Eosinophil Count: Patients who complained of cough with expectoration were given a sputum cup and were asked to expectorate till at least 10 ml of sputum was obtained. In case the quantity of sputum was less, the patient was asked to forcefully expectorate till the required quantity was obtained. Patients who did not complain of any cough were given Levoasthalin nebulisation after which they were asked to expectorate till 10 ml of sputum was obtained. The eosinophils were counted at 40X magnification in a sputum smear stained with Leishman’s stain.
Evaluation of Risk Factors: The patients were enquired about the history of exposure for various factors that aggravated their symptoms in the last 15 days.
Statistical Analysis
Patient pool was categorised as poorly controlled (PC) with a global score of <80% and well controlled groups (WC) with a global score of >80%.
The proportion of patients under each factor in PC was compared with the WC with the help of descriptive statistics.
The mean global score, age, duration, severity, number of sputum eosinophils, technique of inhalation, awareness of asthma action plan and compliance in both the PC and the WC were compared by using unpaired students ‘t’-test.
Results
A total of 60 patients were screened of which 50 fulfilled the criteria. Majority of the patients were less than 50 years. There were more males than females. Asthma duration ranged from 1 year to greater than 10 years. More than half of the patients had severe asthma as shown in [Table/Fig-2].
| Factors | Number of Patients |
|---|
| 1-Age |
| 18-50 years | 43 |
| 51-65 years | 7 |
| 2-Sex |
| Males | 32 |
| Females | 18 |
| 3-Duration |
| <5 years | 13 |
| 5-10 years | 19 |
| >10 years | 18 |
| 4-Severity Score |
| 0-6 | 16 |
| 7-12 | 34 |
| 5-Smokers | 16 |
| 6-Alcoholics | 11 |
| 7-Family history of asthma | 25 |
Prescribed Treatment
Fourteen patients were prescribed inhaled budesonide and formoterol fumarate. Eight patients were prescribed inhaled salmeterol and fluticasone propionate. Twelve patients were prescribed oral montelukast and inhaled budesonide or fluticasone propionate. Four patients were prescribed oral deriphyllin and inhaled budesonide or fluticasone propionate. Three patients were prescribed oral deriphyllin and oral montelukast. Nine patients were prescribed inhaled salbutamol. The dose and duration prescribed were as per the standard protocols.
