Histopathological Trends of Testicular Neoplasm: An Experience over a Decade in a Tertiary Care Centre in the Malwa Belt of Central India
Preeti Rihal Chakrabarti1, Shilpi Dosi2, Amit Varma3, Priyanka Kiyawat4, Gaurav Khare5, Sandeep Matreja6
1 Assistant Professor, Department of Pathology, Sri Aurobindo Medical College and PG Institute, Indore, India.
2 Assistant Professor, Department of Pathology, Sri Aurobindo Medical College and PG Institute, Indore, India.
3 Professor and Head, Department of Pathology, Sri Aurobindo Medical College and PG Institute, Indore, India.
4 Junior Resident, Department of Pathology, Sri Aurobindo Medical College and PG Institute, Indore, India.
5 Junior Resident, Department of Pathology, Sri Aurobindo Medical College and PG Institute, Indore, India.
6 Junior Resident, Department of Pathology, Sri Aurobindo Medical College and PG Institute, Indore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Preeti Rihal Chakrabarti, Flat 404, Akanksha Apartments Saims HospitalCampus, Indore-452001, India.
E-mail: preetirihal@yahoo.co.in
Introduction
Testicular and para-testicular neoplasm are rare type of tumours affecting adolescents and young adults, reflected by the paucity of published data in India.
Aim
This study was undertaken to estimate the epidemiological characteristics and histological types and subtypes of testicular neoplasm according to the WHO classification in our patient group. Identification of histopathological pattern of testicular tumour is immensely important for improved management protocols.
Materials and Methods
This was a retrospective study done over a period of ten years from 2004 to 2014 in a tertiary care centre. All relevant clinical data including patient’s age, laterality, history of risk factors and serum tumour markers were collected from records. Histopathological slides were retrieved and reviewed for tumour and its subtype and classified according to WHO classification (2004).
Results
A total of 37 cases of testicular and paratesticular neoplasm were encountered in our study with a mean age of 38.1 years. Right testis was affected in 70.3% of cases. The most common clinical presentation was scrotal swelling with heaviness. Germ cell tumour was the most common type accounting for 77.1% followed by lymphomas (17.1%). Germ cell tumours were categorized into seminomatous (48.2%) and non-seminomatous tumours (51.8%). The most common subtype of non-seminomatous tumours was mixed germ cell tumour accounting for 85.8%.
Conclusion
The incidence of testicular neoplasm among general population in Asian countries is low, as reflected in the very few studies that have been performed and published in literature. Epidemiological and histomorphological spectrum of our study was comparable to most of the countries except for some African and Western countries.
Carcinoma testis, Germ cell tumor, Seminoma
Introduction
Testicular cancers comprise 1% of all the male cancers worldwide [1]. In developed countries, testicular neoplasms have been noted as most common solid tumour between the 2nd and 4th decade of life [2,3]. There are various risk factors for development of testicular cancers which include: a family history of testicular tumour in first degree relatives, infertility, cryptorchidism, Klinefelter’s syndrome and some other uncommon factors like trauma, hormones, etc [4]. Although testicular cancer can be derived from any cell type found in the testicles, more than 95% of testicular cancers arise from germ cells. The hypothesis behind the germ cell tumour is that the disease process begins in foetal life and comprises of abnormal proliferation of primordial germ cells [5,6].
In 2004, WHO has classified testicular and paratesticular neoplasms into various subgroups [7] and same were incorporated in present study. After an exhaustive literature search with keywords (testicular neoplasm, Germ cell tumour, Central India) revealed minimal number of studies from the Indian subcontinent and none from Central India region.
Aim
Hence, the purpose of our study was to report the trends and distributions of types and subtypes of testicular neoplasm in a Central India (Malwa region) population, comprising of all the male patients admitted for evaluation of testicular masses over the period of 10 years from December 2004 to January 2014.
Materials and Methods
This was a retrospective study of all testicular malignancies diagnosed in the Department of Pathology of tertiary care centre from 2004 to 2014. The histopathological slides were retrieved and reviewed. All clinically relevant data including patients age, laterality, history of risk factors and serum tumour markers was collected from the records. The tumours were classified according to WHO classification (2004) [7].
