Dilatation of the Proximal Cystic Duct: Is It a Variant to “Type VI” Choledochal Cyst?
Christos Kaselas1, Dimitrios Patoulias2, Ioannis Patoulias3, Ioannis Spyridakis4
1 Pediatric Surgeon, 1st Department of Pediatric Surgery, “G. Gennimatas” University Hospital, “Aristotle” University of Thessaloniki, Thessaloniki, Greece.
2 Medical Student, 1st Department of Pediatric Surgery, “G. Gennimatas” University Hospital, “Aristotle” University of Thessaloniki, Thessaloniki, Greece.
3 Consultant Pediatric Surgeon, 1st Department of Pediatric Surgery, “G. Gennimatas” University Hospital, “Aristotle” University of Thessaloniki, Thessaloniki, Greece.
4 Consultant Pediatric Surgeon, 1st Department of Pediatric Surgery, “G. Gennimatas” University Hospital, “Aristotle” University of Thessaloniki, Thessaloniki, Greece.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Christos Kaselas, Pediatric Surgeon, 1st Department of Pediatric Surgery, “G. Gennimatas” University Hospital, “Aristotle” University of Thessaloniki, Ethnikis Amynis 41, 54635, Thessaloniki, Greece.
E-mail: xkaselas@otenet.gr
Choledochal cysts are rare congenital malformations, comprising of dilatation of the biliary tree of different localization. Classically, classification of choledochal cysts describes five variants of the disease. Type VI choledochal cyst is considered by many authors as the sixth variant of this classification and is described either as a dilatation of the cystic duct or as a cystic duct cyst. We present a rare case of cystic duct dilatation that presented with acute cholangiopancreatitis and a clinical picture consistent of a choledochal cyst in a 10-year-old female patient. Cholecystectomy with excision of the cystic duct was performed. Histopathologic examination did not reveal any findings consistent with choledochal cyst. Based on these findings we speculate that in our case the dilatation of the cystic duct is a variant to type VI choledochal cyst, based on the fact that no cystic-like malformation has been identified in histology. We provide details of the pre-operative work-up and compare them with intraoperative findings in order to increase awareness of the condition.
Biliary duct disease, Biliary tract surgical procedures, Cholangitis, Extrahepatic biliary tract
Case Report
A 10-year-old girl with insignificant previous medical history was referred to the Department of Paediatrics of our hospital due to acute epigastric pain that radiated to the back and fever up to 39oC. On clinical examination, there was diffuse mild abdominal sensitivity and tenderness which was more intense at the right upper abdominal quadrant. No palpable mass was identified. During her hospitalization, her clinical condition deteriorated with biliary vomiting and mild jaundice. Initial abdominal ultrasound investigation revealed a focal enlargement of the head of the pancreas and cholelithiasis without choledocholithiasis. The diagnosis of acute cholangiopancreatitis was confirmed at that point and a joint treatment between the medical and surgical team was decided. The patient was kept null by mouth for 4 days, a Nasogastric Tube (NGT) was inserted and a 5-days antibiotic course was initiated. On removal of the NGT, she started receiving and tolerating fat-free oral diet and was discharged from hospital on day 7 of treatment after full recovery.
