Atypical Response of Gingival Tissue to Extruded Metapex
Puneet Jindal1, Navjot Singh Khurana2, Ruchi Juneja3, Harmesh Sharma4, Varun Kumar5
1 Senior Resident, Department of Conservative Dentistry and Endodontics, Oral Health Sciences Centre, PGIMER, Chandigarh, India.
2 Demonstrator, Department of Conservative Dentistry and Endodontics, Government Dental College, Patiala, Punjab, India.
3 Senior Resident, Department of Conservative Dentistry and Endodontics, Oral Health Sciences Centre, PGIMER, Chandigarh, India.
4 Assistant Professor, Department of Perodontics, Government Dental College, Patiala, Punjab, India.
5 Consultant Endodontist, Faces N Smiles Dental Clinic, Sector-10, Chandigarh, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ruchi Juneja, 3052, Sector 38 D, Chandigarh-160036, India.
E-mail: ruchijuneja1986@gmail.com
Biodentin, Calcified canal, Gingival pouch, Perforation
A 30-year-old female reported with a chief complaint of pain in upper front tooth and an ulcer on gum in the same area. There was a history of multiple dental appointments for root canal treatment of the same tooth and during this course of treatment, an ulcer had developed on the gingiva, which hadn’t healed since last two months. No history of any associated systemic disease was reported.
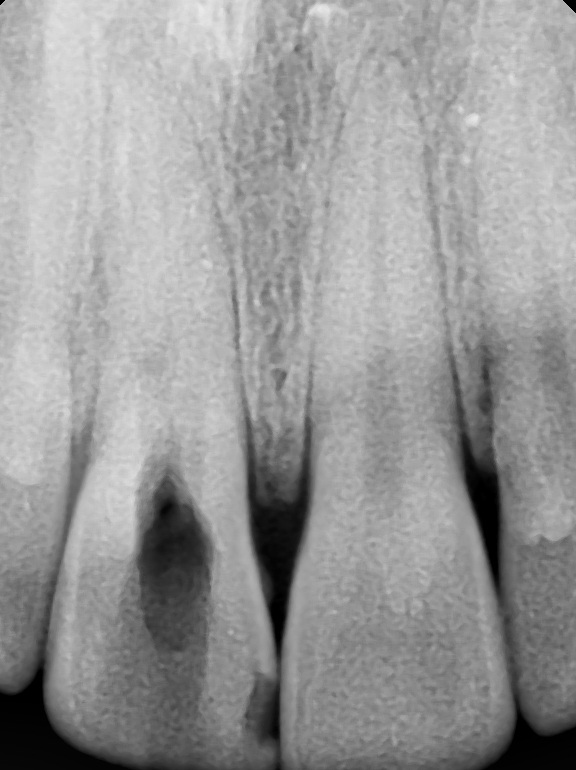
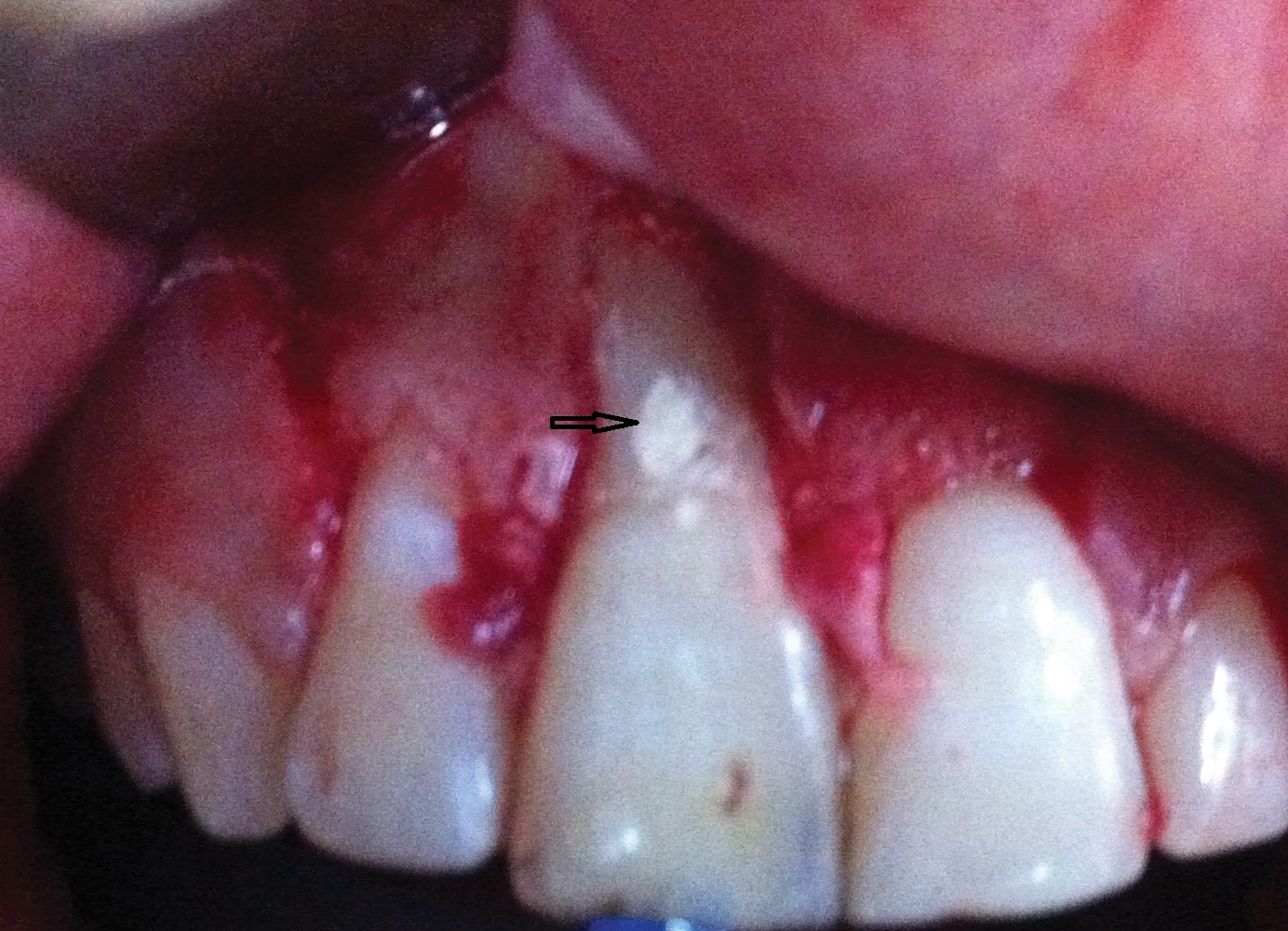
On clinical evaluation, maxillary right central incisor was found to be discoloured and a fenestration defect of size 2X2mm was present in the gingiva through which the root of the tooth was visible [Table/Fig-1]. The area was free of any discharge, with a mild swelling on the attached gingiva, firm on digital palpation. The tooth was slightly tender on percussion. Pulp sensitivity tests produced no response on Tooth #11 and normal response on adjacent teeth.
Pre-operative clinical picture showing fenestration with respect to maxillary right central incisor.

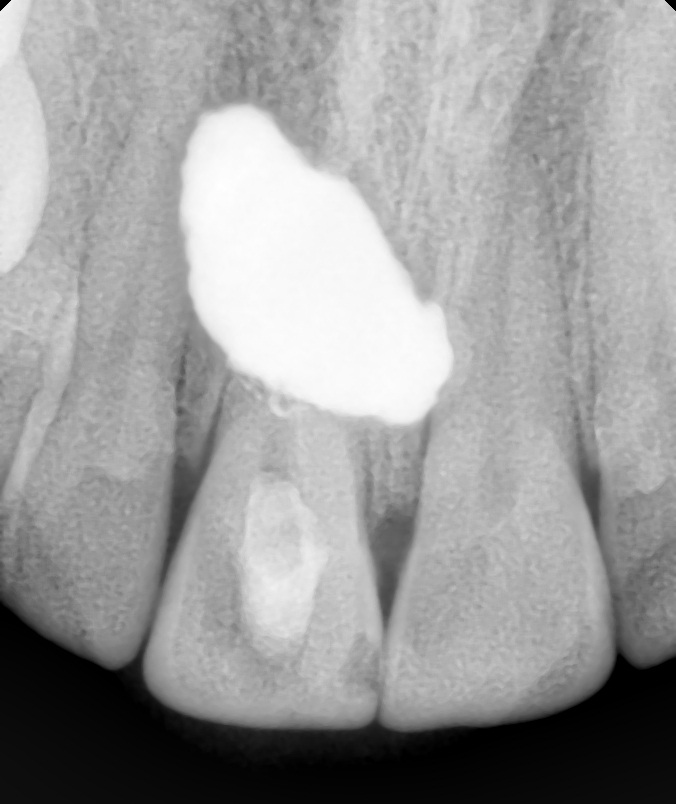
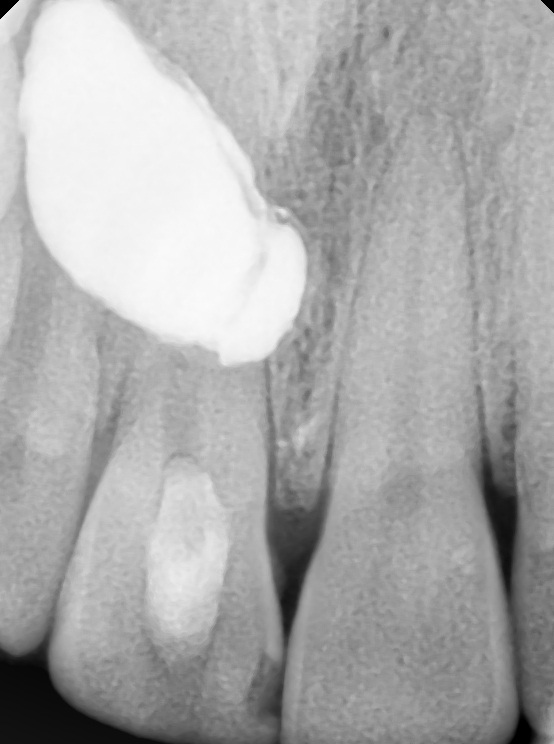
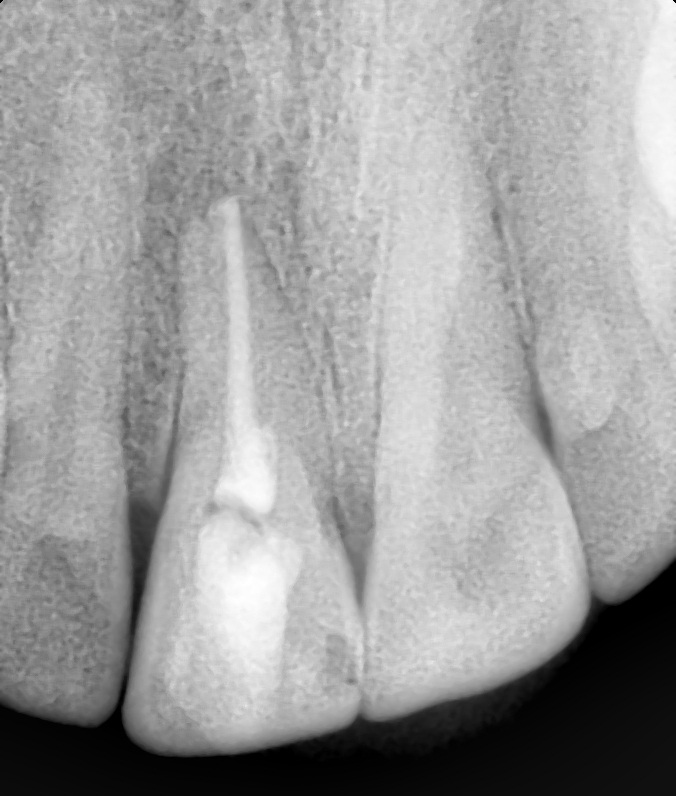
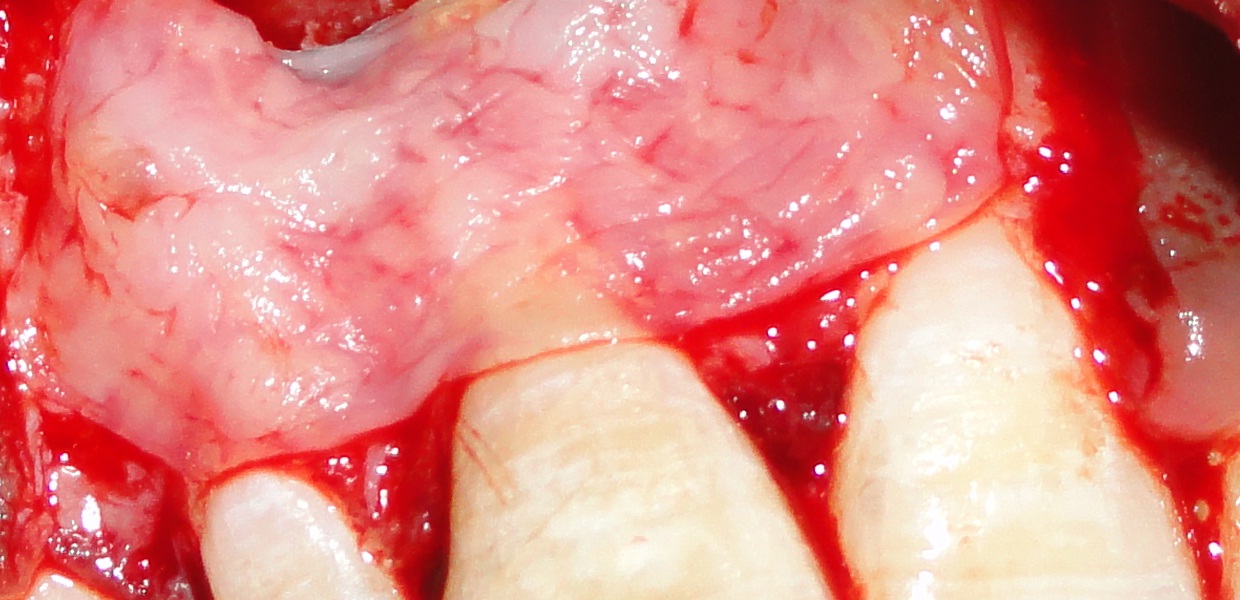
