The papulosquamous skin disorders are characterized by scaly papules and plaques [1]. These assume considerable importance because of their frequency of occurrence. As all are characterised by scaly papules confusion may result in their diagnosis. Although histopathological study is considered the gold standard in diagnosing dermatological lesions, it has its limitations and very often a definite ‘specific’ diagnosis is not possible [2]. The limitations of histopathology in arriving at a specific diagnosis maybe due to treatment effect, non-classical presentation, inappropriate biopsy site or overlapping clinical and histopathological features. Histopathological reporting should be accompanied by clinical history because of the overlapping histopathological features of different clinical conditions [3]. Some papulosquamous conditions like psoriasis present with numerous clinical variants and mimic various dermatological conditions. This leads to a diagnostic dilemma for the clinician. The pathogenesis of conditions like lichen planus is not exactly defined [4]. In case of such diseases, studies are lacking in India. Therefore, a clinicopathological correlation will go a long way in proper treatment of such diseases and can vary the prognosis significantly. Younas and Haque stressed on the importance of definite differentiation in the diagnosis of papulosquamous skin diseases [5]. D’Costa emphasized on clinicopathological correlation in the diagnosis of papulosqaumous skin diseases [4]. The present study is an attempt to analyse various histopathological patterns of non- infectious erythaematous, papulosquamous lesions of the skin based on the tissue reaction pattern and to assess the concordance of provisional clinical diagnosis and histopathological diagnosis. The study also discusses the reasons for low concordance.
Materials and Methods