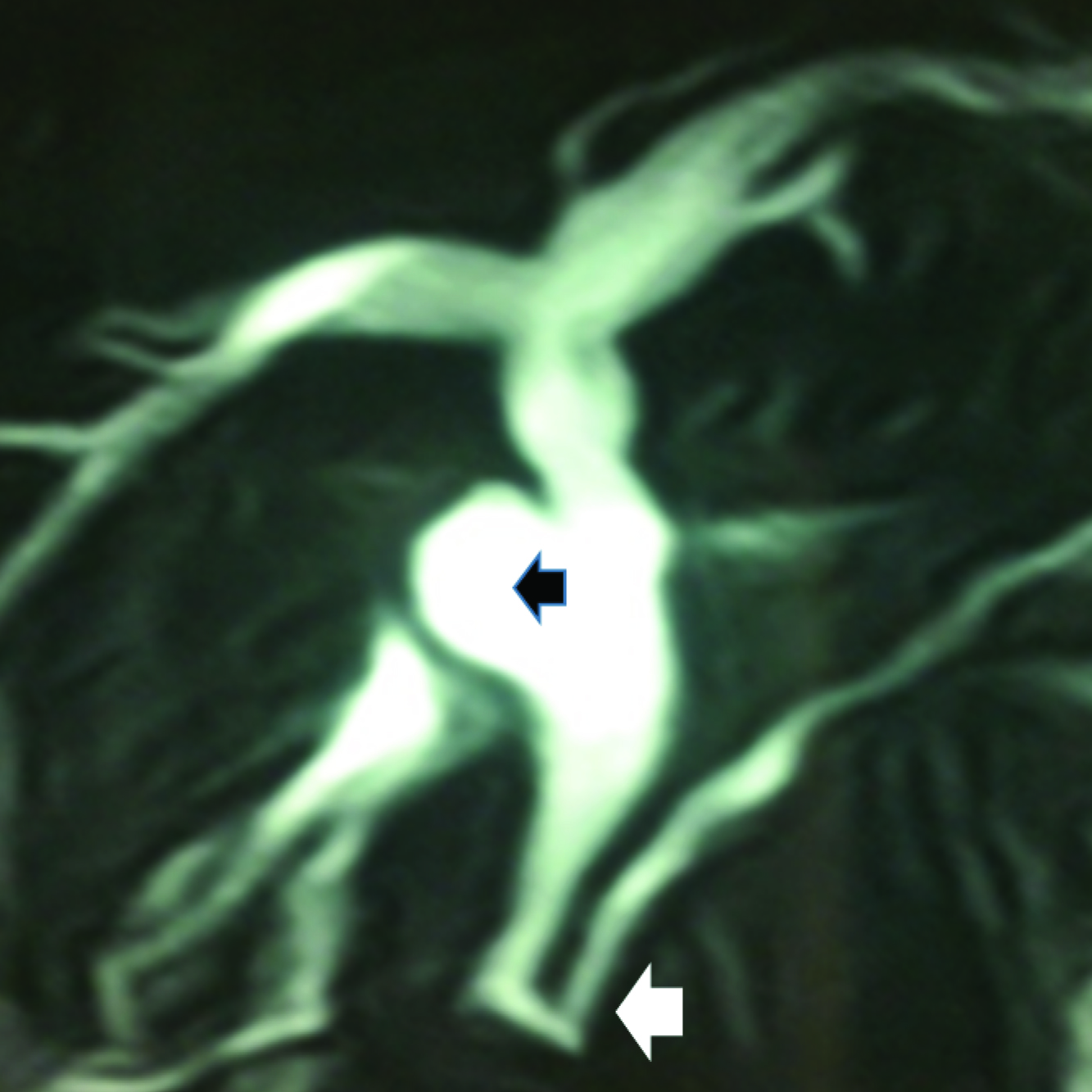
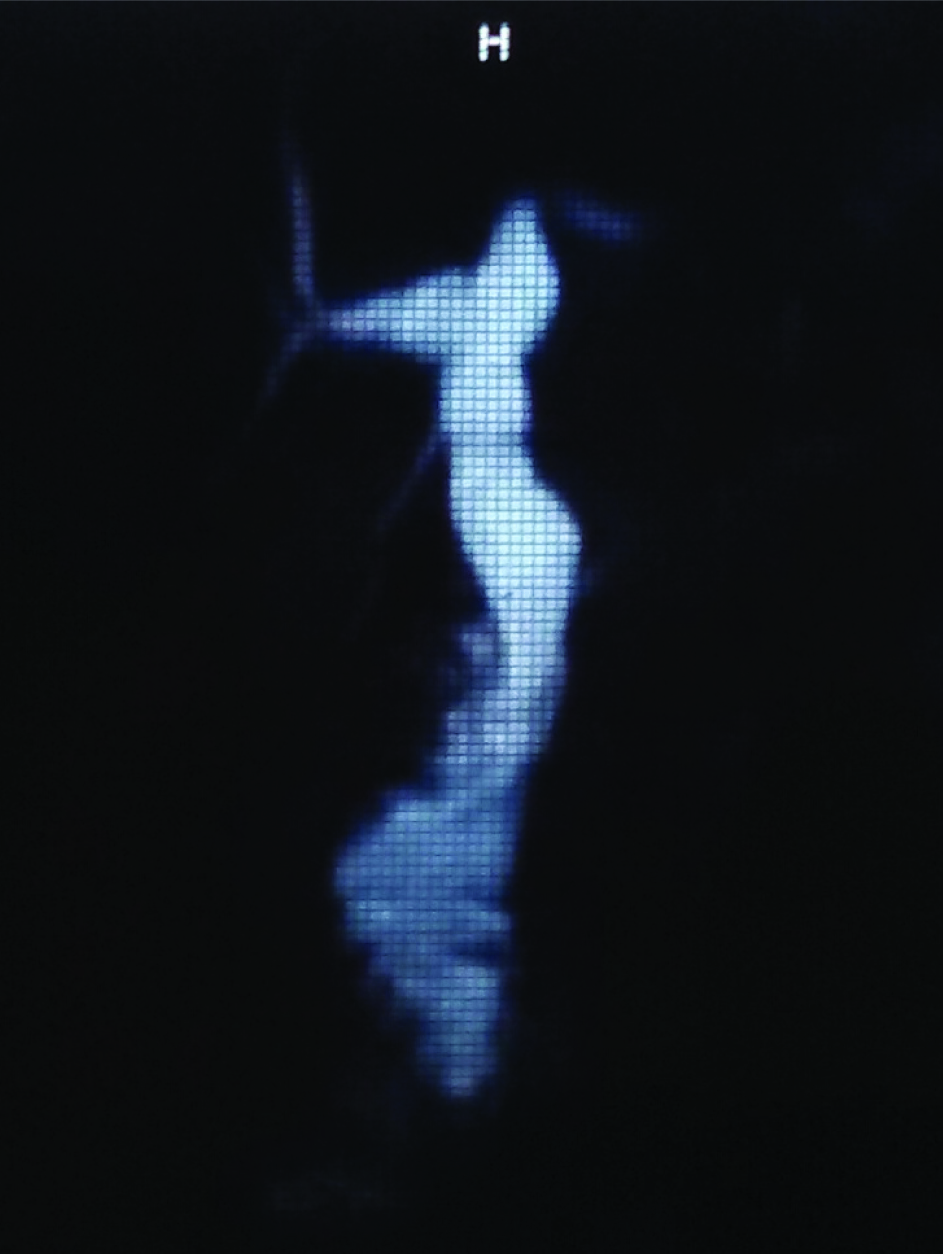
Follow-up ultrasound investigation that was performed after three months, which revealed a saccular lesion adjacent to the distal 1/3 of the bile duct measuring approximately 18mm in diameter and bile sludge that was detected along the common bile duct [Table/Fig-1]. Intra and extra hepatic bile ducts were measured within the upper limits of normal diameter. Subsequent Magnetic Resonance Cholangiopancreatography (MRCP), revealed a cystic lesion of (or adjacent to) the bile duct without identification of a foolproof Abnormal Pancreatic Biliary Duct Junction (APBDJ). Other MRCP findings included mild dilatation of the common hepatic duct and the left and right hepatic ducts without any stones or sludge. Interestingly, gall-bladder and cystic duct were not depicted [Table/Fig-2].
Ultrasonography revealing a saccular lesion adjacent to the distal 1/3 of the bile duct (arrow).

MRCP image revealing a cystic lesion of (or adjacent to) the bile duct (black arrowhead) without identification of a foolproof abnormal pancreatic biliary duct junction (white arrowhead).
