Idiopathic Fatal Pancytopenia: A Case Report
Hema Goyal1, Vijai Tilak2
1 Junior Resident, Department of Pathology, IMS, BHU, Varanasi, India.
2 Professor, Department of Pathology, IMS, BHU, Varanasi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hema Goyal, SE-357, Shastri Nagar, Ghaziabad-201002, India.
E-mail: hemagoyal88@gmail.com
Pancytopenia is defined as decrease in red blood cells, white blood cells and platelets. Many disease processes involve the bone marrow primarily or secondarily resulting in pancytopenia. A 55-year-old male presented with generalized body weakness and few episodes of malena for last one year. Physical and systemic examination was unremarkable. CBC report revealed pancytopenia. Other haematological parameters were within normal limit. Stool for occult blood was positive. USG and CECT abdomen showed no abnormality. The patient was evaluated for any evidence of malignancy but no clue was found. Bone marrow examination was done as patient was having pancytopenia. Bone marrow smears, clot sections and bone marrow biopsy was normal. Immunohistochemistry and cytogenetics study was unremarkable. Patient was admitted in hospital for 1 month and his condition rapidly deteriorated. The cause of pancytopenia remained unexplained and therefore it was named as Idiopathic fatal pancytopenia. “Idiopathic Fatal Pancytopenia (IFP)” is an emerging new entity with a grave prognosis. We wish to sensitize the medical community and the scientists to this rapidly fatal condition.
Cytogenetics, Idiopathic cytopenia of undetermined significance (ICUS), Immunohistochemistry
Case Report
