Parathyroid Adenoma Completely Impacted within the Thyroid Gland: A Case Report
Sayed Mahmoud Mirhosaini1, Soroush Amani2, Rana Fereidani3
1 Assistant Professor, Department of Internal Medicine, Hajar Hospital, Shahrekord University of Medical Sciences, Shahrekord, Iran.
2 Otolaryngologist, Department of Otolaryngology, Kashani Hospital, Shahrekord Univrsity of Medical Sciences, Shahrekord, Iran.
3 Pathologist, Department of Pathology, Kashani Hospital, Shahrekord University of Medical Sciences, Shahrekord, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Soroush Amani, Otolaryngologist, Department of Otolaryngology, Kashani Hospital, Shahrekord University of Medical Sciences, Parastar Street, Shahrekord, Iran. E-mail : soamani2008@yahoo.com
Ectopic parathyroid adenoma can be seen in various locations. Sometimes ultrasound and even fine needle aspiration studies cannot distinguish this lesion from thyroid lesions. A 29-year-old woman with a prominent nodule of left thyroid lobe was referred to surgical department. Thyroid function test were normal. She had no family history of parathyroid disease, other endocrine disease, and any other malignancies and had received no radiation. Ultrasonography revealed a solid and hypoechoic mass, 25x20 mm in size, with a regular shape and contour without calcification in the inferior of left lobe of the thyroid gland. For definite diagnosis, immunohistochemistry study of the lesion with three markers was done. Finally, PTH marker was positive in cytoplasms of cells so parathyroid adenoma was confirmed. Fine needle aspiration of the nodule was suspicious for follicular neoplasm; however, postoperative histopathology and immunohistochemistry revealed a parathyroid adenoma. Ultrasonography may be helpful to identify localized thyroid lesions especially in parathyroid adenoma.
Benign, Cytoplasm, Ultrasonography
Case Report
