Changing Trends of Skin Cancer: A Tertiary Care Hospital Study in Malwa Region of Punjab
Sonal Tina Lal1, Raja Paramjeet Singh Banipal2, Deepak John Bhatti3, Hanuman Prasad Yadav4
1 Assistant Professor, Department of Plastic Surgery, GGS Medical College and Hospital, Faridkot, Punjab, India.
2 Associate Professor, Department of Radiotherapy, GGS Medical College and Hospital, Faridkot, Punjab, India.
3 Professor and Head, Department of Plastic Surgery, GGS Medical College and Hospital, Faridkot, Punjab, India.
4 Professor and Head, Department of Radiotherapy, GGS Medical College and Hospital, Faridkot, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sonal Tina Lal, 61, Medical Campus, Sadiq Road, Faridkot, Punjab-151203, India.
E-mail: sonalbanipal@gmail.com
Introduction
Skin cancer constitutes a small but significant proportion of patients with cancer. Although the presence of eumelanin in dark skin is protective against the development of skin cancer, it is increasingly being diagnosed in the Indian population.
Aim
To study the profile of skin cancer patients presenting to a tertiary hospital in Malwa area of Punjab, India.
Materials and Methods
Retrospective study was done to analyse the profile of skin cancer patients who attended the institution over one year from 1st December 2013 to 30th November 2014. A comprehensive review of aetiology and related risk factors was done to correlate the environmental factors with high skin cancer prevalence in this region.
Results
Skin cancer constituted (3.18%) 84 out of 2638 patients registered with cancer of all types. The age of the patients was 62±14.2 years and ranged from 27 to 92 yrs. Basal cell carcinoma (BCC) was the most common histological type(46/84, 54.76%) followed by squamous cell carcinoma (SCC) (31/84, 36.91%) and malignant melanoma (MM) (7/84, 8.33%). Male: female ratio was found to be 0.79:1. BCC showed higher female preponderance (p<0.05). Head and Neck was the commonest site involved (p<0.05). Majority (88%) of patients were from rural area. 92% of patients were directly into the profession of agriculture with history of prolonged exposure to sunlight.
Conclusion
Skin cancer constitutes a small but significant proportion of patients with cancers. This study highlights a paradoxically increasing trend of BCC and female preponderance. Head and neck is the most common site involved. Exposure to Ultra Violet B (UVB) radiation and higher levels of arsenic in drinking water has been reported to be associated with skin cancers. Limited studies show that levels of arsenic and pesticides were higher in the samples of drinking water in Malwa area of Punjab. Therefore a multipronged strategy to provide safe drinking water supply and discouraging the indiscriminate use of pesticides is recommended.
Arsenic, Basal cell carcinoma, Skin cancer, Ultraviolet radiation
Introduction
There has been an increasing concern in print and electronic media regarding increased incidence of cancer in the Malwa belt of Punjab. Various authors have attempted to scientifically correlate the available data with environmental factors. Although skin cancer is a less common malignancy, its incidence is noted to be progressively increasing over last few decades [1,2]. Basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and malignant melanoma are the most frequent primary skin cancers. BCC and SCC are together known as Non-Melanomatous Skin Cancers (NMSC). Skin cancers are relatively uncommon malignancies worldwide not ranking among the first ten common cancers [1], although there has been progressive increase in the skin cancers over last few decades [2].
Of all the diagnosed cancers in India, less than 1% is skin cancer. Worldwide BCC is the commonest cutaneous malignancy, but in India, SCC is reported to be the most prevalent skin cancer [3]. Skin cancer incidence in India is relatively lower in comparison to the western world [4], but absolute number of cases is estimated to be significant due to larger population base. In India, skin cancer constitutes less than 1% of all diagnosed cancers. BCC is the commonest skin cancer worldwide, but various studies from India have consistently reported SCC as the most prevalent skin malignancies [3]. Although, the incidence of skin cancers in India is lower as compared to the western world [4], absolute number of cases is estimated to be significant due to larger population base.
Although the incidence of all types of skin cancers is thought to be lower among Indians due to the protective effect of melanin, there are several smaller reports that NMSCs may be on the rise in India [5]. Conventional thinking is that the incidence of all varieties of skin cancer is lower among Indian due to protective effect of melanin. Though national surveys and cross-country data in India are unavailable, there are several smaller reports that NMSCs may be on the rise in India [5]. A significant number of patients have reported to the Plastic Surgery department in our institution over a year with skin tumors and have undergone required excision and reconstructive surgeries for the same. Similarly, on review of oncological registrations there are significant numbers of new cases reported. A hospital based study in this region reported a paradoxically increasingly trend of BCC with female predilection [6].