Radiographic evaluation revealed a sealed access, but the root outline was completely obscured by a radiopaque shadow [Table/Fig-2], indicating a possibly extruded root canal filling material. Clinical exploration revealed a buccal perforation. The main canal had not been located and seemed calcified. As it was necessary to check the direction of advancement of file during the search of the calcified canal, surgery was planned to remove the radiopaque material. Surprisingly, no material was found underneath the flap [Table/Fig-3]. An intraoperative radiograph was taken to assess the status, however, the radiopaque shadow was still present, but at slightly different location than the previous radiograph [Table/Fig-4]. This raised the suspicion that the material could be somewhere within the flap. On examination, it was found that the flap in a localized area was thicker and more firm. Hence, a vertical incision was given on the connective tissue side of the flap and a yellow colored material (metapex) was found encapsulated within the connective tissue [Table/Fig-5,6]. Thorough curettage was done and the material was completely removed [Table/Fig-7]. Repeat radiograph revealed a calcified canal [Table/Fig-8], which was then located with an endodontic explorer. Root canal treatment was completed on the same appointment [Table/Fig-9] and perforation was repaired using biodentin [Table/Fig-10]. Before closure, Platelet-Rich Fibrin (PRF) membrane was placed on the root surface of Tooth #11 to cover the apicomarginal bony defect and the flap was sutured back [Table/Fig-11,12].
Pre-operative radiograph with sealed access with respect to tooth #11 and root margins obscured by radiopaque shadow.
Clinical picture after flap reflection didn’t reveal any material beneath the flap.

Intraoperative radiograph revealed that the material was still there, but at slightly different location in comparison to pre-operative radiograph creating a suspicion that material might be present within the flap.
Vertical incision given in the flap to expose the material.
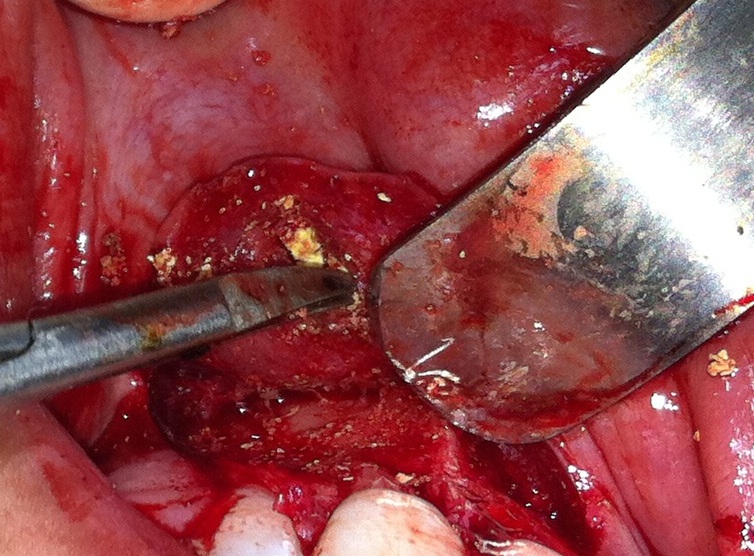
Foreign material completely exposed inside the gingival pouch.