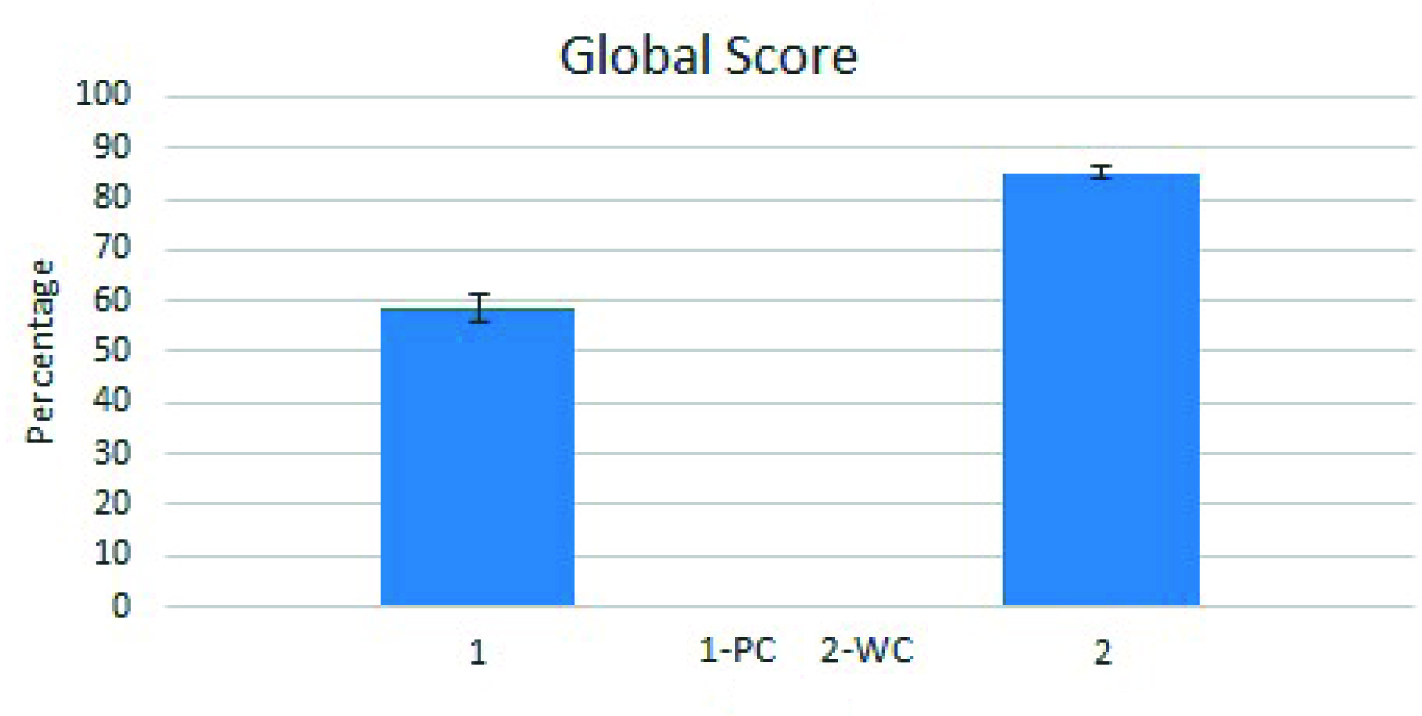
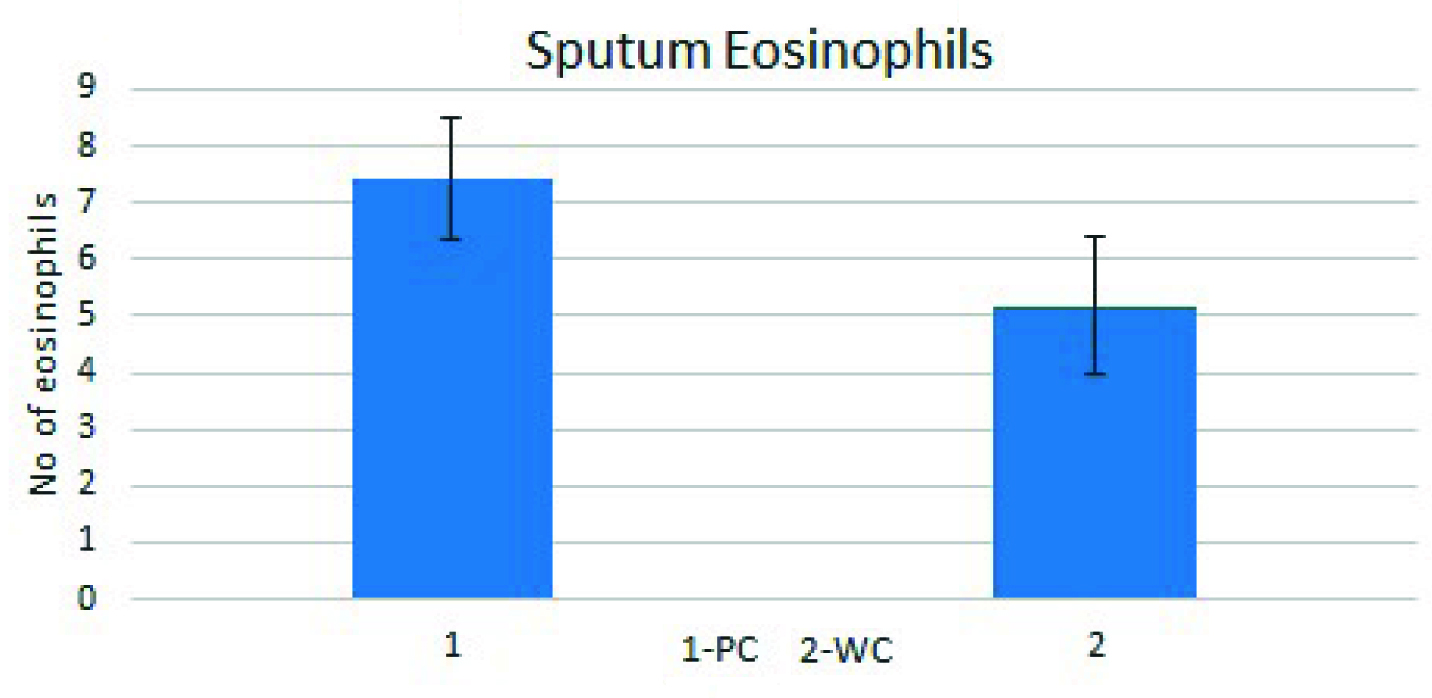
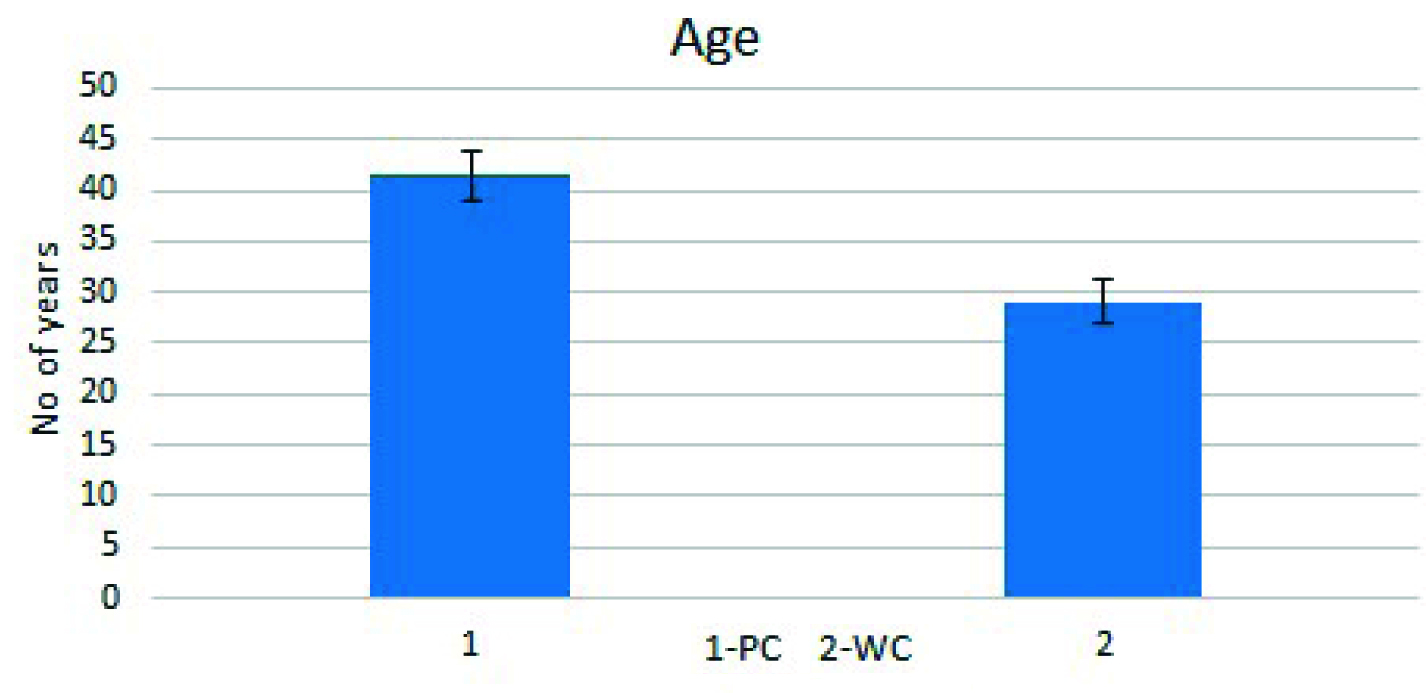
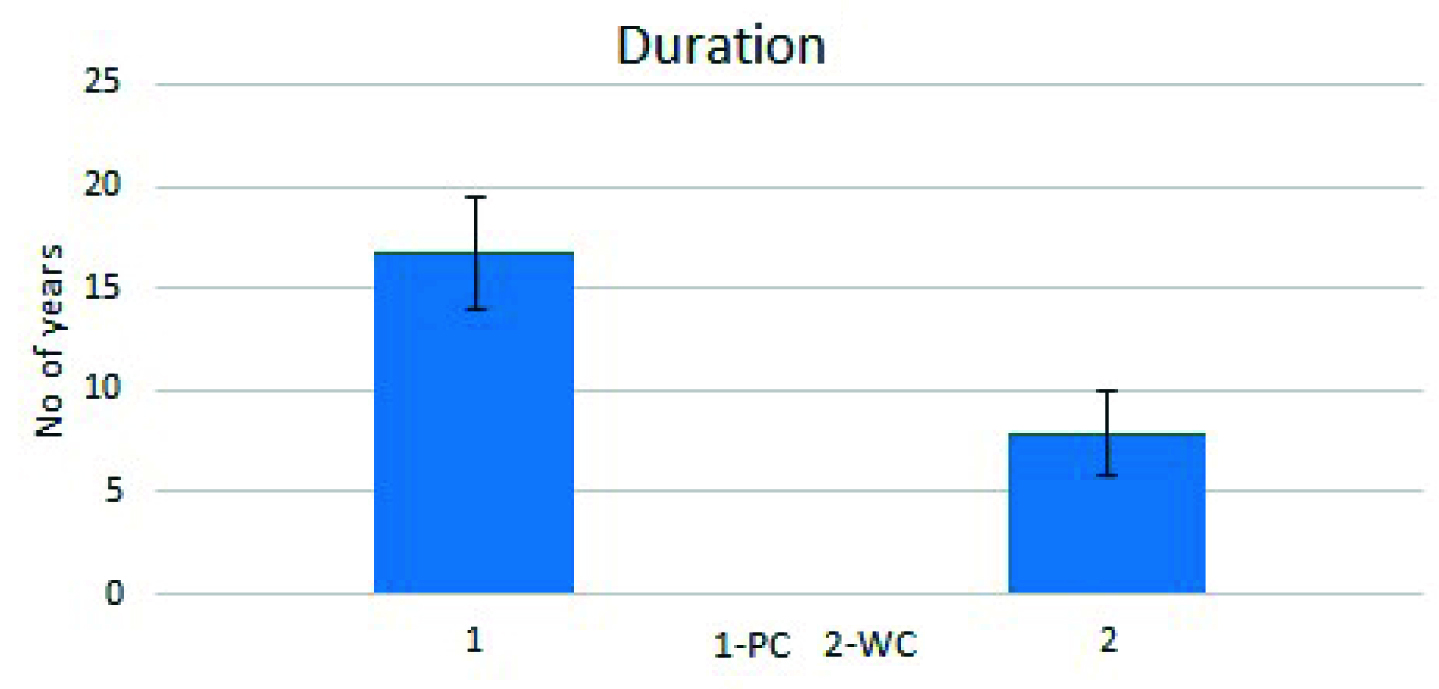
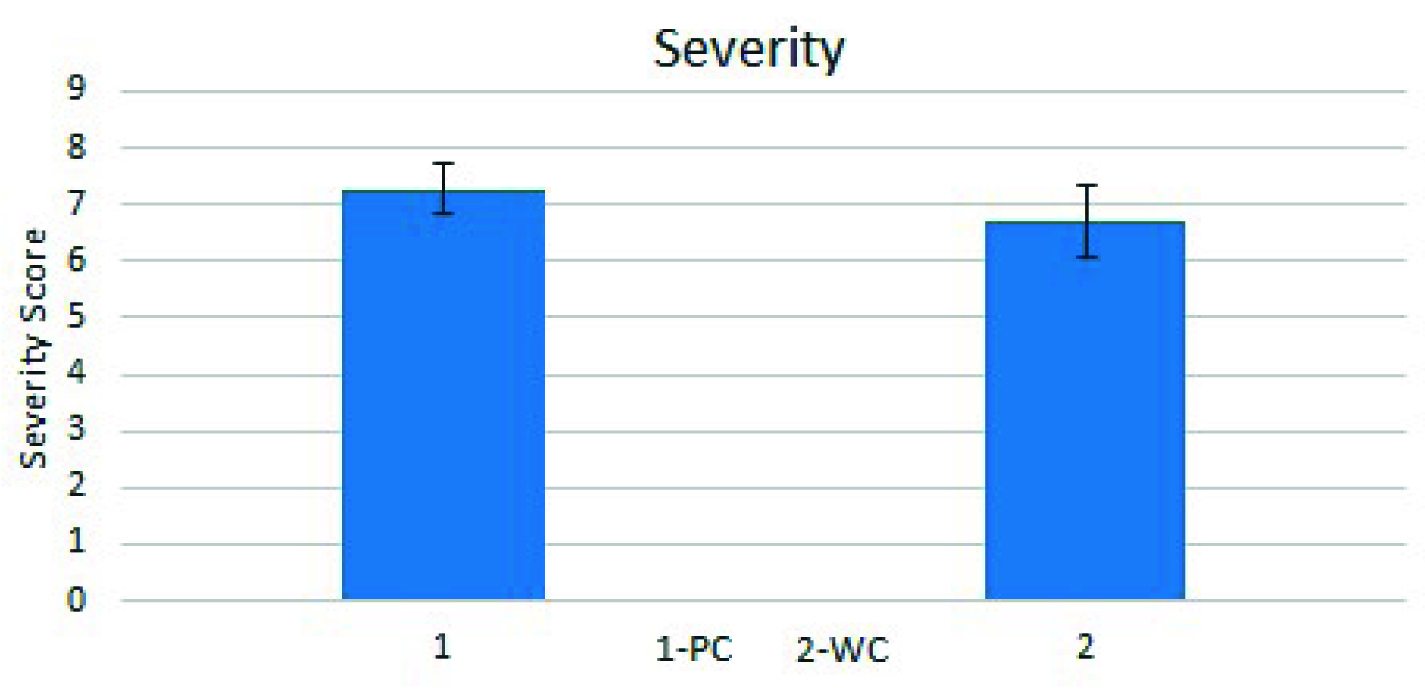
The study showed that 33 of the 50 patients (66%), had a global score of < 80% indicating Poor Control (PC), the remaining 17 patients (34%) were Well-Controlled (WC) with score of above 80%. The mean global asthma score in PC was 58.46 ± 2.881 vs 85.2 ± 1.19 in the WC group (p<0.05) [Table/Fig-3]. Mean sputum eosinophil count was 7.441 ± 1.081 in PC vs 5.176 ± 1.201in WC group (p<0.05) [Table/Fig-4]. The mean age in PC was 41.41 ± 2.413 vs 29.00 ± 2.157(p<0.05) in the WC group [Table/Fig-5]. The mean duration of asthma in PC was 16.76 ± 2.761 vs 7.882 ± 2.065 7.88 years in WC (p<0.05) [Table/Fig-6]. The severity score was 7.265 ± 0.4434 in PC vs 6.706 ± 0.64 in WC group [Table/Fig-7]. Eight (24.2%) patients in PC and six (35.2%) patients in WC were unaware of the treatment plan. One (3.03%) patient in PC group and three (17.6%) patients in WC were unaware of technique of inhalation. One (3.03%) patient in PC group and three (17.6%) patients in WC were non–compliant.
Assessment of asthma control.