NMSCs arise from keratinocytes. Ultraviolet B radiation (UVB 290-320 nm) derived from sun exposure is a well known agent causing NMSCs [7]. Arsenic, radiation therapy, coal tar and various hydrocarbons are other important aetiological agents [8]. Arsenic, in compound form used in insecticides, pesticides, herbicides and poultry feeds is poisonous and harmful environmental contaminant [9]. In humans arsenic is known to cause skin cancer [10]. Both SCC and BCC arise from keratinocytes. Ultraviolet radiation cause skin derived from sun exposure is well known to be most important cause of skin cancer. Epidemiological data and experimental evidence indicate that UVB radiation (wavelength 290-320 nm) includes the most significant wavelengths for induction of skin cancers [7]. Other important aetiological agents include radiation therapy, arsenic, coal tar and various hydrocarbons [8]. Though pure arsenic is not poisonous, but its compounds that are used as pesticides, herbicides, insecticides and poultry feeds are poisonous. In fact, arsenic is a very harmful environmental contaminant [9] and in humans this element is known to cause skin cancer [10].
Major source of human exposure to arsenic is contaminated drinking water. The carcinogenic potential of inorganic arsenic exposure through drinking water is a cause for considerable concern, especially because the hazardous inorganic arsenic is a powerful human multi-site carcinogen [11,12]. In combination with UVB, arsenic can cause skin cancer [13]. Available data shows an increased level of Arsenic, Selenium and mercury in ground as well as tap water, more than permissible level of United States Environmental Protection Agency (USEPA). High use of pesticides is also well known in Punjab [14].
Aim
The purpose of this study was to analyse the profile of skin cancer patients presenting to tertiary care centre in Malwa area of Punjab. Some environmental factors correlating with high skin cancer prevalence in this region were reviewed.
Materials and Methods
This retrospective study was done at a tertiary hospital draining majority of the cases from Malwa area of Punjab. One year data of Plastic Surgery and Radiotherapy department was reviewed retrospectively. Patient record of total 84 patients with skin malignancies out of 2638 new cancer cases registered over a period of one year during 2013 to 2014 was analysed.
Patients were first evaluated in the outpatient clinic by a team of Plastic Surgeon and Radiation oncologist and they underwent treatment according to the protocol decided. A detailed history and clinical examination was done. Routine blood investigation, chest X-ray and imaging studies like CECT and MRI were done as and when required to see the local extent and regional spread of the tumour. Fine Needle Aspiration Cytology (FNAC)/Biopsy were carried out to look for regional spread. Depending upon the histology of the tumour, wide local excision with adequate margin was done. In case of large surgical defect not amenable for primary closure, reconstruction using skin grafts, local or regional flaps were performed as shown in [Table/Fig-1a-c,2a-c]. In cases of locally advanced growths and regional nodal spread adjuvant postoperative radiotherapy (60Gy/30# over 6 weeks) was given.
(a) Photograph of a patient with Basal Cell Carcinoma Nose. (b) Intra-operative photograph after tumour ablation and marking of Axial paramedian forehead flap for nasal reconstruction. (c) Four months post operative picture of well healed flap.

(a) Photograph of a patient with Basal Cell Carcinoma Glabellar region. (b) Intraoperative photograph after tumour ablation and marking for Limberg flap for reconstruction. (c) Two month postoperative photograph of well healed flap.

Statistical Analysis
To analyse the results, descriptive statistics such as mean, standard deviation (SD) and frequency tables were utilized. Various analytical tests such as χ2 test, p-value and t-test were used. The p-value less than 5% was considered as significant.
