Sebaceous Gland Carcinoma of the Lower Eyelid Reconstructed with a Composite Flap: A Case Report
Surya Rao Rao Venkata Mahipathy1, Alagar Raja Durairaj2, Kanmani Kothandaraman3, Vimal Chander Rajamanohar4, Aarthi Prabakaran5
1 Associate Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
2 Associate Professor, Department of Plastic and Reconstructive Surgery, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
3 Professor, Department of Ophthalmology, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
4 Assistant Professor, Department of Pathology, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
5 Resident, Department of Ophthalmology, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surya Rao Rao Venkata Mahipathy, Associate Professor, Department of Plastic & Reconstructive Surgery, Saveetha Medical College & Hospital, Thandalam, Kanchipuram-602105, India.
E-mail: surya_3@hotmail.com
Sebaceous gland carcinomas are skin adnexal tumours occurring in the periocular region of elderly females. It is an uncommon malignancy usually involving the upper eyelid and has an indolent course. Mainstay of treatment is surgical excision. Here we present a case of a sebaceous gland carcinoma of the lower eyelid for which wide local excision was done and the lower eyelid reconstructed using a composite flap of nasal chondromucosal graft with a nasolabial flap.
Rare, Skin adnexal tumour, Surgery
Case Report
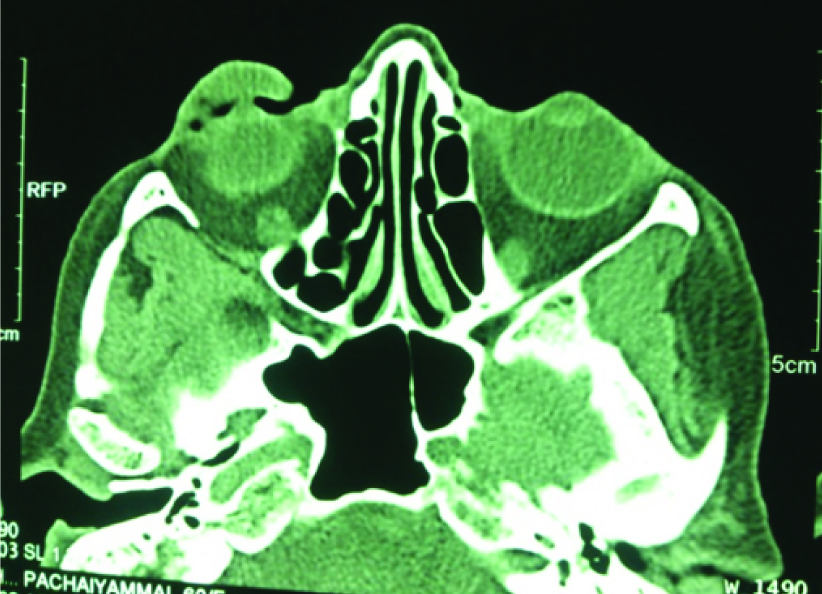
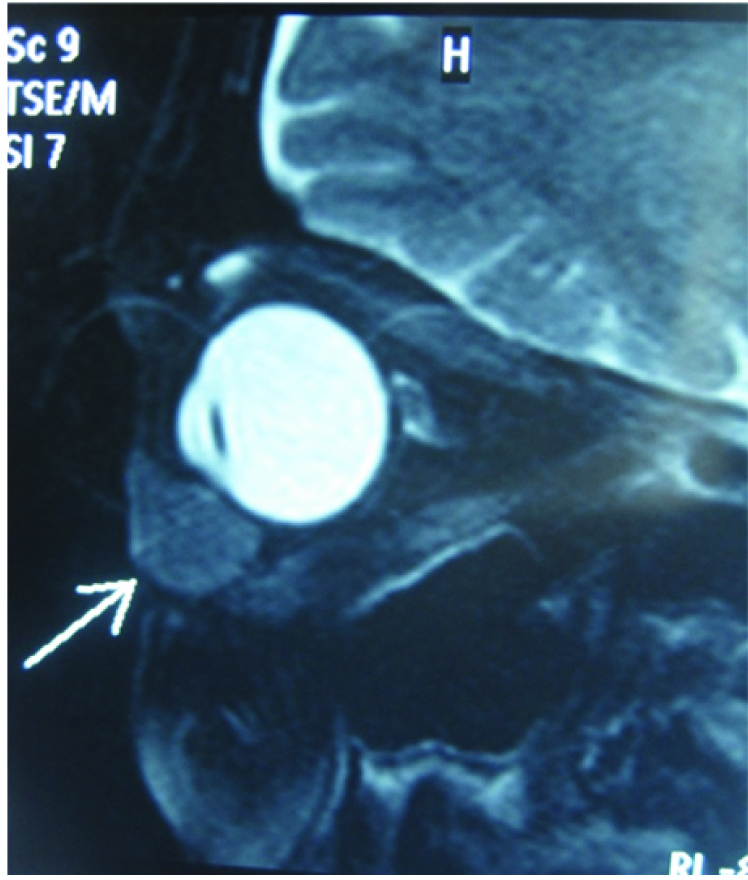
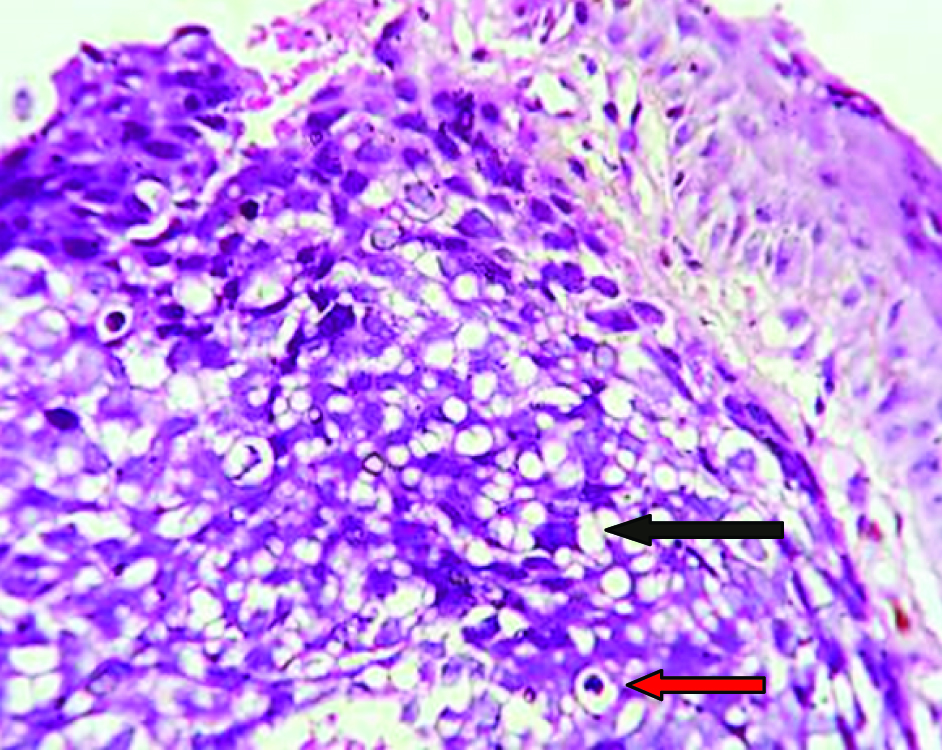
A 60-year-old female presented with a swelling of the right lower eyelid for the past 3 years. The swelling initially started as a small nodule and progressively increased in size for the past 3 years to attain the present size of about 20x15 mm [Table/Fig-1]. It was painless with no ulceration, bleeding, discharge or watering of the eyes. She complained of difficulty in vision and irritation of the right eye. She gave history of cataract surgery to the right eye 3 years ago done elsewhere. Ophthalmologic examination of the right eye showed clear conjunctiva and cornea with a deep anterior chamber and pseudophakia. Fundoscopy revealed clear media, cupping and peripapillary atrophy of the disc with normal vessels and a dull foveal reflex. On examination of the right lower eyelid, a nodulo-proliferative swelling of size approximately 