The study comprised of 150 clinically diagnosed/suspected and untreated cases of non-infectious erythaematous, papulosquamous lesions of the skin attending the Department of Dermatology in a tertiary care hospital between July 2012 and August 2014. Skin biopsies from 150 clinically diagnosed/suspected cases of non-infectious erythaematous, papulosquamous lesions were performed by the dermatologist and sent to the Department of Pathology in 10% formalin. The specimen obtained was subjected to tissue processing after fixation. Tissue sections were prepared from paraffin block and stained with haematoxylin and eosin followed by microscopic examination.
Inclusion Criteria
Cases included in the study were those with clinical features of non-infectious erythaematous, papulosquamous skin disorders.
Exclusion Criteria
Skin disorders with infective aetiology and other skin lesions which are not papulosquamous disorders were excluded.
Results
The present study comprised of 150 cases. Males (67%) were more commonly affected with a male to female ratio of 2:1. The age distribution pattern revealed that the maximum cases (24.66%) were in the age range of >60 years and the least number (0.66%) were in the youngest age range of 0-10 years.
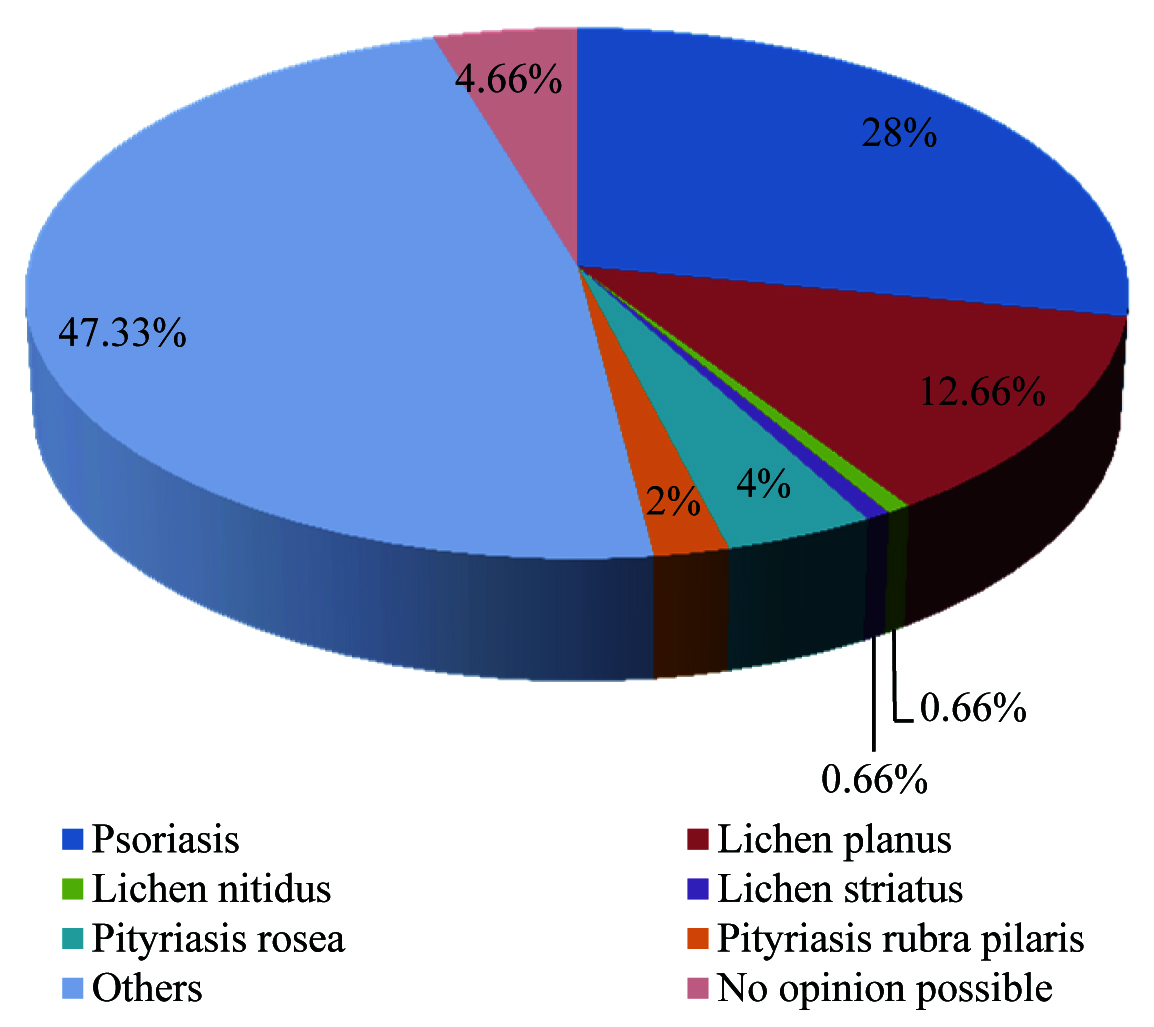
An analysis of the broad categories revealed that out of the 150 cases, 72 cases (48%) were histopathologically classified as non-infectious erythaematous, papulosquamous skin diseases. The most frequently encountered lesion was psoriasis (42 cases, 28%), followed by lichen planus (19 cases, 12.66%) and biopsy was inconclusive in 4.66% of the cases (7 cases). The remaining 47.33% (71cases) clinically suspected as papulosquamous conditions were categorised histopathologically as other conditions which were not included under papulosquamous skin diseases [Table/Fig-1]. The most frequently encountered tissue reaction pattern was the psoriasiform reaction pattern, among which psoriasis constituted the highest percentage of cases i.e., 28% of the total cases.
Incidence of skin lesions (n=150).