Results
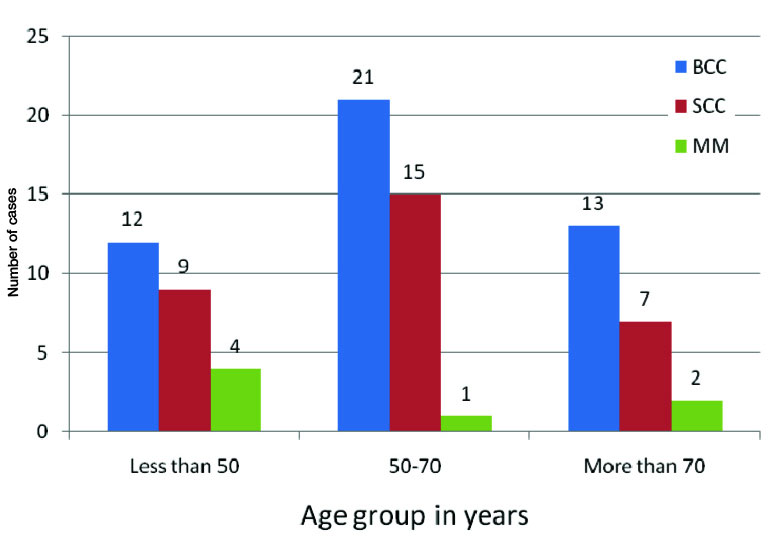
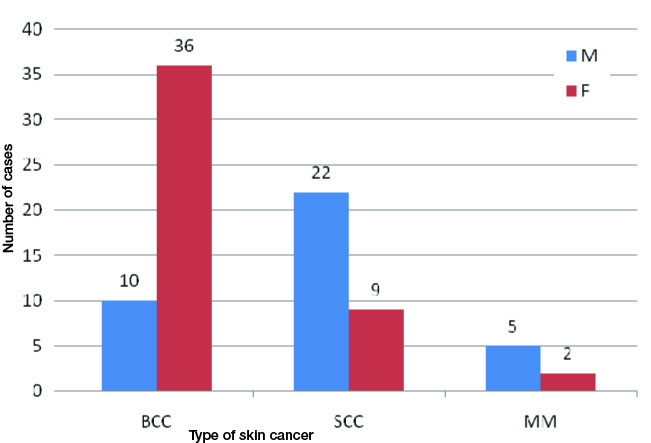
Skin cancers constituted 84 out of 2638 (3.18%) patients registered with cancers in the centre over a period of one year. Out of the 84 patients, 46 (54.76%) had BCC, 31 (36.91%) had SCC and 7 (8.33%) had melanoma [Table/Fig-3]. The age of the patients was 62 ± 14.2 years and ranged from 27 to 92 years [Table/Fig-4]. Thirty seven (44.05%) patients were men and remaining 47 (55.95%) were women (M: F=0.79:1). BCC showed higher prevalence among women (78.20%) while SCC (70.96%) and MM (71.43%) showed higher prevalence among males [Table/Fig-5]. There was significant association between type of skin cancer and gender affected, p-value was <0.05. Majority (88%) of patients were from rural area. A 92% of patients were directly into the profession of agriculture. These patients gave the history of prolonged exposure to outdoors in sunlight. Majority of cases (79.76%) had lesions confined to head and neck area. All cases of BCC and (67.74%) cases of SCC were found in head and neck area. There was statistically significant association between type of cancer and region involved (p-value <0.05). Distribution of skin cancer according to site involved is shown in [Table/Fig-6].
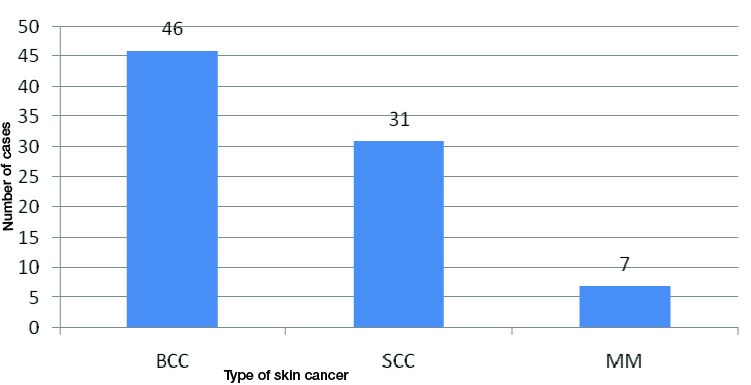
Age distribution of various skin cancers.
Sex distribution as per type of skin cancers.
