Diagnostic Dilemma in a Thyroid Incidentaloma: Second Primary versus Metastatic Nodule?
Abid Ali Mirza1, Esha Pai2, Kodaganur Gopinath Srinivas3, Shankarappa Amarendra4, K.S Gopinath5
1 Senior Resident, Department of Surgical Oncology, HCG- Bangalore Institute of Oncology, Bangalore, India.
2 Senior Resident, Department of Surgical Oncology, HCG- Bangalore Institute of Oncology, Bangalore, India.
3 Junior Resident, Department of Surgical Oncology, HCG- Bangalore Institute of Oncology, Bangalore, India.
4 Consultant Surgical Oncologist, Department of Surgical Oncology, HCG- Bangalore Institute of Oncology, Bangalore, India.
5 Consultant Surgical Oncologist, Department of Surgical Oncology, HCG- Bangalore Institute of Oncology, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Esha Pai, 802, Olive 1, Prestige St. Johns Woods, 80 St. Johns Cross Road, Koramangala, Bangalore -560029, India.
E-mail: dr.eshapai@gmail.com
With the increasing use of 18F-Fluro-Deoxyglucose (FDG) Positron Emission Tomography (PET) the number of thyroid incidentalomas is on the rise. Focal thyroid incidentalomas identified by FDG-PET have been reported to have a high incidence of malignancy. Neuroendocrine tumours of the thyroid are rare entities. The most common neuroendocrine tumour of the thyroid is medullary carcinoma. A thyroid nodule in a patient with a known neuroendocrine tumour must be differentiated from a primary medullary carcinoma which can present as a diagnostic challenge to the clinician.
A 65-year-old female patient was referred for thyroidectomy for a FNAC diagnosed follicular neoplasm of the left lobe of the thyroid, detected on FDG PET follow up. She was a known case of neuroendocrine tumour of the pancreas with no features suggestive of familial Multiple Endocrine Neoplasia (MEN) syndrome. The patient had undergone Whipple’s procedure elsewhere, 5 years back. Following total thyroidectomy, the final histopathology report was suggestive of a primary neuroendocrine tumour.
We present this case to highlight the clinical dilemma in diagnosing a thyroid incidentaloma as a second primary neuroendocrine tumour versus a solitary metastatic nodule in the background of metastatic gastroentero pancreatic neuroendocrine tumour. Although clinically, a metastatic nodule should have been the obvious diagnosis, the histopathological and immunohistochemical features were in favour of a primary non-medullary Neuroendocrine Tumor (NET) of the thyroid.
Multiple Endocrine Neoplasia syndrome, Neuroendocrine tumours, Whipple’s procedure
Case Report
A 65-year-old asymptomatic female patient was referred to the Department of Surgical Oncology; Bangalore Institute of Oncology, for thyroidectomy for a FNAC diagnosed follicular neoplasm of the left lobe of the thyroid. She was a known case of neuroendocrine tumour of the pancreas, having undergone a Whipple’s procedure, elsewhere 5 years back. She had no co-morbidities and family history was negative. The histopathology of the Whipple’s procedure was reported as well differentiated endocrine carcinoma, with negative circumferential margins (R0). The tumour was Neuron Specific Enolase (NSE), synaptophysin and chromogranin A positive on immunohistochemical studies.
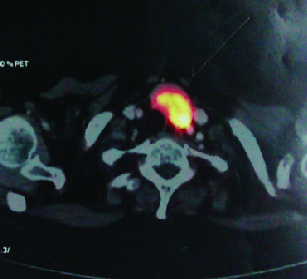
On the sixth month of follow-up her chromogranin A levels were elevated (825ng/ml, Normal <100 ng/ml), but subsequent endoscopic USG did not show any recurrence. The patient was followed up with annual abdominal CT. On the fifth year, follow-up CT showed nodular lesions in segment 4b, 7 and 8. Subsequent PET CT showed increased tracer uptake in heterogeneously enhancing lesion measuring 2.8x3.9x3.3cm in the region of inferior left lobe of thyroid [Table/Fig-1]. USG guided FNAC was reported as follicular neoplasm. Preoperative calcitonin was 25.4 (Normal upto 18.2).
PET CT showing increased tracer uptake in heterogeneously enhancing lesion measuring 2.8x3.9x3.3 cm in the region of inferior left lobe of thyroid.