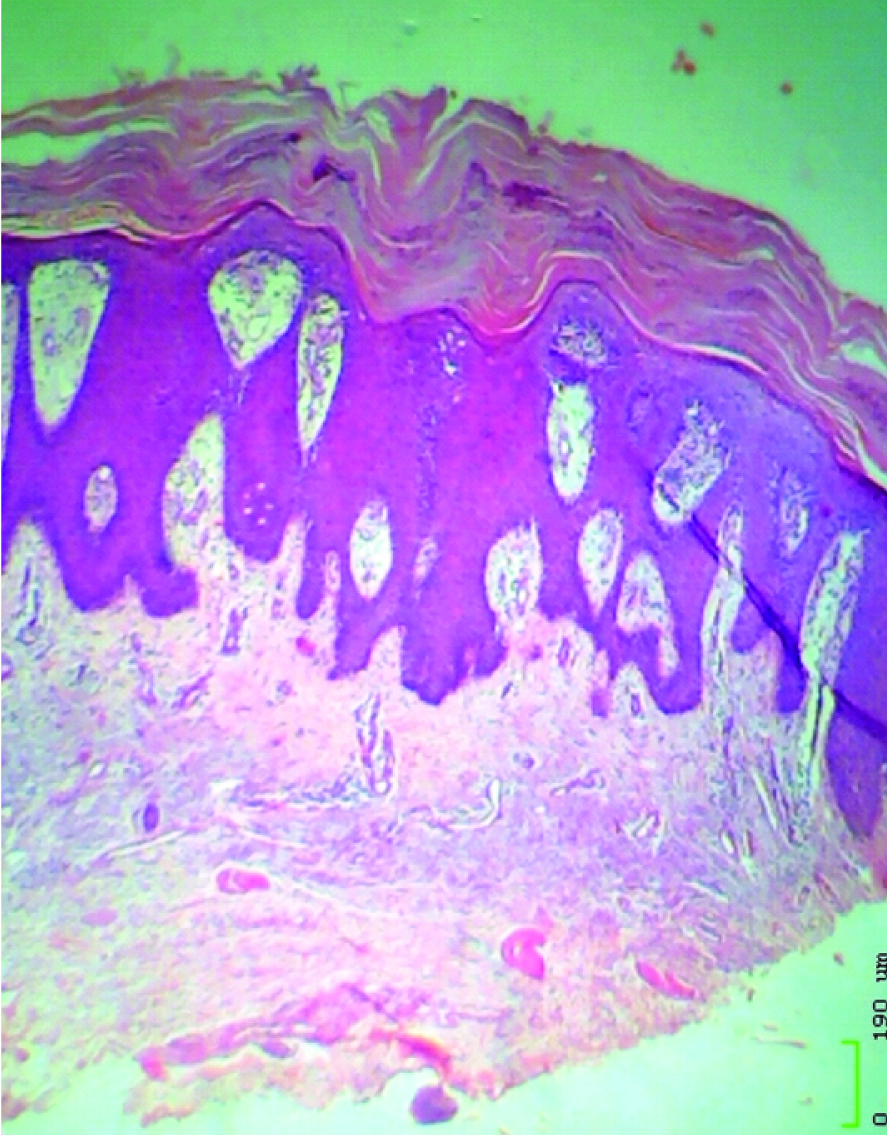
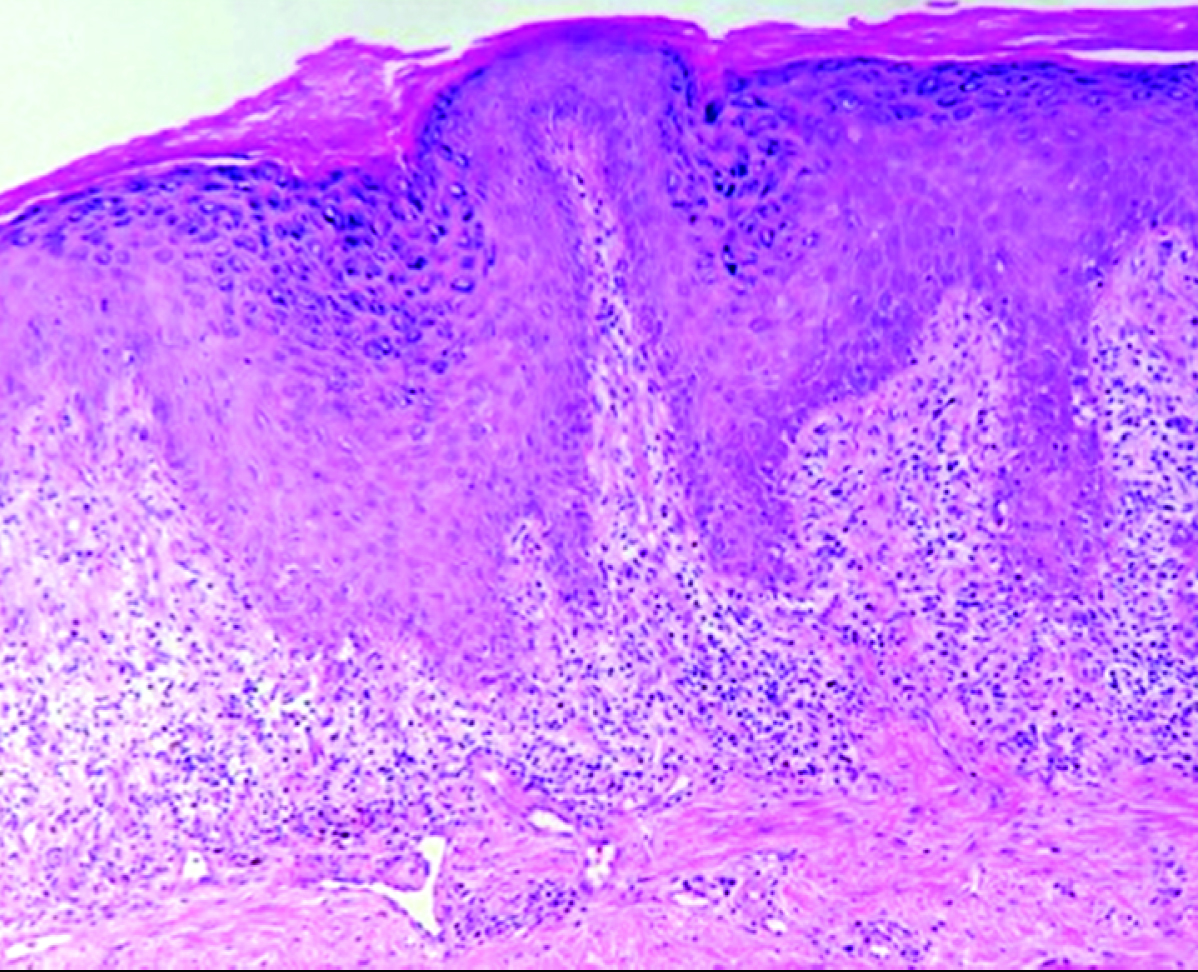
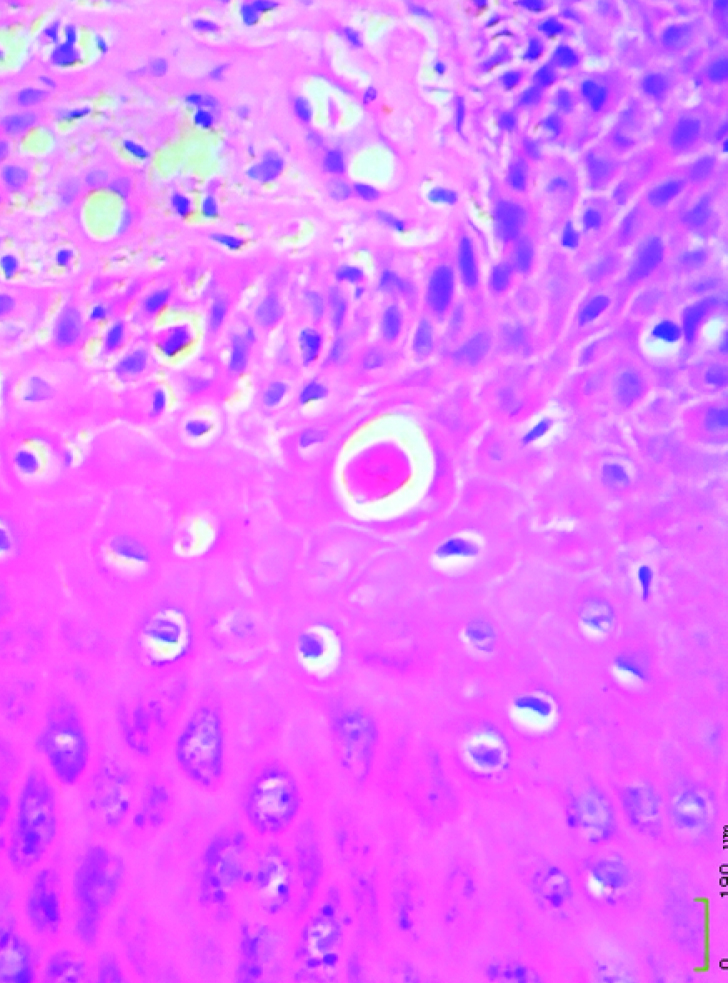
The most common histopathological findings in the epidermis in case of psoriasis were psoriasiform hyperplasia with acanthosis (90.47%) [Table/Fig-2,3]. In lichen planus, majority of them showed basal cell degeneration, hypergranulosis and diffuse inflammatory infiltrate in the dermis [Table/Fig-4,5]. One case of lichen nitidus showed elongated rete ridges with claw clutching ball appearance with hyperkeratosis, parakeratosis and dermal perivascular lymphocytic infiltrate. One case of lichen striatus diagnosed histopathologically showed parakeratosis and patchy papillary dermal lymphocytic infiltrate. All the six cases (100%) of pityriasis rosea showed spongiosis. Out of the three cases diagnosed as pityriasis rubra pilaris histopathologically, two cases (66.66%) showed follicular plugging, follicular and perifollicular parakeratosis, acanthosis and perivascular inflammation.
