First Branchial Arch Fistula: A Rarity and a Surgical Challenge
J.S. Rajkumar1, Deepa Ganesh2, J.R. Anirudh3, S. Akbar4, Niraj Joshi5
1 Chairman & Advanced Laparoscopic Surgeon, Department of Minimal Access Surgery, LifeLine RIGID Hospitals, Kilpauk, Chennai, India.
2 Consultant Laparoscopic Surgeon, Department of Minimal Access Surgery, LifeLine RIGID Hospitals, Kilpauk, Chennai, India.
3 Assistant Surgeon, Department of Minimal Access Surgery, LifeLine RIGID Hospitals, Kilpauk, Chennai, India.
4 Assistant Surgeon, Department of Minimal Access Surgery, LifeLine RIGID Hospitals, Kilpauk, Chennai, India.
5 Consultant ENT Surgeon, Department of ENT, LifeLine RIGID Hospitals, Kilpauk, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepa Ganesh, 51 A Medavakkam Tank Road, Kilpauk Chennai-600010, India.
E-mail: drdeepa@gmail.com
Although 2nd Branchial arch fistulae (from incomplete closure of Cervical sinus of His) are well known, 1st arch fistulae are much rarer (<10%) and are usually not tackled comprehensively. We present a case of a rare first branchial arch fistula of the type II Arnot classification, which presented with two external openings of more than 20 years duration. Patient had a successful resection of all the concerned fistulous tract. Review of literature and the surgical challenges of the procedure are presented herewith.
Arnot type II, Branchial anomaly, Branchial fistula, Facial nerve
Case Report
A 29-year-old lady presented with long standing and recurrent openings in the neck and below the ear lobe on the right side, which had been discharging pus for the past 20 years. She had seven procedures in the past, on both the openings, with an immediate recurrence within a few months. There was no other significant history pertinent to the head and neck of the patient. Examination revealed no other congenital anomalies. There was an area in the right submandibular triangle that was extensively scarred and was found to have the external opening of a fistula in it. There was also a separate external opening with hypertrophic scar tissue about 2cm below and behind the tip of the right ear lobe. Apart from these rest of the head and neck examination was normal apart from a tender submandibular and parotid gland area, presumably in relation to the track of pus. Rest of the examination was normal. A first branchial arch fistula, of Arnot type II was diagnosed.
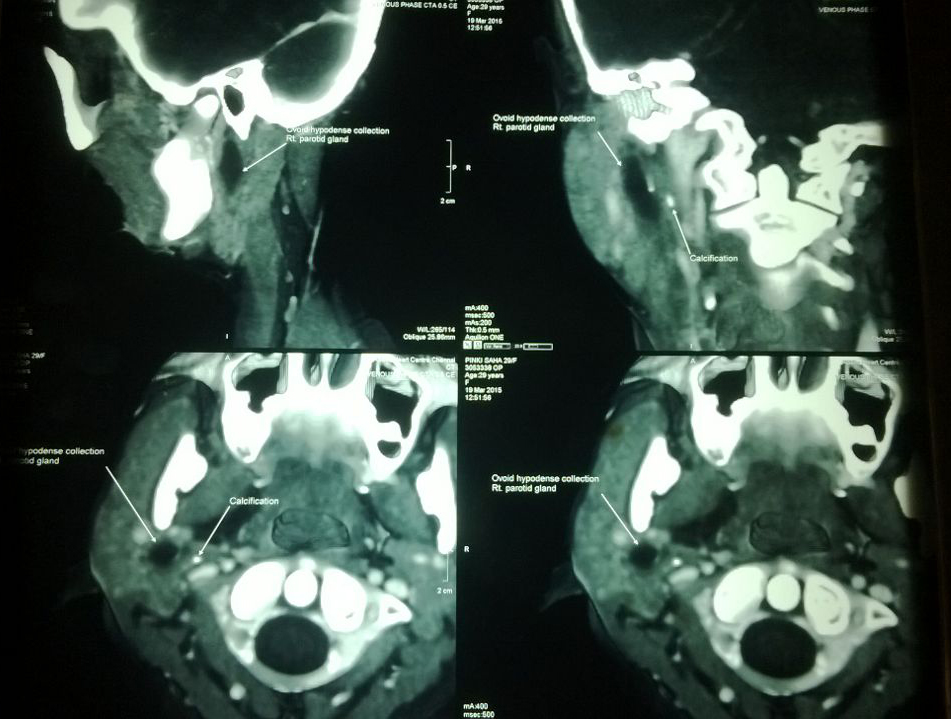
Confirmation was done using a CT fistulogram which showed the following: 1) A fistula going from the external opening in the submandibular triangle, superficial to the submandibular gland and going towards the deep lobe of the parotid and ending in an ovoid collection of Purulent material in relation to the deep lobe of the parotid gland. There was no obvious fistula communication to the oral cavity; 2) A separate tract running from below and lateral portion of the ear lobe towards the mastoid and stopping as a blind tract in relation to the external acoustic canal [Table/Fig-1,2 and 3]. Rest of investigations was normal. Based on the above CT fistulogram findings, double tract fistula of the type II Arnot classification of first branchial arch anomalies was diagnosed. After warning the patient about possible facial nerve injury and obtaining informed consent, we proceeded with exploration using the following technique.