Results
Based on our archives, there were 37 histopathologically confirmed cases of testicular and paratesticular neoplasms over a study period of ten years. The mean age was 38.1 years with the age range of 1 to 80 years. More than 59% of cases occurred in 3rd and 4th decade [Table/Fig-1]. Twenty six (70.3%) of the tumours were on the right side and 11 (29.7%) were on left side. There was no bilateral involvement in our study.
Age wise distribution of testicular neoplasm (n=37).
| Age group(years) | Frequency | Percentage |
|---|
| 0-10 | 01 | 2.7% |
| 11-20 | 03 | 8.1% |
| 21-30 | 11 | 29.7% |
| 31-40 | 11 | 29.7% |
| 41-50 | 02 | 5.4% |
| 51-60 | 03 | 8.1% |
| 61-70 | 04 | 10.9% |
| 71-80 | 02 | 5.4% |
Scrotal swelling and heaviness was recorded in 29 cases and history of pain in 7 cases. A history of cryptorchidism was noted in 3 cases and family history of testicular neoplasm in 2 cases. Testicular atrophy was noted in 1 case. Preoperative assay of tumour marker showed elevated α-fetoprotein and β-human chorionic gonadotrophin levels in 10 (27.0%) and 6 cases (16.2%) respectively.
Out of total 37 cases, 35 (94.6%) cases were testicular and 2 (5.4%) were paratesticular neoplasm. Out of 35 testicular neoplasm, 27 cases (77.1%) were germ cell tumours, 6 cases (17.1%) were lymphomas, 1 case (2.9%) of mixed germ cell/sex cord stromal tumour and cavernous hemangioma each. Two cases of paratesticular neoplasm were reported as sarcomas [Table/Fig-2].
Main histological types of testicular and paratesticular tumours (n=37)
| S.No | Histological Type | No of cases | Percentage |
|---|
| 1 | Germ cell tumours | 27 | 73.0% |
| 2 | Lymphoma | 06 | 16.2% |
| 3 | Sarcoma | 02 | 5.4% |
| 4 | Others * | 02 | 5.4% |
*Mixed germ cell/Sex cord stromal tumour- 1, Cavernous hemagioma-1.
Of the germ cell tumours, 13 cases (48.2%) were seminomas and 14 cases (51.8%) were non-seminomas. The most frequent subtype of non-seminomatous tumour was mixed germ cell tumours accounting for 85.8% [Table/Fig-3]. The mean age for germ cell tumour was 32.4 years, with seminoma 37.9 years and for non-seminomatous tumour 27.5 years. Patient diagnosed with lymphomas had a mean age of 61.3 years.
Histological subtypes of germ cell tumour (n=27).
| S.No | Histological types and subtypes | No of cases | Percentage |
|---|
| 1 | Seminomatous | 13 | 48.2% |
| 2 | Non-Seminomatous | 14 | 51.8% |
| 3 | Embryonal carcinoma | 00 | 00 |
| 4 | Yolk sac tumour | 01 | 7.1% |
| 5 | Teratoma | 01 | 7.1% |
| 6 | Mixed germ cell tumour | 12 | 85.8% |
Discussion
There are less number of studies published in the past couple of years on testicular neoplasm in Asian countries, among them few were pertaining from India [8–10]. Testicular and paratesticular neoplasm are still relatively less as compared to other cancers, as it constitute 10.5% of all male reproductive cancers in India [11]. In present study, we found only 37 cases during ten year period with an average of 3.7 cases per year. There is a marked variation in the incidence of testicular neoplasm worldwide as western countries [12,13] showing a higher rate as compared to African [14,15] and Asian countries [4,10,16,17] [Table/Fig-4]. The high incidence in western countries is due to genetic factors, cryptorchidism, oestrogen rich diet and industrialization [4,18]. However, in present study lower incidence was observed due to lack of major risk factors like cryptorchidism as it accounted for 8.6% in our patient group. This is comparable with the finding of other workers, who found previous history of cryptorchidism in 10% of all testicular cancer patients, making it the single most important risk factor associated with testicular cancer [14].