Assessment of inflammation with sputum eosinophil count.
Factors contributing to asthma control-Age.
Factors contributing to asthma control-Duration.
Factors contributing to asthma control-Severity.
Precipitating Factors
In PC Group, the asthma attacks were precipitated by dust (96.9%), weather changes (78.7%), cold air (69.6%) and tobacco smoke (69.6%). In WC Group, dust (88.2%), weather changes (64.7%), cold air (76.4%) and pets (58.8%) accounted for most of the asthma attacks in majority of the patients.
Discussion
The present study was conducted to evaluate asthma control using MAQOL and to identify the factors contributing towards poor asthma control in patients on regular medication in an Indian population.
The study showed that 66% had poor control even on regular maintenance therapy. This result is in concurrence with the INSPIRE study done by Partridge MR et al., which was a multicentric study on 3415 adults prescribed regular maintenance therapy with inhaled corticosteroids or inhaled corticosteroids along with long-acting β2-agonists. Their study also showed that patients recognise deteriorating asthma control and adjusted their medication during episodes of worsening [6].
When poorly controlled, the first question is to assess the adequacy of prescription and patient compliance to treatment. Non-compliance to medication has shown an increased morbidity and mortality [7]. The answers to the questionnaire revealed that majority of the patients were fairly compliant to the prescribed medications in both the groups contrary to the reports in the literature that says that only a small proportion of patients with asthma regularly take medications as prescribed. The prescriptions were as per the standard protocols.
Independent studies have attributed inhaler mishandling, insufficient knowledge and inadequate compliance on the part of the patient for poor asthma control [8].
Melani S et al., conducted a study to evaluate the inhalation technique of a large sample of experienced outpatients referring to chest clinics to investigate the prevalence and the factors associated with inhaler misuse and to assess the relationship between inhalation technique and some clinical outcomes with the help of a validated questionnaire. The study showed that many patients on inhalers do not handle it appropriately as they were not educated about it. However, this was not the only reason for poor asthma control [8].
