Giant Intramuscular Nodular Fasciitis Masquerading as Soft Tissue Sarcoma with Neural Involvement - A Case Report
Anandhi Amaranathan1, Vishnu Prasad Nelamangala Ramakrishnaiah2, Susan Rajan3, Rajesh Nachiappa Ganesh4
1 Assistant Professor, Department of Surgery, JIPMER, Puducherry, India.
2 Professor, Consultant G I Surgeon, Department of Surgery, JIPMER, Puducherry, India.
3 Junior Resident, Department of Surgery, JIPMER, Puducherry, India.
4 Associate Professor, Department of Pathology, JIPMER, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anandhi Amaranathan, 12, New Street, Shanthi nagar, Lawspet, Pondicherry- 605008, India.
E-mail: anandhiramesh76@yahoo.in
Nodular Fasciitis (NF) is described as a benign reactive proliferation of myofibroblasts that occurs predominantly in the subcutaneous location. Most commonly presents as rapidly growing swelling in the young adults, with usual size of less than 4cm and located commonly in the extremities. We hereby report a case of giant nodular fasciitis of 10cm diameter which presented in an unusual location (gluteal region) and rare plane of origin (intramuscular) with unusual symptom of sciatic nerve involvement. Because of the size, location and neural involvement a clinical diagnosis of soft tissue sarcoma was made. After investigating with trucut biopsy and magnetic resonance imaging, benign nature of the lesion confirmed and treated with complete excision, carefully preserving the sciatic nerve. This case is presented for its rarity in size, location, plane of origin and neural compression. To the best of our knowledge this is the first case of nodular fasciitis of 10cm size and in the gluteal muscles.
Gluteal region, Myofibroblasts, sciatic nerve
Case Report
A 19-year-old male presented with complaints of swelling in the left gluteal region for the past 2 years. It was slowly increasing in size and associated with dull ache. He experienced a shooting type of pain for the past one month. He also complained of weakness in the limb, inability to sit on the floor, to squat and to stand for more than 10 minutes. There was no past history of trauma, fever, irradiation or surgery. On examination, 10X10cm hard mass, non tender with ill-defined borders present in the left gluteal region. Swelling was fixed to the underlying bone. Overlying skin was normal. Obvious muscle wasting was present in the left lower limb and power was decreased (4/5) in all muscle compartments. Patient had difficulty in sitting cross legged and to squat. Flexion and abduction at the hip joint showed restriction. No sensory loss was noted. After clinical examination a provisional diagnosis of soft tissue sarcoma with involvement of sciatic nerve was made. Further investigations like trucut biopsy and Magnetic Resonance Imaging (MRI) were done.
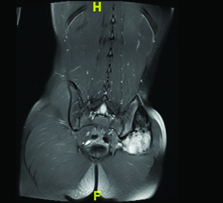
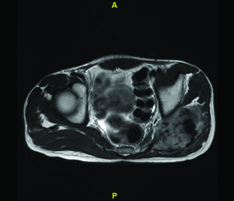
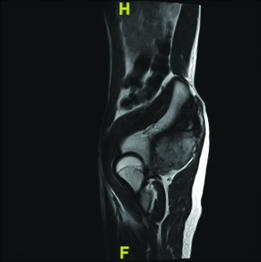
MRI was done in view of the deeper location of the lesion and to confirm our clinical diagnosis. MRI report showed a partly defined heterogeneous solid tumour involving left Gluteus medius and minimus muscles with extension into Gluteus maximus muscle. The lesion was T1 iso, T2 hyper soft tissue component and T1/T2 hypo intense fibrotic component within. On post contrast the soft tissue component showed intense enhancement. Antero medially the lesion was abutting the iliac bone with a small focus of erosion within. Inferiorly it extends till the level of femoral neck region. The muscular branches of the left sciatic nerve appeared to be encased by the tumour while maintained fat plane is noted involving rest of the nerve [Table/Fig-1,2 and 3].
MRI Picture coronal section showing enhancing heterogenous mass in the left gluteal region.
MRI picture of axial plane showing the heterogenous intramuscular mass in the left gluteal region.
MRI picture, sagittal plane, showing the heterogenous mass with well maintained plane with the adjacent bone.
Intraoperatively the mass looked nodular and hard, fixed to the underlying iliac bone, involving the gluteal muscles. It was locally infiltrating the surrounding muscles producing compression on the sciatic nerve. Wide local excision was performed along with the involved gluteal muscles [Table/Fig-4]. Sciatic nerve was identified and preserved.
Well circumscribed, solid, grey white, firm mass on cross section of the specimen.

Trucut biopsy was done which showed spindle cell lesion. No necrosis or pleomorphism. Bland nuclear morphology. Some cells with abundant eosinophilic cytoplasm, suggestive of reactive fibroblastic nodular fasciitis.