A 29-year-old woman with a prominent nodule of left thyroid lobe was referred to surgical department. Thyroid function test was normal. She had no family history of parathyroid disease, other endocrine disease, and any other malignancies as well as no radiation to the head and neck in childhood. Ultrasonography revealed a solid and hypoechoic mass, 25x20 mm in size, with a regular shape and contour without calcification in the inferior of left lobe of the thyroid gland. The lesion was investigated by fine needle aspiration (FNA) of the lesion and the cytology revealed "follicular neoplasia".
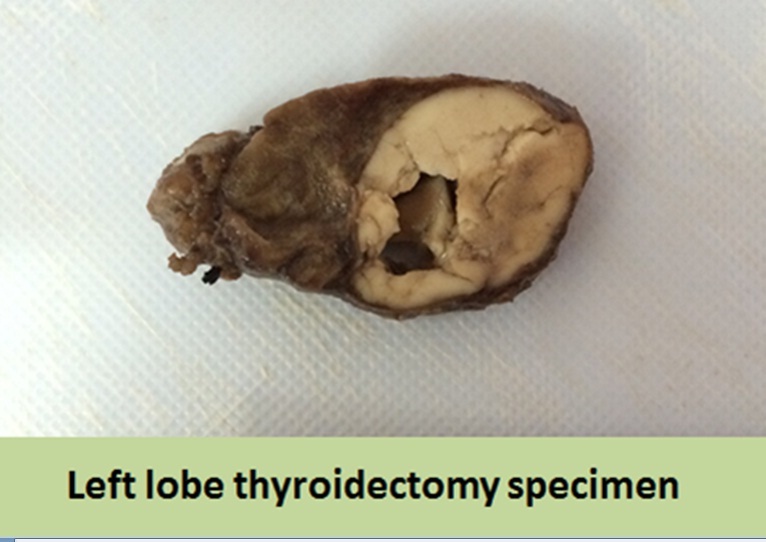
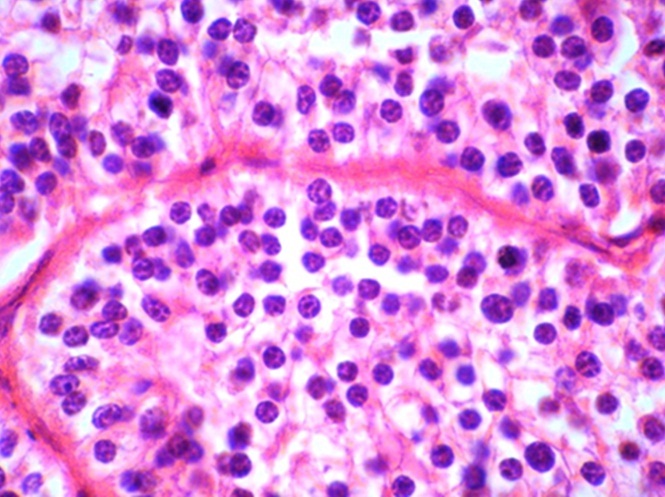
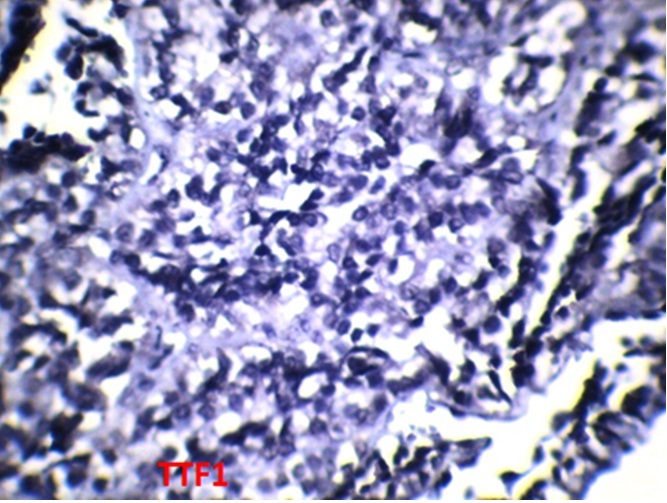
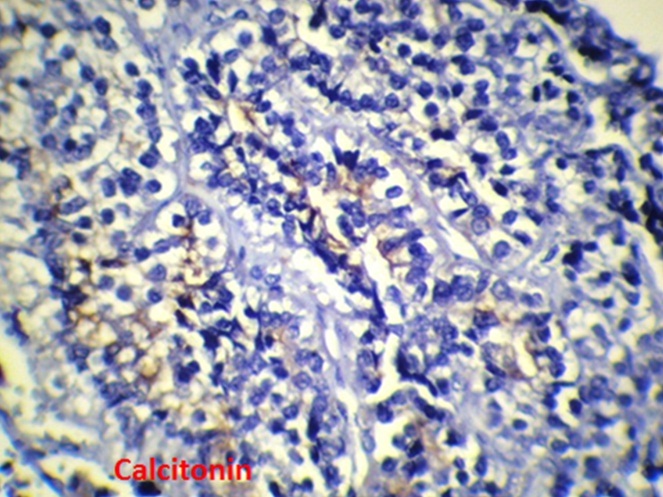
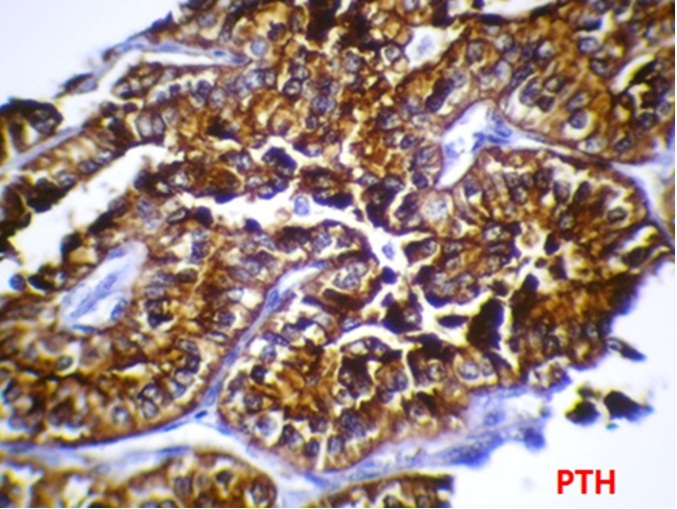
The patient was referred to the surgical department. A left side thyroid lobectomy was performed. On macroscopic examination the left lobe was 5x2.5x2 cm. A 3-cm, creamy-whitish solid nodule, confined to thyroid capsule, was identified [Table/Fig-1]. Microscopically, the lesion was consisted of uniform cells with light eosinophilic cytoplasm encompassing round, monomorph nuclei with punctate chromatin and fine nucleoli, arranged in diffuse and trabecular pattern with a well-developed capillary network [Table/Fig-2]. After operation, the patient complained of muscular spasm in the legs and numbness and tingling in the fingertips. Calcium level was 7.7 mg/dl postoperatively. Follow-up of the patient revealed slow rise in calcium levels and relief of symptoms. This could be in favor of parathyroid adenoma and can be explained by atrophy of residual glands in the presence of a single hyperfunctioning adenoma. Unfortunately we did not have any information about the patient’s preoperative calcium level. The differential diagnoses were: parathyroid adenoma, follicular adenoma of thyroid and medullary carcinoma of thyroid. For definite diagnosis, immunohistochemical study of the lesion with three markers was done. TTF-1 was negative so follicular lesion of thyroid was ruled out [Table/Fig-3]. Calcitonin was also negative so there was no possibility of medullary carcinoma [Table/Fig-4]. PTH marker was positive in cytoplasms of cells [Table/Fig-5] and parathyroid adenoma was confirmed.