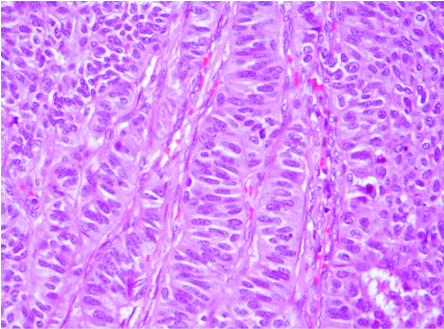
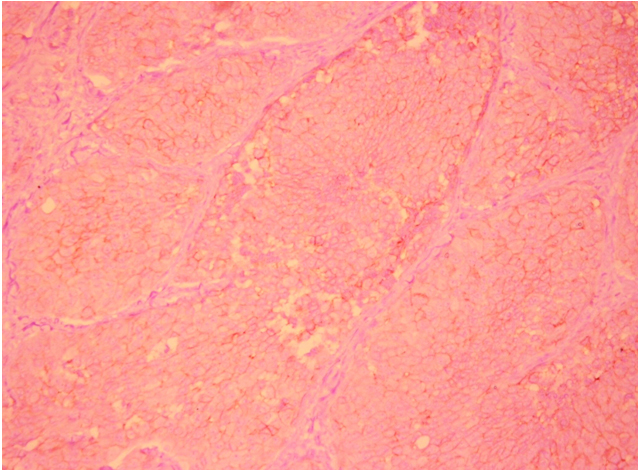
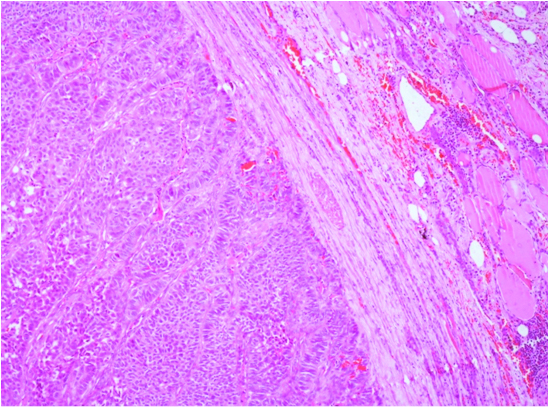
Patient underwent a left hemi thyroidectomy with frozen section followed by total thyroidectomy in the same sitting. The final histopathology, to our surprise, was reported as a single, well encapsulated, nodule measuring 3.5x3x2cm with neuro-endocrine differentiation. The macroscopically tan nodule displayed a trabecular pattern reminiscent of neuro-endocrine differentiation with invasion of vascular spaces [Table/Fig-2]. The immunohistochemistry profile revealed the tumour positive for CD56, synaptophysin, chromogranin and S-100 and negative for TTF-1, calcitonin and thyroglobulin [Table/Fig-3]. The Ki-67 proliferative index was >20% and with vascular invasion present making it grade 3. While the absence of both TTF-1 and thyroglobulin favored a non-thyroid origin, an interstitial pattern of infiltration with multiple nodules characteristic of thyroid metastases was conspicuously absent. The solitary nodule with a well delineated capsule favoured a primary thyroid tumour [Table/Fig-4]. The postoperative course was uneventful. The patient was referred back to the oncology department for chemotherapy.
Trabacular pattern in circumscribed nodule reminiscent of neuro-endocrine differentation with invasion of vascular spaces.
Immunohistochemistry showed CD 56 neuroendocrine marker membraneous staining in the thyroid nodule.
Circumscribed solitary nodule invested by well delineated fibrous capsule separating normal back ground thyroid tissue in the periphery.
Discussion
Thyroid incidentaloma is defined as a thyroid nodule that is incidentally detected by imaging techniques performed for an unrelated purpose. With the increasing use of 18F-Fluro-Deoxyglucose (FDG) Positron Emission Tomography (PET) the number of thyroid incidentalomas is on the rise. PET detected thyroid incidentalomas are classified as diffuse and focal. Most diffuse patterns are considered benign since autoimmune thyroiditis is commonly found [1]. Focal Thyroid incidentalomas with high SUV max in euthyroid patients have a greater risk of harboring a malignancy as demonstrated by Pagano L et al., [2]. Hence, a complete work up including a neck ultrasound and FNAC is mandatory to characterize the nodule. Systematic reviews analyzing focal FDG-PET avid thyroid lesions detected malignancies in 33%-34.8% of subjects, the overwhelming majority (81.3-83%) of which were papillary carcinoma [3,4]. Although the need for intervention in all cases of papillary carcinoma is controversial, given the indolent nature of the disease, other histology’s such as follicular, medullary, anaplastic carcinoma and metastases require intervention unless the patient has a very poor performance status.
Management of thyroid incidentalomas involves careful consideration as to when intervention is required. Appropriate investigation and management depend on the disease stage, patient’s performance status, prognosis and treatment plan for the known nonthyroid cancer and whether or not the thyroid abnormality is symptomatic. In our patient, since the liver metastases were amenable to liver directed therapy, it was decided to tackle the thyroid malignancy initially.