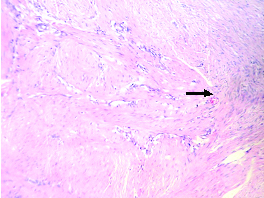
Postoperative biopsy report showed lesion composed of spindle cells with multinodular growth pattern. Focal areas are composed of plump myoid cells with eosinophilic cytoplasm forming short fascicles. Nuclei were elongated, cigar shaped with tapering end. There was no evidence of atypia. There were extensive areas of hyalinization in nodules scattered throughout the lesion [Table/Fig-5,6]. Immunohistochemistry was done which showed Vimentin positive and negative for S100, Desmin and Myoglobin. These features are suggestive of benign proliferative fibroblastic lesion. Possibilities considered are Myofibroma and Nodular fasciitis.
Section show higher magnification of the lesion highlighting plump spindle cells with abundant unifascicular cytoplasmic processes. H & E stain, x 40.
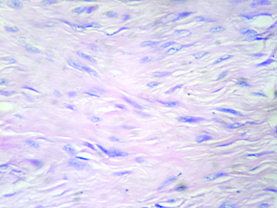
Section show an ill circumbscribed infiltrative lesion comprised of bland appearing spindle shaped cells in sheets and fascicles. H & E stain, x 10.
At follow-up after first, third and sixth month, the muscle power was found to be significantly better than preoperative status. There was no pain but he still has some difficulty in sitting on the floor cross legged and squatting. Also, flexion and abduction at the hip joint showed mild restriction.
Discussion
Nodular fasciitis is a benign myofibroblastic proliferation, which was first reported in 1955 as pseudosarcomatous fibromatosis or fasciitis [1]. The exact aetiology of this proliferative lesion is not known. The triggering factors postulated are local injury or inflammation [2].
More common in young to middle aged adults (20 to 50 years), with a peak incidence in fourth decade [3]. Sex incidence is equal. All reported lesions are usually less than 4cm in diameter. With a few exceptions [3–5] where 8cm, 5cm and 7cm size lesions were reported respectively. To the best of our knowledge our case is the biggest (10X10X5cm) size of nodular fasciitis reported so far. The usual clinical presentation is a rapidly growing swelling with duration of less than a month during consultation. Our patient on the contrary, presented with a swelling of more than one year duration. Only very few cases has been reported with a long duration of symptom like this [6,7].
The upper extremity was the most common location (34%), followed by the head and neck region (24%), trunk (21%), and lower extremity (14%) [3]. Nodular fasciitis in the gluteal region has not been reported so far in the English literature.
Pathologically, nodular fasciitis is an unencapsulated lesion that is typically well demarcated from the surrounding uninvolved tissue but may be focally infiltrative [8] as in our case. There are 3 types of nodular fasciitis according to the anatomical location. They are subcutaneous, fascial (intermuscular) and intramuscular [9]. The subcutaneous form is most common, followed by the fascial form, with the intra-muscular form being the least common [2]. In a retrospective study of 272 cases the subcutaneous form was reported to be 94% and intramuscular form only 5.9% [3]. The intramuscular form can attain a large size as in our case. It is usually considered as soft tissue sarcoma in the clinical scenario due to the deeper location and large size. Other rare forms of nodular fasciitis like intraneural form and intravascular forms are also reported [10–12]. Some rare forms like intra arterial, intraneural and intradermal are also reported.
Fine needle aspiration cytology can be done in the initial evaluation though the diagnosis is quite challenging. The relatively small amount of tissue obtained is often insufficient for a definitive panel of special stains, and thus surgical excision with histological evaluation is recommended. Therefore, caution should be maintained when using FNA to diagnose nodular fasciitis [13].
Imaging with Computer Tomography (CT) or Magnetic Resonance Imaging (MRI) can be used for diagnosis. It is usually fascia based, oval in shape with homogeneous low to isodensity on CT scan. In cases with myxoid change, contrast-enhanced CT scan shows heterogeneous appearance with prominent peripheral nodular or rim-like enhancement. On CT and MR imaging, nodular fasciitis is generally seen as a relatively well-defined, soft-tissue mass of superficial location. Intramuscular forms are mostly deep seated and large and have ill-defined margins [9]. On MRI, the lesion often appears as homogenous T1 signal iso intense to adjacent skeletal muscles and shows heterogeneous intermediate to high signal with different enhancement patterns on T2- or short TI Inversion-Recovery (STIR) weighted sequences attributable to the variable components and cellularity on histology. Some cases may demonstrate distinct and discrete internal and central high T2-weighted signal areas with lower T2- weighted signal intensity peripheral rim, which represents reticulated perilesional soft tissue edema on fluid-sensitive sequences [9].