20x15 mm extending superiorly from the lower eyelid margin and inferiorly underneath the palpebral conjunctiva with a smooth surface and well defined margins and firm in consistency [Table/Fig-2]. Vascularity was seen over the surface of the swelling. CT scan of the right eye lower lid region showed an irregular hypodense mass like lesion of size 2.6x1.7 cm (HU 41) with extension medially into inner canthus with no architectural distortion or underlying bony erosion [Table/Fig-3]. MRI revealed a well defined ovoid homogeneous lesion (22x16x39mm) along the lower eyelid of right orbit with hypointense signals on both T1 and T2 weighted images abutting the anteroinferior aspect of the right eyeball but with no infiltration [Table/Fig-4], the probable diagnosis being fibrous tumour of eyelid or chronic inflammatory lesion. Incisional biopsy showed stratified squamous epithelium with focal atypia and underlying stroma showing a neoplasm composed of lobules of malignant cells with moderate eosinophilic to multivacuolated cytoplasm and moderately pleomorphic and hyperchromatic nuclei with indentation. Focal areas of necrosis and infiltration of tumour cells into stroma surrounded by chronic inflammatory cells was present, the features suggestive of sebaceous carcinoma [Table/Fig-5]. Surgery was planned and proceeded with wide local excision of the lesion with skin, tarsal plate and conjunctiva with a 5mm margin and the resulting defect [Table/Fig-6] was covered with a composite nasal chondromucosal graft for lining [Table/Fig-7] and a superiorly based nasolabial flap for cover [Table/Fig-8]. Patient was comfortable in the postoperative period with no pain, bleeding or epiphora [Table/Fig-9] and the sutures removed on the 7th postoperative day. The flap settled well and the patient was discharged on 14th postoperative day [Table/Fig-10] and was on regular follow-up for recurrence. Histopathology revealed sebaceous gland carcinoma with free margins all around.
Clinical photograph showing the lesion obstructing vision in the right eye.

Photograph showing the noduloproliferative lesion in the right lower eyelid.

CT showing an irregular hypodense mass of the right lower eyelid.
MRI reveals a well defined ovoid homogeneous lesion along the lower eyelid of right orbit with hypointense signals on both T1 and T2 weighted images abutting the anteroinferior aspect of the right eyeball but with no infiltration.