A fistula going from the external opening in the submandibular triangle.
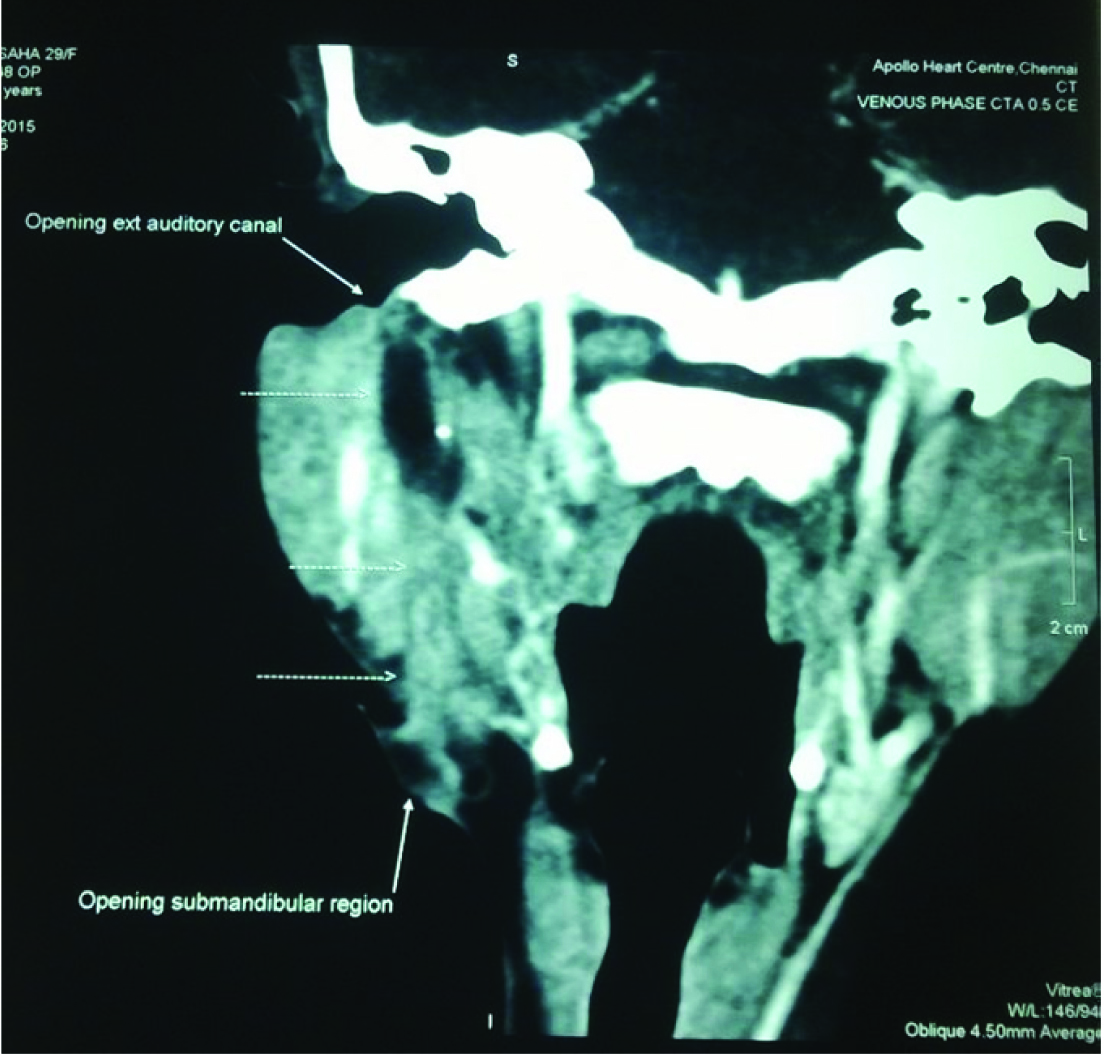
A separate tract running from below and lateral portion of the ear lobe towards the mastoid.