Microscopically, these lesions are characterized by a cellular spindle cell growth in a loosely textured mucoid matrix with lymphocytic infiltration and extravasations of red blood cells. An important diagnostic finding is the presence of undulating wide bands of collagen lined on the side of spindle cells. The high cellularity of the lesion and the presence of mitotic figures are responsible for the frequent confusion of this lesion with sarcoma [14]. Immunohistochemistry is very useful in confirming the diagnosis. The spindle cells showed diffuse expression of smooth muscle actin. They were also positive for calponin, muscle specific actin, and CD10. Intralesional histiocytes and small multinucleated giant cells were positive for CD68 [3].
Treatment options include observation, as spontaneous regression has been reported [15], intralesional steroid or marginal excision. Local excision is by far the most commonly opted treatment. Recurrence after excision is very rare.
Conclusion
Diagnosis of nodular fasciitis is very challenging and it is often mistaken for a sarcoma because of its rapid growth, rich cellularity, and high mitotic activity, poorly circumscribed nature, which may result in it being easily misdiagnosed as a sarcomatous lesion like malignant fibrous histiocytoma or fibro sarcoma.
The diagnosis of nodular fasciitis can be very challenging clinically, especially large intramuscular forms as in our case. FNAC can be easily deceiving as mentioned previously. Further imaging like USG, CT or MRI can help in coming to a conclusion about the benign nature of the lesion. So considering this entity in our differential diagnosis is more important for planning the management
[1]. Konwaler BE, Keasbey L, Kaplan L, Subcutaneous pseudosarcomatous fibromatosis (fasciitis)Am J Clin Pathol 1955 25(3):241-52. [Google Scholar]
[2]. Sinhasan SP, KVB Bhat RV, Hartimath BC, Intra-muscular nodular fasciitis presenting as swelling in neck: challenging entity for diagnosisJ Clin Diagn Res JCDR 2014 8(1):155-57. [Google Scholar]
[3]. Lu L, Lao IW, Liu X, Yu L, Wang J, Nodular fasciitis: a retrospective study of 272 cases from China with clinicopathologic and radiologic correlationAnn Diagn Pathol 2015 19(3):180-85. [Google Scholar]
[4]. Nakagawa T, Sugimoto T, Komiyama S, Yamamoto T, Uemura T, Giant tumour formed by nodular fasciitis of the pharynx: a case reportAuris Nasus Larynx 1994 21(3):196-99. [Google Scholar]
[5]. Xie S, Liu W, Xiang Y, Dai Y, Ren J, A huge nodular fasciitis in parapharygneal space in a 7-year-old girl: a case report and review of literatureInt J Clin Exp Pathol 2014 7(12):9023-27. [Google Scholar]
[6]. Cyriac MJ, Celine MI, Kurien G, Puthiode U, Nodular fasciitisIndian J Dermatol Venereol Leprol 2004 70(4):239-41. [Google Scholar]
[7]. Weinreb I, Shaw AJ, Perez-Ordoñez B, Goldblum JR, Rubin BP, Nodular fasciitis of the head and neck region: a clinicopathologic description in a series of 30 casesJ Cutan Pathol 2009 36(11):1168-73. [Google Scholar]
[8]. Tomita S, Thompson K, Carver T, Vazquez WD, Nodular fasciitis: a sarcomatous impersonatorJ Pediatr Surg 2009 44(5):e17-19. [Google Scholar]
[9]. Kim ST, Kim H-J, Park S-W, Baek CH, Baek JH, Byun HS, Nodular fasciitis in the head and neck: CT and MR imaging findingsAJNR Am J Neuroradiol 2005 26(10):2617-23. [Google Scholar]
[10]. Parrett BM, Orgill DP, Marsee DK, Freedman AS, Raut CP, Novel presentation of intraneural nodular fasciitis of the sciatic nerveJ Peripher Nerv Syst JPNS 2007 12(1):61-63. [Google Scholar]
[11]. Kakutani K, Doita M, Nishida K, Akisue T, Maeno K, Zhang Z, Intractable sciatica due to intraneural nodular fasciitis detected by positron emission tomographySpine 2010 35(21):E1137-40. [Google Scholar]
[12]. Gwan-Nulla DN, Davidson WR, Grenko RT, Damiano RJ, Aortic dissection in a weight lifter with nodular fasciitis of the aortaAnn Thorac Surg 2000 69(6):1931-32. [Google Scholar]
[13]. Mallina S, Rosalind S, Philip R, Harvinder S, Gurdeep S, Sabaria MN, Nodular fasciitis: a diagnostic dilemmaMed J Malaysia 2007 62(5):420-21. [Google Scholar]
[14]. Kotha GK, Bj V, Maryada VR, Jawalkar H, Multifocal nodular fasciitis of the hand and shoulder: case reportJ Hand Surg 2014 39(12):2468-71. [Google Scholar]
[15]. Mardi K, Sharma J, Kaur H, Nodular fasciitis of the hand - a potential diagnostic pitfall in fine needle aspiration cytologyJ Cytol 2007 24(4):197 [Google Scholar]