Histopathology revealed stratified squamous epithelium with focal atypia and underlying stroma showing a neoplasm composed of lobules of malignant cells with moderate eosinophilic to multivacuolated cytoplasm (black arrow) and moderately pleomorphic and hyperchromatic nuclei (red arrow) with indentation.
Defect after wide local excision with 4 mm margin.

Nasal septal chondromucosal graft harvested for posterior lamella.
Superiorly-based nasolabial flap raised for anterior lamella.

Immediate postoperative picture.

2 weeks postoperative picture.

Consent
A written informed consent was obtained from the patient for publication of the images.
Discussion
Sebaceous Gland Carcinomas (SGC) are rare, slow growing skin adnexal tumours commonly arising in the periocular region. It constitutes about less than 5% of eyelid malignancies and has been considered to be the third most common eyelid malignancy following basal cell and squamous cell carcinomas. They arise from either the meibomian glands, glands of Zeis or glands in the region of the caruncle [1]. It usually occurs in elderly females with an increased incidence of local recurrence, regional and distant metastases [2]. It is unique that it has a multifocal origin with pagetoid spread. Sebaceous glands are located in the dermis of periocular skin, tarsal plate, caruncle, and eyebrow skin follicles. Glands of Zeis are modified, sebaceous glands that are found at the base of the eyelashes. Sebaceous gland carcinoma is frequently encountered in the upper eyelid due to the abundance of meibomian glands [3,4].
There are two main pathological types of the SGC - nodular and spreading. The nodular form occurs as a well circumscribed hard nodule with adipose deposits in the region of the upper tarsal plate and is generally known for its multicentricity. The spreading variety of SGC presents as a diffuse involvement of the eyelid margin, loss of eyelashes and resembles other benign conditions like chronic blepharoconjunctivitis. It spreads in pagetoid form [5,6] with diffuse intraepithelial infiltration of the eyelid skin of both the eyelids and conjunctival epithelium [5,7,8]. A rare form of SGC called Muir–Torre syndrome is characterized by squamous metaplasia of the tumour, multiple sebaceous adenomas or carcinomas in the skin, and visceral malignancies.