Of the 150 cases, 88 cases were clinically suspected to be psoriasis of which 40 cases (45.45%) were confirmed histopathologically. Out of 39 cases clinically suspected to be lichen planus, only 19 cases (48.71%) turned out to be lichen planus histopathologically. Of the three cases of lichen nitidus suspected clinically, 1 case (33.33%) was histopathologically confirmed. Five cases were diagnosed clinically as lichen striatus of which 1 case (20%) had positive correlation. One case of clinically suspected parapsoriasis turned out to be subacute spongiotic dermatitis histopathologically. Six cases (66.67%) out of 9 cases clinically suspected to be pityriasis rosea were confirmed histopathologically. Out of 5 cases of pityriasis rubra pilaris suspected clinically, 3 cases (60%) were histopathologically confirmed [Table/Fig-6]. A concordance between clinical diagnosis and histopathological diagnosis was observed in 46.67% of the cases and a discordance of 53.33% was analysed [Table/Fig-7].
Clinical presentation of psoriasis showing plaque on elbow with characteristic silvery-white powdery scaling.

Photomicrograph of a case of psoriasis showing hyperkeratosis, parakeratosis, psoriasiform hyperplasia and fused rete ridges (H&E; 100X)
Photomicrograph of a case of lichen planus showing hyperkeratosis, hypergranulosis and band like inflammatory infiltrate (H&E; 40x).
Photomicrograph showing Civatte body (H&E; 400X)
Correlation of clinical diagnosis with histopathological diagnosis
| Clinical diagnosis n= 150 | Number of cases | Histopathological diagnosis |
|---|
| Correlation | No correlation | Inconclusive |
|---|
| No. | % | No. | % | No. | % |
|---|
| Psoriasis | 88 | 40 | 45.45 | 44 | 50 | 4 | 4.54 |
| Lichen planus | 39 | 19 | 48.71 | 18 | 46.15 | 2 | 5.13 |
| Lichen nitidus | 3 | 1 | 33.33 | 1 | 33.33 | 1 | 33.33 |
| Lichen striatus | 5 | 1 | 20 | 4 | 80 | - | - |
| Parapsoriasis | 1 | 0 | 0 | 1 | 100 | - | - |
| Pityriasis rosea | 9 | 6 | 66.67 | 3 | 33.33 | - | - |
| Pityriasis rubra pilaris | 5 | 3 | 60 | 2 | 40 | - | - |
| Total | 150 | 70 | | 73 | | 7 | |
Overall correlation of clinical diagnosis with histopathological diagnosis.