Comparative study of average number of Testicular neoplasm per year in various countries.
| S.No | Study (year) | Country | Average no of cases per year |
|---|
| 1) | Horwich et al., (2013) [12] | England | 64.9 |
| 2) | Walschaerts et al., (2008) [13] | France | 53.2 |
| 3) | Chalya PL et al., (2014) [14] | Tanzania | 5.6 |
| 4) | Salako AA et al., (2010) [15] | South Western Nigeria | 1.5 |
| 5) | Deotra A et al., (1994) [10] | India (Rajasthan) | 5.5 |
| 6) | Mushtaq S et al., (2007) [16] | Pakistan | 21.4 |
| 7) | Present study (2016) | Central India (Malwa belt) | 3.7 |
In present study, peak age incidence was seen in 3rd and 4th decade of life which was in accordance with reports from African and European series [4,19]. Testicular neoplasm were more common on right side in present study, accounting for 70.3% which was similar to other studies [20,21]. Painless scrotal swelling was the most common clinical presentation in our patients irrespective of the histological types which was in accordance with other workers report [22].
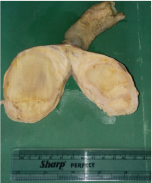
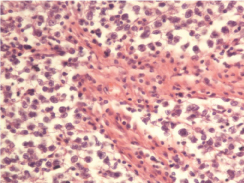
Testicular neoplasm of germ cell origin, constitute more than 95% of these tumours and it is the most common malignancy in men aged between 18-35 years [23]. We found 27 cases (73%) of germ cell testicular tumours with a mean age of 32.4 years. Out of these germ cell tumours, 13 cases (48.2%) were of seminomas with mean age of 37.9 years and 14 cases (51.8%) of non-seminomatous tumours with mean age of 27.5 years. This confirms the known younger age of patients with non-seminomatous tumours compared to seminomatous subtype [16,24,25]. Gross examination of seminomas, showed a well defined, creamish yellow homogenous firm mass, ranging from 4 to 10 cm. Microscopic examination revealed monotonous cell population divided into lobules by thin fibrovascular stroma [Table/Fig-5,6].
Gross photograph of seminoma showing a well defined, yellow homogenous testicular mass.
High power view showing monotonous tumour cells divided by thin fibrovascular septae (H & E- 400x).
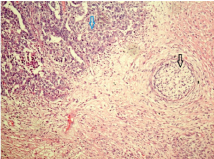
Among the non-seminomatous tumours, mixed germ cell tumour was the most frequent subgroup accounting for 85.8% followed by yolk sac tumour and teratoma. The predominance of mixed germ cell tumours among non-seminomatous tumours have also been reported in Turkey [26]. However, in another study from Ilorin, Nigeria yolk sac tumour was the most common subtype [27]. The most common combination in our study was teratocarcinoma (teratocarcinoma with embryonal carcinoma) accounting for 6/12 cases (50%) followed by 4/12 cases (33.3%) of teratocarcinoma with yolk sac tumour and 2/12 cases (16.7%) of seminoma with yolk sac tumour. Our findings were in accordance with previous study in which teratocarcinoma was commonest subtype [10]. Gross examination of most of the teratocarciomas revealed variegated appearance ranging from 5.5 to 11 cm in diameter. Microscopic examination revealed mostly teratomatous and embryonal carcinomatous elements [Table/Fig-7,8].
Scanner view of mixed germ cell tumour showing teratomatous (black arrow) and embryonal carcinomatous (blue arrow) component. (H & E- 40x).
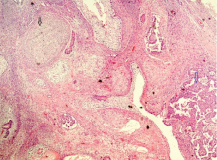
Low power view of mixed germ cell tumour showing teratomatous (black arrow) and embryonal carcinomatous (blue arrow) component. (H & E- 100x).