Histopathology shows large anaplastic cells with hyperchromatic nuclei and foamy cytoplasm due to lipid vacuoles, which is classical of sebaceous carcinoma. The cells stain positive for lipid such as oil red O stain. Another characteristic feature is the spread of the tumour as infiltrating nests, cords or lobules as well as spread superficially within the epithelium. Sebaceous gland carcinoma is invasive when there is hyperexpression of p53 on molecular biology.
The tumour can metastasize by either direct, lymphatic, or haematogenous spread. The most common sites of metastasis are orbit, preauricular and submandibular lymph nodes and parotid gland. It masquerades as a benign condition and therefore there is a delay in diagnosis, and this causes increased morbidity and mortality rates [9]. The literature reported a mortality of about 6% [6].
Various treatment modalities are available depending on the stage of presentation of the tumour. Mainstay is surgical excision with or without neck dissection and orbital exentration in advanced disease. Radical surgical excision with a 4mm tumour free margin is the treatment of choice. Moh’s micrographic surgery is a more effective method of treatment. Approximately, 30% of SGCs recur after resection [10,11]. There is a high rate of metastasis (41%) [3,6].
Full-thickness loss of the eyelid require the reconstruction of the anterior lamella which is made of skin, subcutaneous tissue, orbicularis muscle and the posterior lamella containing the tarsal plates and palpebral conjunctiva [12,13]. The lower tarsus is a dense conjunctive structure which gives rigidity and stability to the eyelid [13], and containing the meibomian glands, which secrete a sebaceous material needed for lubricating the cornea [12,14].
Tumours invading the tarsal plate cause full thickness defects of the eyelid. Defects of up to one-third of the total length of the lower eyelid are capable of being closed primarily. Larger tumours require surgical reconstruction through the preparation of flaps and with or without grafts [15,16]. There are many options to reconstruct the posterior lamella such as jugal mucosa grafts, mucosal grafts from the hard palate [17,18], chondro-mucosal grafts from the nasal septum [18]. The presence of a free tissue graft in the posterior lamella requires a vascularised flap for the anterior lamella.
The nasolabial flaps are very useful and versatile local flap with robust vascularity that can be readily elevated as a superior, inferior, medial and lateral flaps without any delay due to rich sub dermal plexus first described by Sushruta in 600 BC [19]. The flap is aesthetically better as the scar is concealed in the nasolabial groove. Superiorly based nasolabial flaps are used to reconstruct defects of lower part of the nose, lower eyelid, and the cheek. The advantages of using the nasolabial flap is that it has a good vascularity, quick with simple technique, excellent colour and texture match and the use of hairless skin. The disadvantage of the superiorly based nasolabial flap is the trapdoor or pincushion effect caused by scar contracture, loss and asymmetry of the nasolabial sulcus.
Local nodal disease without distant metastasis is treated by radical neck dissection [6]. Topical mitomycin C [20], cryotherapy and proton electron irradiation has been tried for sebaceous gland carcinoma of the eyelid but with poor results [11,21]. Radiotherapy has been tried as a primary form of therapy with variable results [6,21,22]. Radiation is advised for poor surgical candidates due to advanced age or disease, for palliation, and in patients who refuse exenteration for advanced local disease.
The overall mortality rate is 6–11% because of delay in the diagnosis and treatment. The mortality from metastasis may go up to 30%. Involvement of upper or both eyelids and tumour size of more than 10 mm, duration of symptoms more than 6 months (mortality 35%), poorly differentiated and anaplastic tumours, haematogenous and lymphatic spread, orbital extension, multicentricity and pagetoid spread are poor prognostic factors. Tumours less than 6mm and those arising from glands of Zeis are more favourable.
Conclusion
Sebaceous gland carcinoma is a rare tumour which masquerades as benign ocular conditions and hence requires the clinician to identify the tumour and institute early surgical therapy due to the aggressive nature of the tumour.