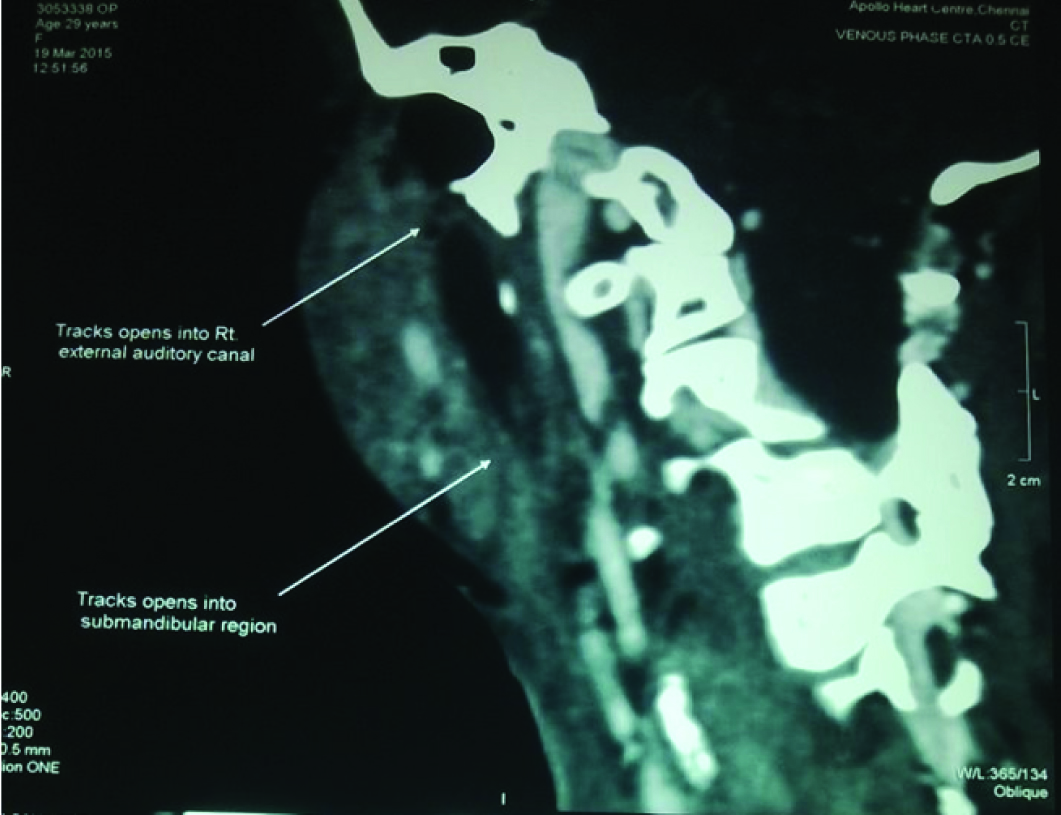
CT fistulogram ℓ Sagittal and coronal view showing extent of the fistula.
Technique
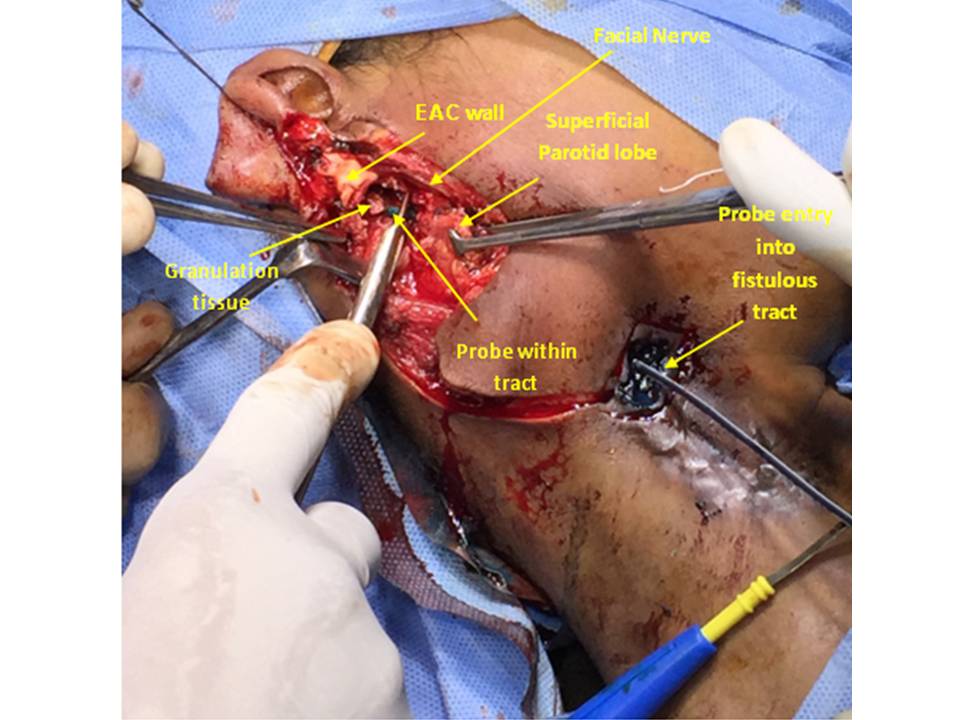
After cervico-facial draping, we first began by excising the area of the external openings and tracking both sinuses inwards. The posterior sinus ended blindly in relation to the external acoustic canal, about 2cm medial to the external acoustic meatus. There was no obvious myringoid web going from there towards the base of the tympanum. We excised the submandibular sinus for about 3-4cms after including the sinus scar in an elliptical incision that excised the hypertrophic scar with it. Raising a sub-platysmal flap to avoid injury to the marginal mandibular branch of the facial nerve we proceeded with the dissection until the parotid was reached. At this point of time the dissection was shifted to the pre auricular region where a modified incision was made and the vertical limb of the incision was joined in a Lazy ‘S’ to the transverse limb which included the submandibular sinus opening. The vertical limb was extended with the suture in the ear lobe giving traction, until the tragus was made out. The tragus was used as a pointer and the facial nerve was dissected out in the stylomastoid foramen. We then proceeded to dissect out the bifurcation of the facial nerve into its cervico-facial and zygomatico temporal branches. Extensive oedema was seen in relation to the facial nerve in this area. Injection of methylene blue was done in the submandibular sinus and this continued and spilled into the deep lobe area of the parotid. Using the methylene blue as a track and using the facial nerve as a plane of avoidance, we managed to curette, cauterize and excise as much of the deep fistulous tract as possible [Table/Fig-4]. When it was completely washed out, curetted and cauterized (the deeper few centimeters) the wound was closed in layers. A cervical advancement flap was not necessary to close the skin. Mere undermining of the platysmal tissue allowed us to get a good closure. The wound was closed with drainage, the patient made a smooth post operative recovery. Histopathology of the excised fistula showed a fistula lined by squamous epithelium (both posterior and anterior tracts), and with some columnar epithelium in the deeper aspect of the anterior tract). The findings were commensurate with a first branchial arch fistula.