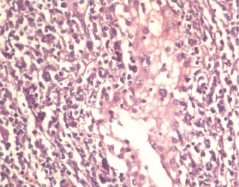
Primary malignant lymphomas of testis are rare and constitute about 5% of all testicular neoplasm [28]. In present study, other than germ cell tumour, lymphomas were the next most common tumour constituting about 16.2% with mean age of 61.3 years. These findings were in accordance with the series from Pakistan which showed Non Hodgkin’s lymphoma were quite frequent, which was reason for second peak in over 60 year’s age group [16,29]. Gross examination of lymphomas revealed mostly fleshy, cream tan, homogenous mass ranging from 7 to 10 cm in diameter. Microscopic examination showed round to oval tumour cells with visible nucleoli in few, predominantly infilterating the interstitium, with involvement of few seminiferous tubules [Table/Fig-9,10].
Gross photograph of lymphoma showing a well defined, tan homogenous testicular mass.

High power view of lymphoma showing tumour cells with prominent nucleoli in few, infiltrating the interstitium and few seminifereous tubules. (H & E- 400x).
Two cases of paratesticular neoplasm were reported in present study, with age of 35 and 80 years respectively. Both cases were histologically proved as leiomyosarcomas. Leiomyosarcoma is relatively common sarcoma of the paratesticular area, especially in adults with age range from 15 to 84 years [30,31]. In contrast to our study, rhabdomayosarcomas were most common variety of paratesticular neoplasm in a study from south western Nigeria [15].
Conclusion
The incidence of testicular neoplasm still remains low in India which is reflected by the paucity of studies in published literature. Germ cell tumours accounted for highest percentage of cases with a commonest subtype of seminoma followed by mixed germ cell tumour. Only one case was reported as benign in present study, which highlights that any testicular swelling should be evaluated thoroughly with clinicopathological correlation to rule out malignancy.
*Mixed germ cell/Sex cord stromal tumour- 1, Cavernous hemagioma-1.
[1]. Purdue MP, Devesa SS, Sigurdson AJ, McGlynn KA, International patterns and trends in testis cancer incidenceInt J Cancer 2005 15:822-27. [Google Scholar]
[2]. Power DA, Brown RS, Brock CS, Trends in testicular carcinoma in England and wales, 1971-1999BJU Int 2001 87:361-65. [Google Scholar]
[3]. Muir CS, Nectoux J, Epidemiology of cancer of the testis and penisNational Cancer Institute Monographs 1979 53:157-64. [Google Scholar]
[4]. Sagalowsky Al, Current consideration in the diagnosis and initial treatment of testicular cancerCompr Ther 1994 20:688-90. [Google Scholar]
[5]. Bray F, Richiardi L, Pukkala E, Cuninkova M, Moller H, Trends in testicular cancer incidence and mortality in 22 European countries: continuing increase in incidence and decline in mortalityInt J Cancer 2006 188:3099-111. [Google Scholar]
[6]. Mcglynn KA, Devesa SS, Graubard BI, Castle PE, Increasing incidence of testicular germ cell tumours among black men n the united statesJ Clin Oncol 2005 23:575-61. [Google Scholar]
[7]. Eble JN, Sauter G, Epstein JI, Pathology and genetics of tumours of the urinary system and male genital organs 2004 LyonIARC Press [Google Scholar]
[8]. Nerli RB, Ajay G, Shivangouda P, Pravin P, Reddy M, Pujar VC, Prepubertal testicular tumours: Our 10 years experienceIndian J Cancer 2010 47:292-95. [Google Scholar]
[9]. Patel MB, Goswami HM, Parikh UR, Mehta N, Histo-pathological study of testicular lesionsGujrat Med J 2015 70:41-46. [Google Scholar]
[10]. Deotra A, Mathur DR, Vyas MC, A 18 year study of testicular tumours in Jodhpur, western RajsatanJ Postgrad Med 1994 40:68-70. [Google Scholar]