Distribution of cancers as per the site involved.
| Part | Total |
|---|
| Type of Cancer | Head and Neck | Upper limb | Trunk | Perineal | Lower Limb |
|---|
| BCC | 46 | 0 | 0 | 0 | 0 | 46 |
| SCC | 21 | 2 | 0 | 5 | 3 | 31 |
| MM | 0 | 2 | 2 | 0 | 3 | 7 |
| Total | 67 | 4 | 2 | 5 | 6 | 84 |
Discussion
Over last few decades, incidence of skin cancer is increasing. NMSC is the commonest variety of cutaneous skin cancer [15]. BCC accounting for 70% of all malignant cancers of skin, is seen with largest incidence in white population [16]. This inverse relationship with degree of pigmentation and incidence may be due to protective effect of eumelanin on ultraviolet light (UVL) – induced damage [17]. Incidence of skin cancer has been increasing since last few decades worldwide. NMSC is the commonest variety of cutaneous malignancy [15]. The largest incidence is seen in white population, in whom BCC is accounting for approximately 70% of all malignant diseases of skin [16]. The incidence shows an inverse relation with the degree of pigmentation, presumably due to protective effect of eumelanin on ultraviolet light (UVL) - induced damage [17].
The reported incidence of skin cancer in India is less than 1% of all the cancers [18]. In our study the incidence of skin cancers is found to be 3.18% of all the cancer patients registered over a period of one year at our centre. NMSC is known to be uncommon in Asians [19]. Among dark skin individuals SCC is commoner than BCC. Various studies from India reported SCC to be most prevalent skin malignancy [3,20–25]. A study from Malwa region of Punjab has shown BCC as the commonest skin malignancy [26] [Table/Fig-7]. In our study also, we noted a change in trend in the histological variety of tumour, BCC (54.76%) being the commonest type of skin malignancy.
Studies showing common type of skin cancers in India.
| S.No | Author | Year | Commonest skin cancer type |
|---|
| 1 | Khanolkar VR et al., [21] | 1945 | SCC |
| 2 | Godbole VK et al., [3] | 1968 | SCC |
| 3 | Talvalkar GV et al., [20] | 1970 | SCC |
| 4 | Budharaj SN et al., [22] | 1972 | SCC |
| 5 | NCRP ICMR [23] | 1996 | SCC |
| 6 | Laishram RS et al., [24] | 2010 | SCC |
| 7 | Adinarayan M et al., [25] | 2011 | SCC |
| 8 | Brar BK et al., [26] | 2015 | BCC |
Punjab is India’s one of most prosperous state, largely due to the green revolution. Seventy percent of population is directly or indirectly associated with agriculture. In our study, majority of cases belong to agricultural background with history of prolonged sun exposure while working in the fields.
The role of some environmental factors in the causation of skin cancers was reviewed. UVB radiation is well known as agent inducing non melanoma skin cancers in a dose dependent way. The effects of UVB radiation are enhanced by ozone depletion, which is responsible for an increase in biologically damaging solar UVB radiations reaching the Earth surface [27]. Mathematical models suggest an increase of 2-4% in the incidence of skin tumour for each 1% reduction in ozone layer [28]. But factors other than the mentioned above need to be searched and verified as ozone destruction is most evident over the temperate and Polar Regions, while India is a tropical country [29,30].
Ingestion of arsenic, both from drinking water supplies and medicinal preparations is known to cause skin cancers [31]. The association between arsenic ingestion and skin cancer has been documented since the late 19th century. BCC and SCC have repeatedly been reported to be associated with ingestion of arsenic alone or in combination with other risk factors [32]. The compounds of arsenic are used as pesticides, herbicides, insecticides and poultry feeds. Also inorganic arsenic, a metalloid is ubiquitously distributed in nature. Under certain conditions like pH, temperature etc, inorganic arsenic easily dissociates from its soil bound forms and enters the aquifers [33]. For this reason, the major source of human exposure to arsenic is the drinking water of course, the contaminated groundwater. In combination with UVB arsenic can cause skin cancer. Indeed arsenic-UVB interaction provides reasonable explanation for the cases of arsenical cancers in sun exposed skin. Multiple and recurrent skin lesions are associated with cellular immunity dysfunction in chronic arsenism [13]. The main proposed mechanisms regarding arsenic carcinogenicity are induction of chromosomal abnormalities, promotion and oxidative stress [34,35].