Neuroendocrine tumours of the thyroid are rare entities. Most are derived from C cells, ranging from carcinoid to the more ominous small cell carcinoma. Metastasis to the thyroid from these tumours can mimic primary neuroendocrine tumours of the thyroid, especially medullary carcinoma. While most neuroendocrine and medullary tumours of the thyroid are sporadic, up to 20% are familial and inherited in an autosomal dominant manner with high degree of penetrance. C cell lesions are readily diagnosed using immuno staining with calcitonin, which is a secretory product of C cells [5]. Other intra thyroidal lesions which include hyalinizing trabecular neoplasms, true paraganglioma, insular carcinoma, parathyroid lesions, show neuroendocrine differentiation. C cell lesions derived from the neural crest, migrate to the thyroid parenchyma via the ultimobranchial body; hence are found predominantly in the upper halves of the thyroid lobes. They are readily diagnosed in histological sections using Grimelius stain and neuroendocrine markers such as chromogranin A, synaptophysin and neuron-specific enolase. Immunostaining using calcitonin, calcitonin-gene–related peptide, somatostatin, gastrin-releasing peptide and serotonin are more specific in identifying these lesions [5].
In an autopsy series the incidence of thyroid metastases in patients with known malignancy was 1.9-24%, the majority having lung, breast and melanoma as primary [6]. Metastatic tumours to the thyroid usually manifest as multiple tumour nodules infiltrating and undermining the thyroid parenchyma with multiple foci of vascular and lymphatic invasion [7]. In this case a circumscribed nodule invested by fibrous capsule was seen on H & E staining [Table/Fig-4], which was in favour of a primary and not metastases. On reviewing the literature, a second primary neuroendocrine tumour in a patient with a known primary, has not been described to the best of our knowledge. This highlights the dilemma we faced in diagnosing the patient since the clinical and histopathological findings did not correlate. Immunohistochemical studies are usually helpful in distinguishing metastatic disease from medullary carcinoma. Secondary neuroendocrine tumours of the thyroid usually are negative for calcitonin and Carcinoembryonic Antigen (CEA). However, calcitonin can be positive in cells of small cell carcinoma of the lung, but CEA is usually negative. The importance of history and physical examination in this setting is crucial as isolated metastasis to the thyroid is rare and patients usually have manifestations of metastasis to other organs. Besides, symptamology characteristic of neuroendocrine tumour such as diarrhea, flushing, weight loss may be elicited [8].
Conclusion
Focal thyroid incidentalomas identified by FDG-PET have a high incidence of malignancy and should be investigated thoroughly. A thyroid nodule in a patient with a known neuroendocrine tumour must be differentiated from a rare possibility of a primary medullary carcinoma. Differentiating a metastatic thyroid nodule from the second primary may present a diagnostic challenge, especially when the clinical and histopathology findings do not correlate.
[1]. Ohba K, Nishizawa S, Matsushita A, High incidence of thyroid cancer in focal thyroid incidentaloma detected by 18F-fluorodexyglucose positron emission tomography in relatively young healthy subjects: results of 3-year follow-upEndocrine Journal 2010 57(5):395-401. [Google Scholar]
[2]. Pagano L, Samà MT, Morani F, Thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography with CT (FDG-PET/CT): clinical and pathological relevanceClin Endocrinol (Oxf) 2011 75(4):528-34. [Google Scholar]
[3]. Shie P, Cardarelli R, Sprawls K, Fulda KG, Taur A, Systematic review: prevalence of malignant incidental thyroid nodules identified on fluorine-18 fluorodeoxyglucose positron emission tomographyNucl Med Commun 2009 30(9):742-48. [Google Scholar]
[4]. Soelberg KK, Bonnema SJ, Brix TH, Hegedus L, Risk of malignancy in thyroid incidentalomas detected by 18F-fluorodeoxyglucose positron emission tomography: a systematic reviewThyroid 2012 22(9):918-25. [Google Scholar]
[5]. Biddinger PW, Ray M, Distribution of C-cells in the normal and diseased thyroid glandPathol Annu 1993 28(Pt 1):205-29. [Google Scholar]
[6]. Mirallie E, Rigaud J, Mathonnet M, Gibelin H, Regenet N, Hamy A, Management and prognosis of metastases to the thyroid glandJ Am Coll Surg 2005 200(2):203-07. [Google Scholar]
[7]. Baloch ZW, Cibas ES, Clark DP, Layfield LJ, Ljung BM, Pitman MB, The National Cancer Institute Thyroid fine needle aspiration state of the science conference: a summationCyto Journal 2008 5:6 [Google Scholar]
[8]. Sivrikoz E, Ozbey NC, Kaya B, Erbil Y, Kaya S, Yilmazbayhan D, Neuroendocrine tumours presenting with thyroid gland metastasis: a case seriesJournal of Medical Case Reports 2012 6:73 [Google Scholar]