With the indication of type I choledochal cyst, the patient was operated. After exposure of the porta hepatis, the gallbladder and cystic duct were recognized. Careful dissection revealed a dilatation of the cystic duct proximal to its junction with the common hepatic duct. The junction itself had a wide opening which excluded the possibility of a cystic duct cyst. Careful inspection and palpation did not indicate any dilatation of the extrahepatic bile tree or presence of gallstones. Typical cholecystectomy with excision of the cystic duct at its junction with the common hepatic duct was performed. Intraoperative cholangiography was performed that demonstrated a picture of possible APBDJ with simultaneous free flow of the contrast to the duodenum [Table/Fig-3]. A mild dilation of the common hepatic and right and left hepatic ducts without any stone identification was also depicted.
Intraoperative cholangiography demonstrating a picture of possible APBDJ (arrowhead) with simultaneous free flow of the contrast to the duodenum.

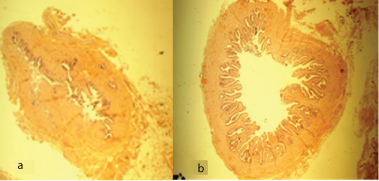
Intraoperative frozen section biopsy did not indicate abnormalities consistent with choledochal cyst. At that point completion of the operation was decided. The postoperative period was uneventful. Routine histopathological examination of the specimen verified that the previous report did not reveal any findings consistent with choledochal cyst but only a dilated cystic duct with normal epithelium [Table/Fig-4a,b]. Two years after the operation, the patient remained free of any complications during regular follow-ups. Postoperative MRI did not reveal any new abnormalities and findings were consistent with the postoperative course [Table/Fig-5].
Histopathological examination of the specimen showing the normal-diameter (a) and the dilated part of the cystic duct (b). (Hematoxylin and eosin stain (H&E), 40x magnification).
Routine Postoperative MRI one year after the operation.
Discussion
This is the first report of a cystic duct dilatation that does not have histopathologic findings consistent with a choledochal cyst and that induces obstructive-like radiographic appearance of bile duct system.
Choledochal cysts are rare cystic malformations of the biliary tree, concerning the extrahepatic and/or the intrahepatic bile ducts. Their incidence is considered to be 1 in every 100.000-150.000 live births. Noteworthy is the fact that the incidence in Asian populations is 10-fold higher than in western populations [1,2].
The most widely used classification of choledochal cysts is the one proposed by Todani et al., which is an extension of the first proposed classification of Alonso Lej et al., [3,4]. According to Todani’s classification, there are 5 types of choledochal cysts. Briefly, type I is the most common type constituting 80%-90% of choledochal cysts and consists of a fusiform or saccular dilatation of the bile duct. Type II cysts are considered as a diverticulum of the bile duct while type III cysts, also called choledochoceles consist of dilatation of duodenal part of the common bile duct. Type IV cysts are described as multiple cysts of the biliary tree and type V cysts, also called Caroli’s disease consist of multiple intrahepatic cysts [4–6].
Although not included in the above classification, there are an important number of publications referring to cystic duct cysts or cystic duct dilatations. Due to their similar clinical presentation and pre-operative findings, but also their consistent histopathological findings to choledochal cysts, many authors proposed that they should be considered as “Type VI” choledochal cysts [1,7–9].
Aetiology of type VI choledochal cyst is rather unclear. Just like choledochal cysts, the most potential theory is associated with an APBDJ and the vicious cycle of pancreatic juice refluxing and mixing with bile, resulting in ductal ectasia [2,10]. As to the localization of the cystic duct-common hepatic duct junction, there is considerable consideration that diminished vascularity of that site, constitutes the junction a weak part where initial dilatation may turn up and evolve [7].
Surgical excision of the cyst is the treatment of choice. This is based not only on the need to relieve the symptoms but also to avoid any future malignant alterations [9–14]. Excision of the cyst can be performed either by open surgery or laparoscopic approach [11]. Although most of the times cholecystectomy and excision of the cystic duct cyst can be achieved, more complicated cases may necessitate additional excision of part of the common bile duct and a Roux-en-Y hepatico-jejunostomy [12].
In our case, clinical presentation of mild cholangiopancreatitis in conjuction with pre- and intraoperative radiographic findings could justify the final diagnosis of a “Type VI” choledochal cyst. However, the double-checked histopathological report of a dilated cystic duct with normal epithelium and without any findings relevant to a choledochal cyst, is inconsistent with such a diagnosis. We speculate that in our case the dilatation of the cystic duct is a variant to type VI choledochal cyst, based on the fact that no cystic-like malformation has been identified in histology.