In a study by Sharma et al., many of the water samples taken from existing hand-pumps, submersible pumps, tube-wells, dug-wells (underground water) and municipal water supply from the south western districts of Punjab were analysed and found to have high content of Arsenic beyond their permissible limits said by WHO along with high variability. Study has revealed that 80% of water samples analysed was having arsenic concentration above the safe limit (10μgm/L) [36].
Limitation
The limitations of this particular study are that this was a retrospective study. Longer prospective studies are required over a bigger population to have exact data on skin cancer in this area.
Conclusion
Incidence of skin cancer is high in Malwa region of Punjab. Basal cell carcinoma is recorded as the commonest histological type and may be attributed to climate changes, exposure to UVB and high levels of arsenic in drinking water. Females are affected more than males. As the incidence rate of skin cancers is dramatically increasing, a clear understanding of the multiple causative factors is an essential step in their prevention. A multipronged strategy to provide safe water supply and discouraging the indiscriminate use of pesticides is recommended. Implementation of comprehensive cancer registry, which includes exposure to environmental agents, is essential in pinpointing the actual causes.
[1]. WHO world health statistics. GLOBOCAN 2000: Cancer Incidence, Mortality and Prevalence Worldwide version 1.0. IARC CancerBase No. 5. Lyon, IARC Press; 2001 [Google Scholar]
[2]. Howe HL, Wingo PA, Thun MJ, Riess LAG, Rosenberg HM, Feigal EG, Annual report to the nation on the status of cancer (1973 through 1998), featuring cancers with recent increasing trendsJ Natl Cancer Inst 2001 93:824-42. [Google Scholar]
[3]. Godbole VK, Toprani HT, Shah HH, Skin cancer in saurashtraInd J Pathol Bacteriol 1968 11:183-89. [Google Scholar]
[4]. Deo SV, Hazarika S, Shukla NK, Kumar S, Kar M, Samaiya A, Surgical management of skin cancer: Experience from a regional cancer centre in IndiaIndian J Cancer 2005 42:145-50. [Google Scholar]
[5]. Panda S, Nonmelanoma skin cancer in India: Current scenarioIndian J Dermatol 2010 55(4):373-78. [Google Scholar]
[6]. Kumar S, Mahajan BB, Kaur S, Yadav A, Singh N, Singh A, A study of Basal cell carcinoma in South Asians for risk factors and clinicopathological characterization: A hospital based studyJournal of skin cancer 2014 3(2014):173582 [Google Scholar]
[7]. Leaf A, Potential health effects of global climatic and environmental changesN Engl J Med 1989 321:1577-83. [Google Scholar]
[8]. Tadini G, Restano L, Gonzales–Parez R, Gonzales-Ensenat MA, Vincente-Villa MA, Cambiaghi S, Phacomatosis pigmentokeratotica. Report of new cases and further delineation of syndromeArch Dermatol 1998 134:333-37. [Google Scholar]
[9]. Tokunaga Risk assessment of arsenic for people who live in the area of arsenic-contaminated underground water in BangladeshKokuritsu Iyakuhin Shokuhin Eisei Kenkyusho Hokuku 2007 125:1-16. [Google Scholar]
[10]. Rossman TG, Uddin AN, Burns FJ, Evidence that arsenic acts as carcinogen in skin cancerToxicol App Pharmacol 2004 198:394-404. [Google Scholar]
[11]. IARC Working Group on the Evaluation of Carcinogenic Risks to HumansSome drinking-water disinfectants and contaminants, including arsenic. IARC Monogrc Eval CarcinogRisks Hum 2004 84:269-477. [Google Scholar]
[12]. Chouhan S, Flora SJ, Arsenic and fluoride: Two major ground water pollutantsIndian J Biol 2010 48:666-78. [Google Scholar]
[13]. Yu HS, Liao WT, Chai CY, Arsenic carcinogenesis in the skinJ Biomed Sci 2006 13:657-66. [Google Scholar]
[14]. Thakur JS, Rao BT, Rajwanshi A, Parwana HK, Kumar R, Epidemiological study of high cancer among rural agricultural community of punjab in rural indiaInt J Environ Res Public Health 2008 5(5):399-407. [Google Scholar]