A creamy-whitish solid nodule was confined to thyroid capsule.
Trabecular pattern with a well-developed capillary network.
Immunohistochemistry image of the lesion that TTF-1 was negative.
Immunohistochemistry image of the lesion that calcitonin was negative.
PTH marker was positive in cytoplasms of cells.
Discussion
In about 6-16% of cases of parathyroid adenoma, one or more parathyroid gland(s) were found in an ectopic location, predominantly in thymus (38%) followed by 31% in the retroesphageal region, 18% were intrathyroidal [1].
The reported case is related to the issues concerning the differential diagnosis of thyroid from parathyroid pathology. In some studies incidental parathyroid adenoma has been detected after thyroid surgery [2,3].
Although, neck ultrasound was demonstrated to be very helpful in detecting hyperfunctioning parathyroid glands in hyperparathyroidism patients, the positive predictive value declines if parathyroid pathology is unsuspected [4]. Because both pathologic entities may be indicated as hypoechogenic structures and peripheral hypervascularization may be absent in hyperfunctioning parathyroid glands, thus the FNA was indicated. However, the major problem with this easily performed procedure is insufficient cohesive cellular structures; therefore, only cytologic examination could be conducted. Although misinterpreting parathyroid adenoma as papillary thyroid carcinoma is rare in aspiration cytology [5], the differentiation from follicular thyroid carcinoma (or adenoma), as with our patient, is still more problematic and may lead to immunocytochemical staining for PTH [6]. Parathyroid adenomas are very likely to be cytologically mistaken for a follicular lesion of the thyroid [7,8]. As with the ultrasound examination of our patient, the FNA interpretation relies greatly on clinical data. The final diagnosis is often made only by postoperative histopathology, which was fortunately diagnosed as a benign parathyroid adenoma in our patient.
Conclusion
Fine needle aspiration of the nodule was suspicious for follicular neoplasm; however postoperative histopathology and immunohistochemistry revealed a parathyroid adenoma. Ultrasonography may be helpful to identify localized thyroid lesions especially in parathyroid adenoma.
[1]. Roy M, Mazeh H, Chen H, Sippel RS, Incidence and localization of ectopic parathyroid ademonas in previously unexplored patientsWorld Journal of Surgery 2013 37(1):102-06. [Google Scholar]
[2]. Katz A, Kong L, Incidental preclinical hyperparathyroidism identified during thyroid operationsThe American Surgeon 1992 58(12):747-49. [Google Scholar]
[3]. Carnaille BM, Pattou FN, Oudar C, Lecomte-Houcke MC, Rocha JE, Proye CA, Parathyroid incidentalomas in normocalcemic patients during thyroid surgeryWorld Journal of Surgery 1996 20(7):830-34. [Google Scholar]
[4]. Frasoldati A, Pesenti M, Toschi E, Azzarito C, Zini M, Valcavi R, Detection and diagnosis of parathyroid incidentalomas during thyroid sonographyJournal of Clinical Ultrasound 1999 27(9):492-98. [Google Scholar]
[5]. Friedman M, Shimaoka K, Lopez C, Shedd D, Parathyroid adenoma diagnosed as papillary carcinoma of thyroid on needle aspiration smearsActa Cytologica 1982 27(3):337-40. [Google Scholar]
[6]. Absher KJ, Truong LD, Khurana KK, Ramzy I, Parathyroid cytology: avoiding diagnostic pitfallsHead & Neck 2002 24(2):157-64. [Google Scholar]
[7]. Tambouret R, Szyfelbein WM, Pitman MB, Ultrasound-guided fine-needle aspiration biopsy of the thyroidCancer Cytopathology 1999 87(5):299-305. [Google Scholar]
[8]. Winkler B, Gooding G, Montgomery C, Clark O, Arnaud C, Immunoperoxidase confirmation of parathyroid origin of ultrasound-guided fine needle aspirates of the parathyroid glandsActa Cytologica 1986 31(1):40-44. [Google Scholar]