Fistulous tract being probed avoiding the facial nerve.
Discussion
The common branchial cyst and branchial fistula pertain to imperfect closure of the endobranchial cleft (2nd to 5th branchial arches). Much rarer is a true first branchial arch fistula, in which there is failure of closure of the first branchial cleft itself. These results in two types of external openings, one in relation to the External Acoustic Canal (EAC) and another one in relation to the Submandibular Gland (SMG). There is a relatively paucity of literature on this rare condition, which is associated with specific surgical technical issues during the operation, especially in relation to the facial nerve branches. This case report highlights these technical snippets and reviews the available literature.
Compared to the classical branchial fistula with its opening the lower end of the anterior order of the sternomastoid, the first branchial arch fistulae present in the submandibular triangle [1]. The Pochet’s triangle is the triangle between the submental area, the hyoid bone, and the mastoid process. Any fistulous opening in this area should raise the possibility of a first branchial arch fistula [2]. Our patient had seven surgeries without a deeper exploration, a tragedy which could well have been avoided if the Pochet’s triangle opening had been kept in mind.
Much rarer than their counter parts lower down, first branchial arch fistulas have been extensively studied and classified by several authors. Arnot et al., divided the first branchial arch fistula into two types, type I and type II, the first being only posterior fistulas with communication, with the external acoustic canal with predominantly ectodermal component [3]. Type II is classified as one with anterior and posterior component and with an ectodermal and mesodermal component, with one track draining towards the deep lobe of parotid and a separate one draining towards the external acoustic canal, exactly like our patient had. In addition a small proportion of type II Arnot fistulae also have what is known as a myringoid web, a web of tissue that runs from the blind ending of the sinus towards the mesotympanum and the middle ear [4–6]. Our patient did not have this extension, which might have engaged us in some more middle ear dissection.