[15]. Preston DS, Stern RS, Nonmelanoma cancers of the skinN Engl J Med 1992 327:1649-62. [Google Scholar]
[16]. Casson P, Basal cell carcinomaClin Plast Surg 1980 7:301-11. [Google Scholar]
[17]. Yamaguchi Y, Beer JZ, Hearing VJ, Melanin mediated apoptosis of epidermal cells damaged by ultraviolet radiation: factors influencing the incidence of skin cancerArch Dermatol Res 2008 300:S43-50. [Google Scholar]
[18]. Mahajan MK, Lal P, Biswal BM, Mohanti BK, Cancer of skin. In: Rath GK, Mohanti BK, editorsText book of radiation oncology: principles and practice 2000 New YorkB. I. Churchill Livingstone:223-37. [Google Scholar]
[19]. Scotto J, Fears TR, Fraumeni JF. Washington: DC: Government Printing Office; 1983. Incidence of nonmelanoma skin cancer in United States. (NIH Publication No 83-2433) [Google Scholar]
[20]. Talvalkar GV, Squamous cell carcinoma of skin: its incidence and aetiopathogenesis in 625 casesInd J Cancer 1970 7:24-33. [Google Scholar]
[21]. Khanolkar VR, Suryabhai B, Cancer in relation to usagesArch Patho 1945 40:351-61. [Google Scholar]
[22]. Budhraja SN, Pillai VC, Periyanayagam WJ, Kaushik SP, Bedi BM, Malignant neoplasm of skin in PondicherryInd J Cancer 1972 9:284-95. [Google Scholar]
[23]. National Cancer Registry Programme, Indian Council of Medical Research (1990-1996) consolidated report of the population based cancer registries [Google Scholar]
[24]. Laishram RS, Banerjee A, Punyabati P, Sharma DC, Pattern of skin malignancies in Manipur, India: A 5-yr histopathological reviewJournal of Pakistan Association of Dermatologists 2010 20:128-32. [Google Scholar]
[25]. Adinarayan M, Krishnamurthy SP, Clinicopathological evaluation of nonmelanoma skin cancerIndian J Dermatol 2011 56:670-72. [Google Scholar]
[26]. Brar BK, Sethi N, Khanna E, an epidemiological review of skin cancer in Malwa belt of Punjab India: a 3-yr clinicopathological studySch J App Med Sci 2015 3(9 D):3405-08. [Google Scholar]
[27]. Madronich S, de Gruijl FR, Strast rophic Ozone Deplaetion between 1979 and 1992: Implications for biologically active ultraviolet-B radiation and non– melanoma skin cancer incidencePhotochem Photobiol 1994 59:541-46. [Google Scholar]
[28]. Fears TR, Scott J, Estimating increases in skin cancer morbidity due to increases in ultraviolet radiation exposureCancer Invest 1983 1:119-26. [Google Scholar]
[29]. Myth: Ozone Deplaetion Occurs Only in Antarctica | Science | Ozone Layer Protection | US EPA. http://www.epa.gov/ozone/science/myths/glob_dep.html [Google Scholar]
[30]. World Meteorological Organization. Assessment of Ozone Deplaetion. World Meteorological Organization; 2010. http://search.usa.gov/search?affiliate=esrl.noaa.gov_csd&query=assessment+of+ozone+deplaetion [Google Scholar]
[31]. Fabbrocini G, Triassi M, Mauriello MC, Torre G, Annunziata MC, Vita VD, Epidemiology of skin cancer: Role of some environmental factorsCancers 2010 2:1980-89. [Google Scholar]
[32]. Guo HR, Yu HS, Hu H, Monson RR, Arsenic in drinking water and skin cancers: Cell-type specificity (R.O.C.)Cancer Causes Contr 2001 12:909-16. [Google Scholar]
[33]. Smedley PL, Kinniburg DG, A review of source, behavior and distribution of arsenic in natural watersAppl Geochem 2002 17:517-68. [Google Scholar]
[34]. Kitchin KT, Recent advances in arsenic carcinogenesis: Modes of action, animal model system methylated arsenic metabolitesToxicol Appl Pharmacol 2001 172:249-61. [Google Scholar]
[35]. Kitchin KT, Ahmad S, Oxidative stress as a possible mode of action for arsenic carcinogenesisToxicol Lett 2003 137:3-13. [Google Scholar]
[36]. Sharma C, Mahajan A, Garg UK, Assessment of arsenic in drinking water samples in south-western districts of Punjab-IndiaDesalination and water treatment 2013 51:5701-09. [Google Scholar]