[11]. Takiar R, Kumar S, Pattern of reproductive cancers in IndiaAsian Pac J Cancer Prev 2014 15:599-603. [Google Scholar]
[12]. Horwich A, Nicol D, Huddart R, Testicular germ cell tumoursBMJ 2013 347:5526 [Google Scholar]
[13]. Walschaerts M, Huyghe E, Muller A, Doubling of testicular cancer incidence rate over the last 20 years in southern FranceCancer Causes Controls 2008 19:155-61. [Google Scholar]
[14]. Chalya PL, Simbila S, Rambau PF, Ten- year experience with testicular cancer at a tertiary care hospital in a resource-limited setting: a single centre experience in TanzaniaWorld Journal of Surgical Oncology 2014 12:356-63. [Google Scholar]
[15]. Salako AA, Onakpoya UU, Osasan SA, Omoniyi-Esan GO, Testicular and paratesticular tumours in south western NigeriaAfr Health Sci 2010 10:14-17. [Google Scholar]
[16]. Mustaq S, Jamal S, Mamoon N, The pathological spectrum of malignant testicular tumours in northern PakistanJ Pak Med Assoc 2007 57:499-501. [Google Scholar]
[17]. Stewart BW, Kleihues P, Cancers of the male reproductive tractIn: World cancer report 2003 Lyon, FranceIARC Press [Google Scholar]
[18]. Oliver RTD, Testicular cancerCurr Opin Oncol 2001 13:191-98. [Google Scholar]
[19]. Richiardi L, Bellocco R, Adami HO, Torrang A, Barlow L, Hakulinen T, Testicular cancer incidence in eight northern European countries: secular recent trendsCancer Epidemol Biomarkers Prev 2004 13:2157-66. [Google Scholar]
[20]. Bhatti AB, Ahmed I, Ghauri RK, Clinical profile, treatment and survival outcome of testicular tumours: a Pakistani perspectiveAsian Pac J Cancer Prev 2014 15:277-80. [Google Scholar]
[21]. Miki T, Kamoi K, Fujimoto H, Clinical characteristics and oncological outcomes of testicular cancer patients registered in 2005 and 2008: the first large-scale study from the Cancer Registeration Committee of the Japanese urological associationInt J Urol 2014 21:1-6. [Google Scholar]
[22]. Gill MS, Shah SH, Soomro IN, Kayani N, Hasan SH, Morphological pattern of testicular tumourJ Pak Med Assoc 2000 50:110-13. [Google Scholar]
[23]. Shanmugalingam T, Soultati A, Chowdhury S, Rudman S, Van Hemelrijck M, Global incidence and outcome of testicular cancerClin Epidemiol 2013 5:417-27. [Google Scholar]
[24]. McGlynn KA, Devasa SS, Sigurdson AJ, Trends in the incidence of of testicular germ cell tumours in the Unites statesCancer 2003 97:63-70. [Google Scholar]
[25]. Ruf CG, Isbaran H, Wagner W, Changes in the epidemiological features of testicular germ cell cancer: age at diagnosis and relative frequency of seminomas are constantly and significantly increasingUrol Oncol 2014 32:33 [Google Scholar]
[26]. Ozgun A, Karagoz B, Tuncel T, Clinicopathological features and survival of young Turkish patients with testicular germ cell tumoursAsian Pac J Cancer Prev 2013 14:6889-92. [Google Scholar]
[27]. Izegbu MC, Ojo MO, Shittu LAJ, Clinico-pathological patterns of testicular malignancies in Ilorin, Nigeria- a report of 8 casesJ Cancer Res Ther 2005 1:229-31. [Google Scholar]
[28]. Sussman EB, Hajdu SI, Lieberman PH, Malignant lymphoma of testis: a clinicopathologic study of 37 casesJ Urol 1977 118:1004-07. [Google Scholar]
[29]. Jamal S, Moghal S, Mamoon N, Mushtaq S, Luqman M, Anwar M, The pattern of malignant tumours: tumour registry data analysis, AFIP, Rawalpindi, Pakistan(1992-2001)J Pak Med Assoc 2006 56:359-62. [Google Scholar]
[30]. Soosay GN, Parkinson MC, Paradinas J, Paratesticular sarcomas revisited: a review of cases in the British Testicular Tumour RegistryBr J Urol 1996 77:143-46. [Google Scholar]
[31]. Fisher C, Goldblum JR, Epstein JI, Leiomyosarcomas of the paratesticular region: a clinocopathologic studyAm J Surg Pathol 2001 25:1143-49. [Google Scholar]