The first branchial arch starts developing from the 4th week of an intrauterine life and during this period the parotid and the facial nerve are also in the process of development. The facial nerve in particular has a very close relationship to the deeper aspect of the first branchial arch fistula. 37% of the fistulae are found to go medial to the facial nerve, as it was in our case [3,7]. A 22% of fistulae go laterally and in 31% the facial nerve is enmeshed within the fistulae with the branches of facial nerve. In the last variety injury to the facial nerve is very common [8]. One does not know about the orientation of the fistula in relation to the facial nerve until one has started the dissection process and this is why it is important to obtain informed consent about possible facial nerve damage. Fortunately in our case we could establish a clear plane of a facial nerve branches and we could establish that the fistula run separately and deep to this plane. GR Ford and Balakrishnan have reviewed the literature on first branchial arch fistulae and their suggestion is to dissect out the facial nerve branches primarily [9], as this is the structure that is most in danger to damage by the excision. We followed this technique and primarily dissected out the facial nerve at the stylomastoid foramen with its bifurcation and its major branches. All other dissection of the fistula is secondary to facial nerve damage, the only irreparable on slaught by the surgeon.
In our particular patient the dense inflammatory adhesion between the deeper parts of the parotid and the fistula made us worry about possible facial nerve injury in the upper median plane. Therefore we opted to proceed with a hybridized version of fistula resection. We resected as much of the fistula as possible and in the blind areas instead of trying a blind resection of entire fistulous tract, we washed out the fistula, cauterized the lining of the fistula with bipolar diathermy, and with mechanical curetting followed by washout with hydrogen peroxide. This attack of the lined epithelial track fistulas with direct mechanical fulguration as well as thermal fulguration with or without chemical fulguration is typical of the newer less conservative approach to fistulas, which a number of authors have used with high degree of success for complicated fistulas in ano.
First branchial arch fistulas are a rare type of endocervical (less than 10%) branchial arch anomalies, with specific challenges [10], especially in relation to the facial nerve branches and to the parotid gland. This rather difficult diagnosis has been made easier using a CT fistulogram which is the investigation of choice for this condition [11]. We would like to reiterate that detailed dissection of the facial nerve and his branches will prevent damage to them during the repair of fistula. We would also like to recommend hybrid modalities of dealing with the deepest aspect of the fistula, like cauterization of the epithelial lining tract using bipolar cautery. Review of the literature of this rare disease has been done.
Conclusion
The challenges of dealing with a first branchial arch fistula have been elaborated here, with a case report of type II Arnot variety. Avoiding injury to the facial nerve is of paramount importance and early identification and preservation of the nerve and branches, prior to fistula dissection may help surgeons avoid a catastrophe. Another learning point is that cauterization of the fistula may help healing without damage to adjacent structures like the facial nerve.
[1]. Olsen KD, Maragos NE, Weiland LH, First branchial cleft anomaliesLaryngoscope 1981 91:423-36. [Google Scholar]
[2]. Somashekara KG, Sudarshan Babu K, Lakshmi S, ℓ Type II First branchial cleft cyst: a case report with review of literatureIndian J Otolaryngol Head Neck Surg 2111 63(Suppl 1):75-77. [Google Scholar]
[3]. Arnot RS, Defects of the first branchial cleftS Afr J Surg 1971 9(2):93-98. [Google Scholar]
[4]. Violaris NS, Pahor AL, A variation of first branchial cleft ℓThe Journal of Laryngology & Otology 1993 117(17):625-26. [Google Scholar]
[5]. Bill AH, Vadheim JL, Cysts, sinuses and fistulas of the neck arising from the first and Second branchial cleftsAnnals of Surgery 1955 142:555-61. [Google Scholar]
[6]. Prabhu V, Ingrams D, First branchial arch fistula: diagnostic dilemma and improvised surgical managementAmerican Journal of Otolaryngology 2111 32(6):617-19. [Google Scholar]
[7]. Miller PD, Corcoran M, Hobsley M, Surgical excision of first cleft branchial fistulaeBritish Journal of Surgery198471(9):696-97. [Google Scholar]
[8]. Liston SL, The relationship of the facial nerve and first branchial cleft anomalies ℓ Embryologic considerations ℓThe Laryngoscope 1982 92:1318-11. [Google Scholar]
[9]. Ford GR, Balakrishnan A, Evans JNG, Branchial cleft and pouch anomalies-The Journal of Laryngology & Otology 1992 116(12):137 [Google Scholar]
[10]. Aronsohn RS, Batsakis JG, Anomalies of the first branchial cleftArchives 1976 [Google Scholar]
[11]. Whetstone J, Branstetter BF, Fluoroscopic and CT fistulography of the first Branchial cleftAJNR Am J Neuroradiol 2116 27(9):1817-19. [Google Scholar]