Although most reports describe a dilatation of the cystic duct, there have been reports describing simultaneous dilatation of both the cystic and common bile duct or a diverticulum of the cystic duct [13,14]. Even more, it has proposed that “Type VI” choledochal cysts should be sub-classified as VIA and VIB depending on the presence of simultaneous common bile dilatation [13].
In our case, cystic duct dilatation should be considered as a variant to Type VI choledochal cyst and treated appropriately. In cases where definite diagnosis is not reached not even during operation, intraoperative frozen section biopsy can be a reliable alternative. If none pathological histological findings are encountered, then cholecystectomy with excision of the cystic duct along with its dilatation should be enough, with close long term follow up being unconditioned. On the other hand, if histological findings consistent of a choledochal cyst are met, then cyst removal with concominant hepatico-jejunostomy is the treatment of choice.
Conclusion
Reports of Type VI choledochal cysts are increasing, necessitating their inclusion in the accepted choledochal cyst classification. However, as these kind of cysts include many variants both on anatomical and histopathological grounds, a separate classification focusing only on cystic duct dilatation features might prove to be more appropriate.
[1]. Yoon JH, Magnetic resonance cholangiopancreatography diagnosis of choledochal cyst involving the cystic duct: report of three casesBr J Radiol 2011 84:18-22. [Google Scholar]
[2]. Singham J, Yoshida EM, Scudamore CH, Choledochal cysts. Part 1 of 3: classification and pathogenesisJ Can Chir 2009 52:434-40. [Google Scholar]
[3]. Alonso-Lej F, Rever WB, Pessango DJ, Congenital choledochal cyst, with a report of 2 and analysis of 94 casesInt Abstr Surg 1959 108:1-30. [Google Scholar]
[4]. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K, Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cystAm J Surg 1977 134:263-69. [Google Scholar]
[5]. Todani T, Watanabe Y, Toki A, Ogura K, Wang ZQ, Co-existing biliary anomalies and anatomical variants in choledochal cystBritish J Surg 1998 85:760-63. [Google Scholar]
[6]. Todani T, Watanabe Y, Toki A, Morotomi Y, Classification of congenital biliary cystic disease: special reference to type IC and IVA cysts with primary ductal strictureJ Hepatobiliary Pancreat Surg 2003 10:340-44. [Google Scholar]
[7]. De U, Das S, Sarkar S, Type VI choledochal cyst revisitedSingapore Med J 2011 52:91-93. [Google Scholar]
[8]. Maheshwari P, Cystic malformation of cystic duct: 10 cases and review of literatureWorld J Radiol 2012 4:413-17. [Google Scholar]
[9]. Goya C, Arslan MS, Yavuz A, Hamidi C, Kuday S, Okur MH, A Rare Anomaly of Biliary System: MRCP Evidence of a Cystic Duct CystCase Rep Radiol 2014 2014:291071doi: 10.1155/2014/291071 [Google Scholar]
[10]. Tadokoro H, Takase M, Recent advances in choledochal cystsOpen J Gastroenterol 2012 2:145-54. [Google Scholar]
[11]. Chan ES, Auyang ED, Hungness ES, Laparoscopic management of a cystic duct cystJSLS 2009 13:436-40. [Google Scholar]
[12]. Shah OJ, Shera A, Shah P, Robbani I, Cystic dilatation of the cystic duct: a type 6 biliary cystIndian J Surg 2013 75:500-02. [Google Scholar]
[13]. Bhoil R, Sood S, Sood RG, Singla G, Bakshi S, A variant of type VI choledochal cyst: combined dilatation of cystic duct and common bile ductJ Ultrasound 2015 19:71-2. [Google Scholar]
[14]. Rohilla S, Singh D, Yadav RK, Bansal AR, Bala M, Diverticular choledochal cyst from cystic duct (TYPE VI VARIANT)SEAJCRR 2015 4:1320-25. [Google Scholar]