| Clinical correlation | Number of biopsies | Percentage (%) |
|---|
| Positive | 70 | 46.67 |
| Negative | 80 | 53.33 |
| Total | 150 | 100 |
Discussion
Psoriasis
Out of a total of 88 cases clinically suspected as psoriasis, 40 cases (45.45%) were confirmed histopathologically, 44 cases (50%) were diagnosed as some other condition and the diagnosis was inconclusive in 4 cases (4.54%). The most frequent histopathological findings in the present study were psoriasiform hyperplasia with acanthosis, parakeratosis and dermal infiltrate. When the present study was compared to a study by Puri et al., it was found that the difference between the two studies, with respect to psoriasiform hyperplasia with acanthosis, was non-significant (p=0.354, i.e.;>0.05) [6]. Therefore, this study was comparable to the study by Puri et al., [6] [Table/Fig-8]. On comparing the present study with a study by Karumbaiah et al., it was found that there was statistically no significant difference between the two studies with respect to parakeratosis (p=0.3816) [7] [Table/Fig-8]. The clinical manifestations are misleading in many of these conditions. Some cases are clinically suspicious whereas others may present differently [7]. Problems due to overlap were noted in the present study. Five cases clinically suspected to be psoriasis were diagnosed as seborrhoeic dermatitis histopathologically. Fourteen cases which were clinically suspected to be psoriasis were diagnosed as spongiotic dermatitis histopathologically.
Comparison of histopathological changes in psoriasis
| Hisbottomathological changes* | Puri et al., [6](2012) (%)n=16 | Karumbaiah et al., [7](2014) (%)n=22 | Present study(2014) (%)n=42 |
|---|
| Epidermis |
| Hyperkeratosis | 56.25 | 77.27 | 28.57 |
| Parakeratosis | 87.5 | 72.72 | 61.90 |
| Psoriasiform hyperplasia with acanthosis | 81.25 | 72.72 | 90.47 |
| Suprapapillary plate thinning | 25 | 40.90 | 35.71 |
| Munro microabscess | 43.75 | 22.72 | 26.19 |
| Spongiform pustule of Kogoj | - | 4.54 | 11.90 |
| Hypogranulosis | 25 | 22.72 | 19.04 |
| Dermis |
| Papillary oedema | - | 27.27 | 19.04 |
| Vascular changes | 50 | 86.36 | 14.28 |
| Dermal infiltrate | 37.59 | 81.81 | 66.66 |
*Includes multiple findings for each case.
Lichen Planus
When the present study was compared to a study by Younas and Haque [5], it was found that with respect to irregular acanthosis with saw tooth rete ridges, the two studies were comparable (p=0.1929) [Table/Fig-9]. On comparing the present study with a study by Parihar et al., it was found that with respect to basal cell degeneration, there was significant difference between the two studies (p<0.0001) [8]. This could be attributed to the small sample size in the present study (n=19) in comparison with Parihar et al., (n=145) [8] [Table/Fig-9]. The findings of the present study were consistent with the classical description of lichen planus by Mobini et al., [9].