Similarly in our study, the majority of the patients followed the right technique of inhalation and hence did not emerge as a contributing factor for poor asthma control. However, the sample size is too small compared to study by Melani et al., to make the conclusion [8]. Patients in PC group had a longer duration of asthma (Mean: 17 years) compared to WC group (Mean: 7.8 years). Duration of asthma was a significant contributor to the poor control, probably because the long standing inflammation might have not responded to the medication. This result is in concurrence with a study on duration of asthma conducted by Cassino et al., which revealed that patients with long duration of asthma had a significant lower FEV1 per cent predicted than those with short duration and there is also an association between Functional Residual Capacity (FRC) and duration of asthma that was independent of the degree of airflow limitation. Their study suggested that longstanding asthma lead to irreversible airway changes and there may be parenchymal remodelling in the process [9].
It is also well known that patient awareness of asthma action plan would help in the proper use of inhalers and compliance. In our study majority of the patients in PC group (76%) were aware of asthma action plan therefore this was not a significant contributory factor.
Patients in PC group were of higher age (Mean: 42 years) compared to WC group (Mean: 29 years). It is observed that elderly subjects with longstanding asthma failed to achieve normal airflow after bronchodilator administration, in contrast to those with asthma of short duration. Therefore, higher the age poorer the asthma control indicating probably unresponsiveness to ongoing treatment [9].
More patients in the PC group had severe asthma. The severity score was higher in PC group (Mean score 7.3) as compared to WC group (Mean score 6.7), the probable reason being advancement in age.
The induction of sputum is a safe, non-invasive method of studying airway inflammation in asthma [10]. Eosinophilic infiltration is the most striking feature in airway inflammation which can be detected in induced sputum [11]. Hence, we adopted this method to evaluate the inflammation. Our study showed a higher eosinophil count in PC group compared to WC group indicating persistent inflammation. A comparative analysis is also done with other studies as shown in [Table/Fig-8] [12–15].
Comparison of our study with other studies.
| Other Studies | Present Study |
|---|
| In a study conducted by Mahdi Bijanzadeh et al., they concluded that asthma aggregates within families and is a complex multifactorial disease with the involvement of environment and genetic components. Autosomal recessive pattern of inheritance was prominent in asthma [12]. | In our study, 25 out of 50 patients had associated family history of bronchial asthma. Therefore, we cannot come to a definite conclusion on the genetic basis for bronchial asthma in our study but it maybe thought provoking to conduct further studies on the genetic component. |
| In a study conducted by Sodhi et al., [13]The mean age of their patients who had bronchial asthma was 26.85 years. Slight male preponderance has been seen.The mean duration of illness was 9.75 years.Patients had limited or no knowledge about bronchial asthma and its treatment protocols.Most of the patients were using inhalers but inhaler mishandling and discontinuation of inhaler therapy has been reported in the study.Alternate systems of medicine were used by the patients.Majority of their patients avoided trigger factors. | In our study, the mean age of the patients was 39.39 years. Majority of the patients were males.In our study, majority of the patients had duration of the illness ranging between 5-10 years.Patients had knowledge and were educated about bronchial asthma and its treatment protocols.Inhalers were used by majority of the patients and were not a contributory factor for poor asthma control in our study.No alternate systems of medicine were used by the patients.No evidence of avoiding trigger factors seen in the patients in our study. |
| In a study conducted by Gaude et al., non-compliance was one of the major factors contributing to bronchial asthma [14]. | In our study, majority of the patients were compliant and compliance was not a major factor for poor asthma control. |
| In a review article written by Barnes and Woodlock, it has been suggested that bronchial asthma can worsen despite regular treatment due to irreversible obstruction. They have also suggested trying medications such as selective potassium channel openers, interleukin-5 antagonists and chemokine receptor antagonists [15]. | 66% of our patients were poorly controlled despite regular treatment. Lung parenchymal remodelling is an important factor which needs to be considered. Fibreoptic bronchial biopsy and high resolution computed tomography could be used for further evaluation as our study only incorporated sputum eosinophil analysis and lung function tests. |
Limitation
The study could have been better if the sample size was larger. The study design was cross-sectional. Therefore, a prospective study with an intense follow up for at least 30 days may throw more light on the factors aggravating the condition.
Conclusion
Thus the study has shown that regular objective monitoring is essential in evaluating the response to treatment. As age advances the duration of asthma obviously increases and at that point of time assessment of inflammation and identifying the non-responders may be necessary to modify the treatment strategy. Modified questionnaire is useful in evaluating asthma-control. Sputum eosinophil count correlates with asthma-control. Factors significantly contributing to poor asthma control were duration, age and severity which might have led to persistent inflammation leading to poor response to regular medication.