[1]. Buitrago W, Joseph AK, Sebaceous carcinoma: The great masquerader: Emerging concepts in diagnosis and treatmentDermatol Ther 2008 21:459-66. [Google Scholar]
[2]. Straatsma BR, Meibomian gland tumoursArch Ophthalmol 1956 56:71-93. [Google Scholar]
[3]. Ni C, Kou PK, Meibomian gland carcinoma: A clinico-pathological study of 156 cases with long-period follow up of 100 casesJpn J Ophthalmol 1979 23:388-401. [Google Scholar]
[4]. Rao NA, Hidayat AA, Mclean IW, Zimmerman LE, Sebaceous carcinomas of the ocular adnexa: A clinico-pathological study of 104 cases, with five year follow up dataHuman Pathol 1982 13:113-22. [Google Scholar]
[5]. Zurcher M, Hinstchich CR, Garner A, Bunce C, Collin JR, Sebaceous carcinoma of the eyelid: A clinicopathological studyBr J Ophthalmolo 1998 82:1049-55. [Google Scholar]
[6]. Shields JA, Demirci H, Marr BP, Eagle RC, Jr, Shields CL, Sebaceous carcinoma of the eyelids: Personal experience with 60 casesOphthalmology 2004 111:2151-57. [Google Scholar]
[7]. Sweebe EC, Cogan DG, Adenocarcinoma of the meibomian gland; a pseudochalazion entityArch Ophthalmol 1959 61:282-90. [Google Scholar]
[8]. Russell WG, Page DL, Hough AJ, Rogers LW, Sebaceous carcinoma of meibomian gland origin. The diagnostic importance of pagetoid spread of neoplastic cellsAm J Clin Pathol 1980 73:504-11. [Google Scholar]
[9]. Cook BE, Bartley GB, Treatment options and future prospects for the management of eyelids malignancieOpthalmolgy 2001 108:2088-98. [Google Scholar]
[10]. Ginsber J, Present status of Meibomian gland carcinomaArch Ophthalmol 1965 73:271-77. [Google Scholar]
[11]. Epstein GA, Putterman AM, Sebaceous adenocarcinoma of the eyelidOphthalmic Surg 1983 14:935-40. [Google Scholar]
[12]. Ahmad J, Mathes DW, Itani KM, Reconstruction of the eyelids after Mohs surgerySemin Plast Surg 2008 22(4):306-01. [Google Scholar]
[13]. Parodi PC, Faini G, De Biasio F, Rampino Cordaro E, Guarneri GF, Miani F, Full-thickness lower eyelid reconstruction with a conchal chondro-perichondral graft and local coverage with Mio-cutaneous flaps—our divisional experienceJ Oral Maxillofac Surg 2008 66(9):1826-32. [Google Scholar]
[14]. Harvey DT, Taylor RS, Itani KM, Loewinger RJ, Mohs micrographic surgery of the eyelid: an overview of anatomy, pathophysiology, and reconstruction optionsDermatol Surg 2013 39(5):673-97. [Google Scholar]
[15]. Stein JD, Antonyshyn OM, Aesthetic eyelid reconstructionClin Plast Surg 2009 36(3):379-97. [Google Scholar]
[16]. Jewett BS, Shocley WW, Reconstructive options for periocular defectsOtolaryngol Clin North Am 2001 34(3):601-25. [Google Scholar]
[17]. Miyamoto J, Nakajima T, Nagasao T, Konno E, Okabe K, Tanaka T, Fullthickness reconstruction of the eyelid with rotation flap based on orbicularis oculi muscle and palatal mucosal graft: long-term results in 12 casesJ Plast Reconstr Aesthet Surg 2009 62(11):1389-94. [Google Scholar]
[18]. Moesen I, Paridaens D, A technique for the reconstruction of lower eyelid marginal defectsBr J Ophthalmol 2007 91(12):1695-97. [Google Scholar]
[19]. Ducic Y, Burye M, Nasolabial flap reconstruction of oral cavity defects: a case report of 18 casesJ Oral Maxillofac Surg 2000 58:1104-08. [Google Scholar]
[20]. Shields CL, Naseripour M, Shields JA, Eagle RC, Topical mitomycin C for pagetoid invasion of the conjuctiva by eylid sebaceous gland carcinomaOphthalmology 2002 109:2129-33. [Google Scholar]
[21]. Nunery WR, Welsh MG, McCord CD., Jr, Recurrence of Sebaceous carcinoma of the eyelid after radiation therapyAm J Ophthalmol 1983 96:10-15. [Google Scholar]
[22]. Hendley RL, Reiser JC, Cavanagh HD, Primary radiation therapy for meibomian gland carcinomaAm J Ophthalmol 1979 87:206-09. [Google Scholar]