Comparison of histopathological changes in lichen planus.
| Hisbottomathological changes* | Younas and Haque [5](2004) (%)n=12 | Pariharet al., [8](2015) (%)n=145 | Present study(2016) (%)n=19 |
|---|
| Epidermis |
| Hyperkeratosis | + | - | 31.57 |
| Focal parakeratosis | - | - | 15.78 |
| Irregular acanthosisSaw tooth rete ridges | 66.6 | 9476 | 42.10 |
| Hypergranulosis | 83.3 | 96.5 | 52.63 |
| Basal cell degeneration | 100 | 99 | 57.89 |
| Max Joseph space | 58.3 | 29.5 | 10.52 |
| Civatte bodies | + | 82 | 21.05 |
| Orthokeratosis | - | 100 | 21.05 |
| Dermis |
| Band like inflammatory infiltrate | 100 | 94 | 42.10 |
| Diffuse inflammatory infiltrate | - | - | 57.89 |
* This table includes multiple findings for each case
+ Finding seen in majority of the cases
Lichen Nitidus
Lichen nitidus commonly occurs in young adults and children particularly in males [10]. Mehta and Balachandran reported no obvious racial or gender predilection [11]; however, majority of the cases were found in children and young adults. Lichen nitidus can be confused with and can coexist with lichen planus clinically.
Lichen Striatus
Lichen striatus is known to mimic linear verrucous epidermal nevus [12]. One case of lichen striatus which was diagnosed histopathologically, in the present study, showed parakeratosis and patchy papillary dermal lymphocytic infiltrate. These findings were consistent with the study by Zhang and McNutt [13].
Pityriasis Rosea
Both genders were equally susceptible according to some authors, while others quoted a female preponderance [14]. In our study, a female predominance was observed. The findings of the present study were comparable to the study by Prasad et al., [15]. However, hyperkeratosis, which was a predominant finding in the study by Prasad et al., was not observed in the present study [15].
Pityriasis Rubra Pilaris
In the present study, follicular plugging, follicular and perifollicular parakeratosis, acanthosis and dermal perivascular inflammation were the predominant findings which were similar to the findings in a study by White [16].
The predominant reaction patterns which were noted in the present study were psoriasiform and lichenoid reaction patterns. However, an attempt to categorise the lesions based on the tissue reaction patterns was not successful due to the considerable overlap in the histopathological features and absence of classical features in many cases. In a study by Costa et al., and Younas and Haque clinicopathological correlation carried out showed compatible clinical as well as histopathological diagnosis in 76.30% of the cases as against the present study [4,5]. In the present study, a total of 150 cases were analysed to assess the correlation between clinical and histopathological diagnoses. A concordance was observed in 46.67% (70 cases) and discordance in remaining 53.33% (80 cases) [Table/Fig-7].
The reason for the low concordance may be the following: In cases like psoriasis and lichen planus, where the tissue reaction patterns were classical, histopathological diagnoses confirmed the clinical diagnoses. But other conditions without classical patterns were ambiguous histopathologically, or diagnosed otherwise. There is a considerable overlap in the clinical presentation, due to which many cases clinically suspected as papulosquamous skin lesions turned out to be other conditions. In some early cases, clinical signs and symptoms may precede the presently known characteristic tissue changes, or vice versa. If a biopsy is taken at an early stage or from inappropriate site, there is likely to be discordance between clinical and histopathological observations. Selecting representative lesion is essential in establishing histopathological diagnosis. Although these cases were reported as untreated, the chances that some of these cases had taken treatment cannot be ruled out. The results may be affected partially by the effect of treatment.
Conclusion
Papulosquamous skin diseases show considerable overlap in clinical and histopathological features. Knowledge of the key histopathological features and a clinicopathological correlation will aid in making a specific diagnosis. In the present study, the age distribution pattern indicated the maximum cases in the age range of >60 years. Gender distribution pattern showed a male preponderance. The most frequently encountered lesion was psoriasis followed by lichen planus. In psoriasis the clinical presentations are misleading because of the varied clinical presentations. Psoriasis also presents with the problem of overlap. Histopathology serves as a tool and rules out the lesions that mimic psoriasis. Clinicopathological correlation helped most in psoriasis as against other non-infectious erythaematous papulosquamous skin diseases. This study showed a low concordance (46.6%) between clinical and histopathological diagnosis which throws light on the overlapping histopathological features and difficulties in arriving at a specific diagnosis.