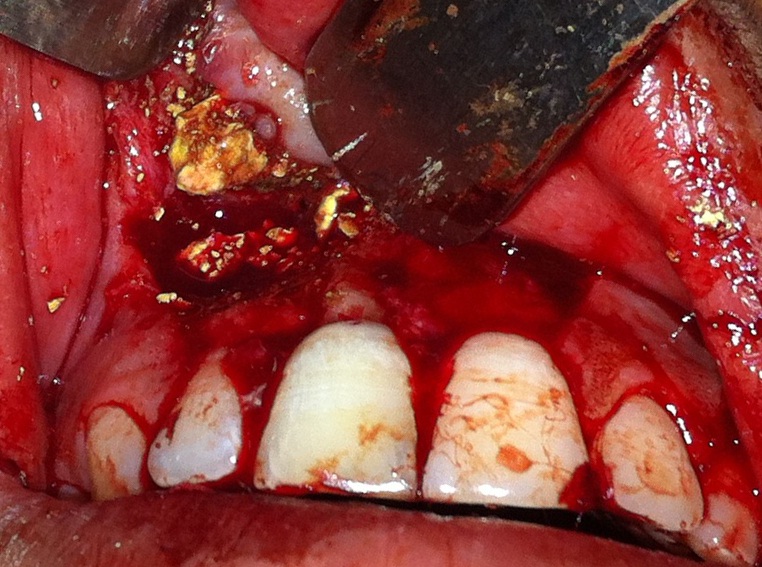
Foreign material curetted out of the gingival pouch.

Radiograph after removal of metapex showing sclerosed canal.
Root canal treatment was completed and canal was obturated using gutta percha points with zinc oxide eugenol sealer.
Perforation on the labial aspect was repaired with bio-dentin after obturation.
PRF was placed to cover the fenestration defect before flap closure.

The follow-up visit after a week revealed uneventful soft tissue healing. Patient was lost to follow up thereafter.
Discussion
Extruded materials have a potential to induce a foreign body reaction, even in the absence of microbial factors. The response of tissues is different depending upon the extent of toxicity of these materials. Calcium hydroxide [Ca(OH)2] is generally considered a well-tolerated endodontic material. But a delay in healing of periapical lesions has been reported by a few researchers in cases of accidental extrusion of Ca(OH)2 [1]. Gingival necrosis, when Ca(OH)2 comes in contact with gingiva, damage to inferior alveolar nerve on neural contact, severe tissue necrosis on inadvertent intra-arterial injection have already been reported in literature [2].
In the present case, it seems probable that it was extruded Ca(OH)2 only, that caused a fenestration defect and the residual amount was completely encapsulated by the granulation tissue within the gingiva. Ca(OH)2 has a high pH and hence, possesses more toxic effect immediately after placement, which decreases over time. The immediate high toxicity was probably sufficient to cause necrosis of overlying bone and gingiva leading to fenestration. As the toxicity decreased over time, the residual amount may have caused the irritational fibroblastic stimulation of gingival connective tissue leading to encapsulation of metapex particles in a pouch like structure. Sahli proposed that the necrotizing ability of calcium hydroxide may destroy any epithelium present thereby allowing a connective tissue invagination [3]. This could be the probable reason for initial penetration into the connective tissue which later got encapsulated due to inflammatory responses.
PRF was used in this case as it acts as a membrane to prevent epithelial migration in addition to acting as a source of many growth factors that play a significant role in healing and repair mechanisms [4].
The widely held view that extruded metapex doesn’t impair tissue healing is not consistent with clinical observations in this case. Every attempt should be made to limit all kinds of endodontic materials within the confines of root canal to achieve a predictable healing outcome. All efforts should be made to prevent extrusion of calcium hydroxide material to avoid any complications and achieve a faster healing.
[1]. Galhotra V, Singla A, Jindal S, Sofat A, Effect of unintentional periapical extrusion of metapex in immature teeth-a case reportJ Clin Diagn Res 2015 9(1):ZD01-02. [Google Scholar]
[2]. Shahravan A, Jalali S, Mozaffari B, Pourdamghan N, Overextension of nonsetting calcium hydroxide in endodontic treatment: literature review and case reportIran Endod J 2012 7:102-08. [Google Scholar]
[3]. Sahli CC, Radiographic and histological study of a case of apexification in a human molarRev Esp Endodoncia 1989 7:101-06. [Google Scholar]
[4]. Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T, Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recessionJ Indian Soc Periodontol 2015 19:66-71. [Google Scholar]