A non-diabetic, non-hypertensive 55-year-old male patient presented with generalized body weakness and few episodes of malena since last one year. Physical examination of the patient revealed mild pallor, no clubbing, no jaundice, no lymphadenopathy and no pedal oedema. Informed consent was obtained from the patient.
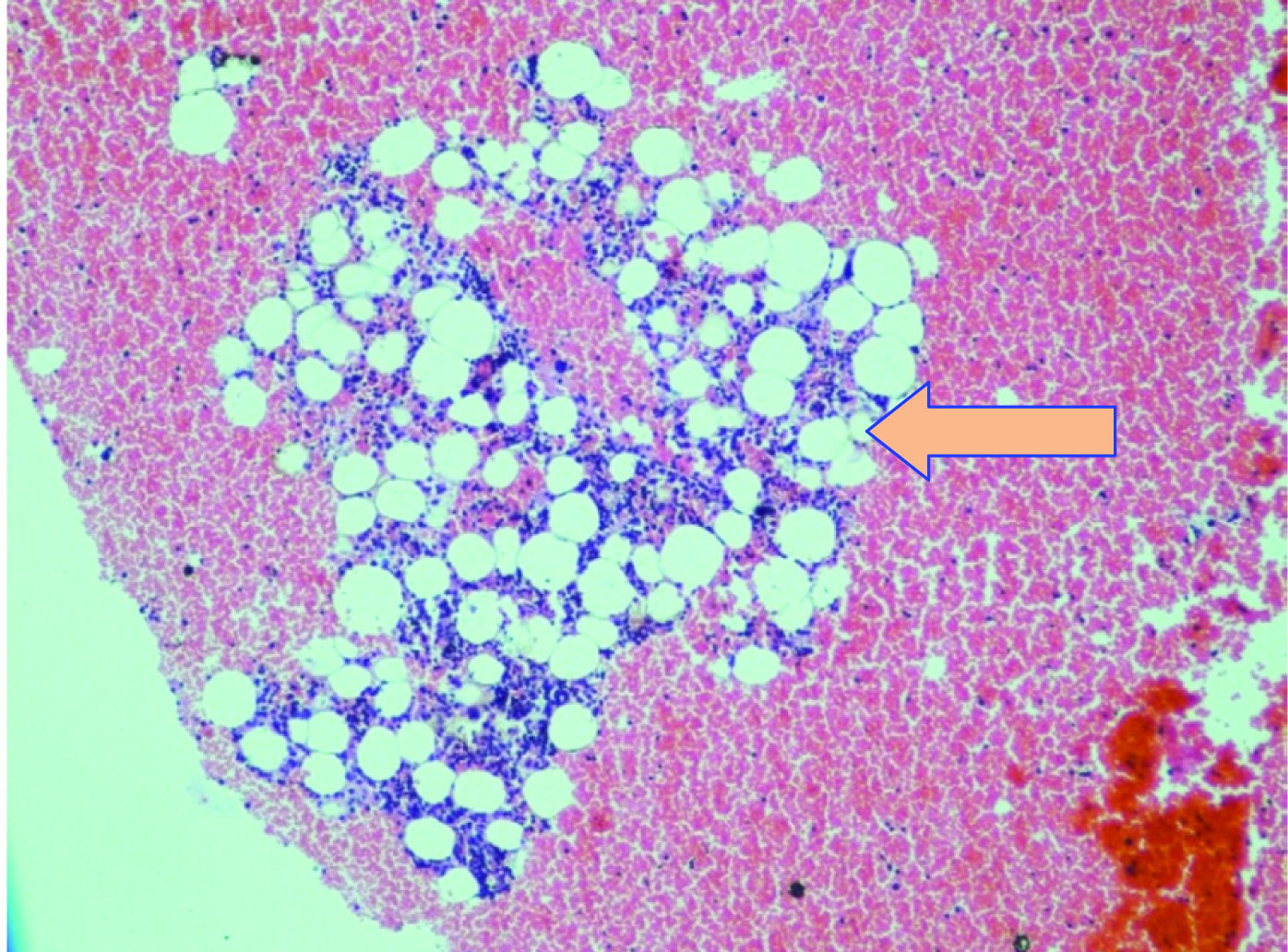
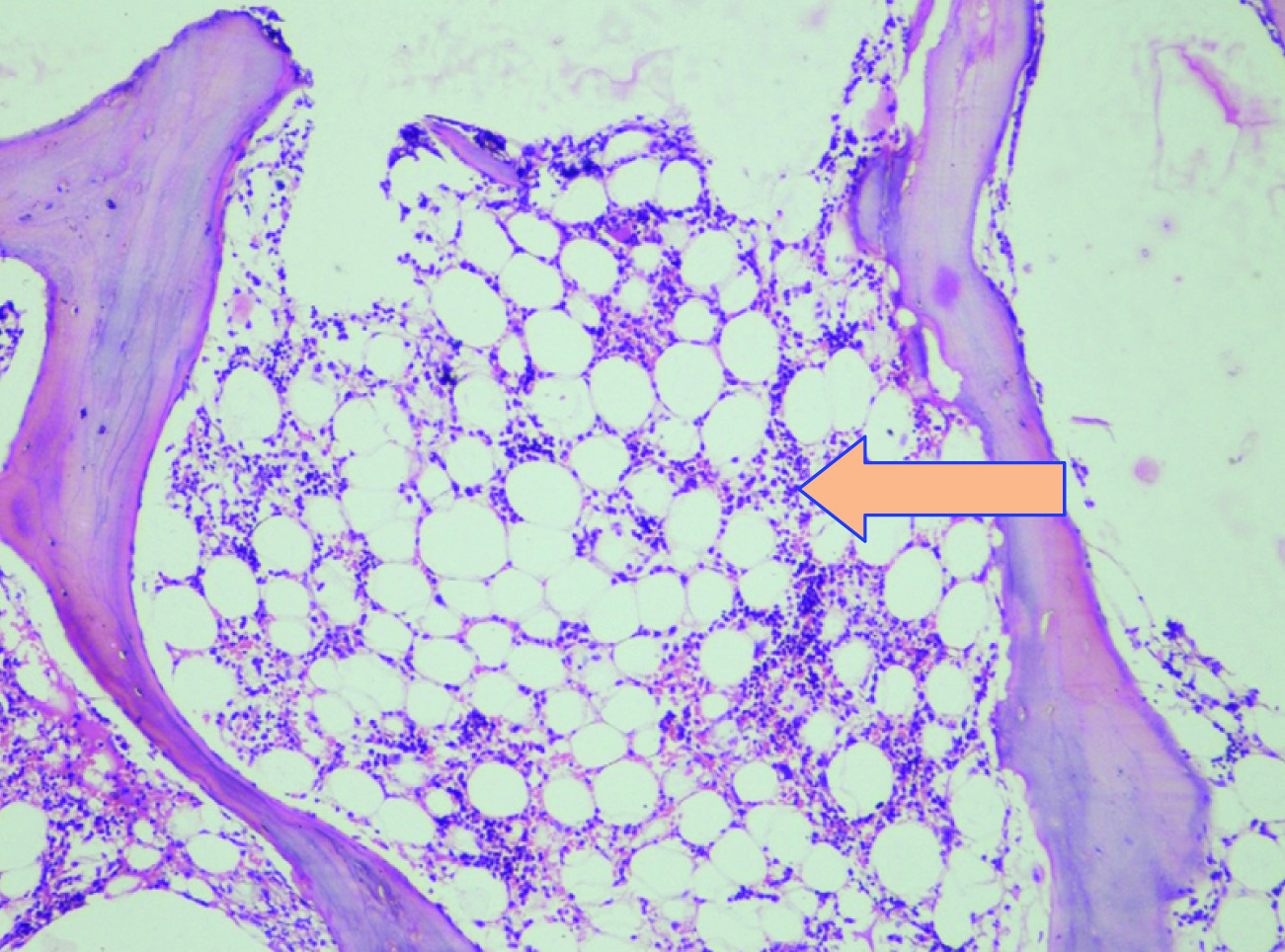
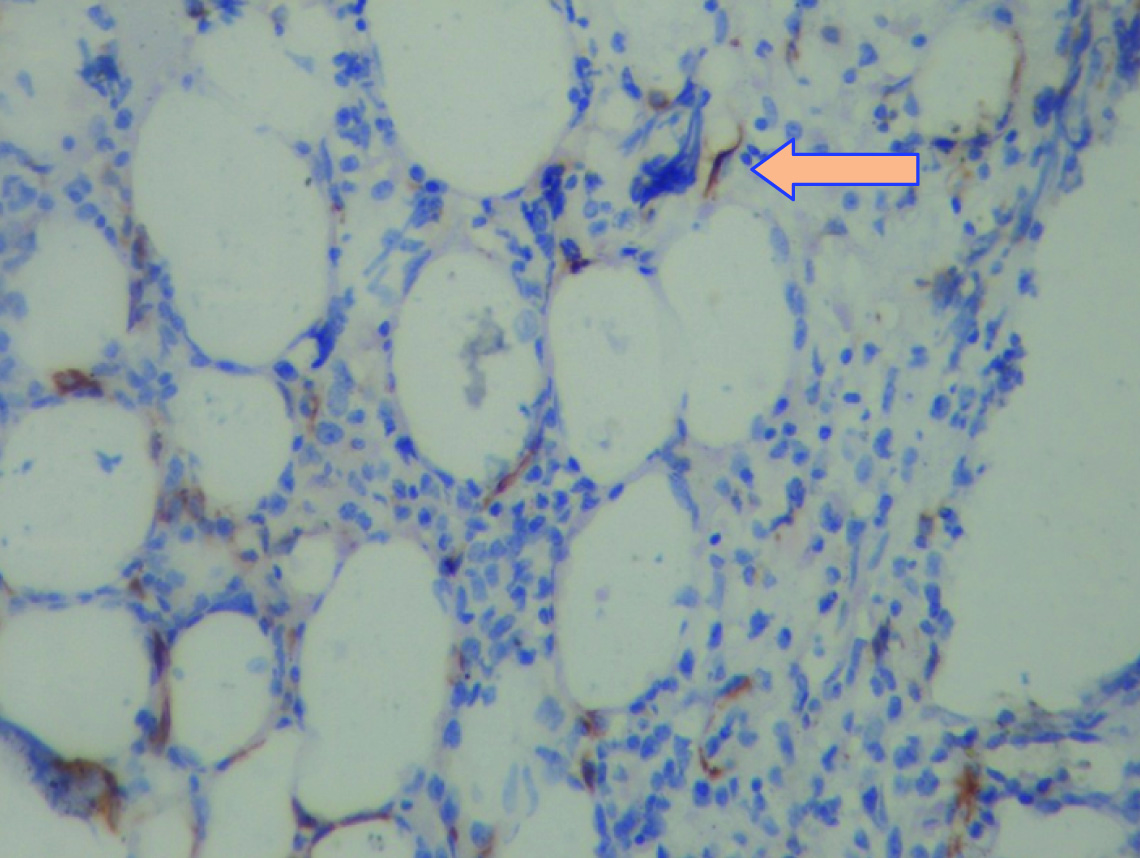
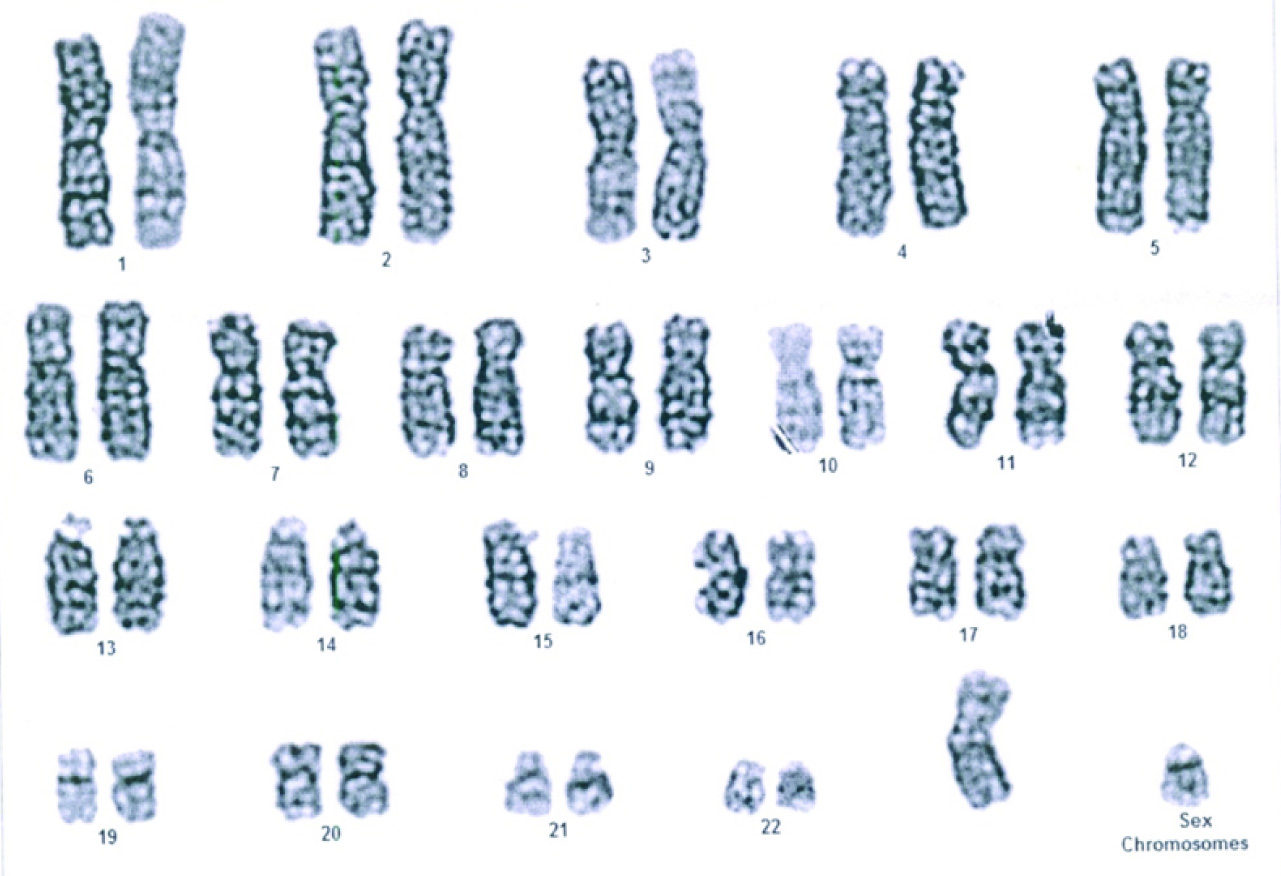
Systemic examination was within normal limit. There was no relevant history of intake of any drugs or previous radiation exposure. CBC revealed pancytopenia with Hb-9.5g/dl, TLC -3700 cells/cumm, Platelet count – 89,000 cells/cumm, RBC count – 3.17X106 /UL, MCH – 29.9pg, MCV – 88.2fl, MCHC – 34g/dl, RDW – 15.9%, Reticulocyte count was 0.9%. As per the previous records, patient was having pancytopenia since 8 months. Stool for occult blood was positive. Renal function test, liver function test, lipid profile was within normal limit. Clinically urine was straw coloured and urine routine microscopy was done to rule out microhaematuria. Serum LDH was 700 IU/L, S.Ferritin – 123.8 mg/dl, S.iron – 109mg/dl and TIBC – 89μg/dl. Bleeding time, PT(INR), APTT and coagulation profile was within normal limit. Ultrasound abdomen and KUB was done to rule any specific pathology but was normal. Viral markers (HBsAg, HIV, HAV, HCV, EBV), Dengue, paracheck, rk39 and leptospira (IgG & IgM) test were negative. Contrast enhanced CT scan was done and no evidence of any pathology was detected. As the patient had few episodes of malena, endoscopy was performed but it was within normal limits. Bone marrow examination was done and smears showed normal distribution of all lineage, no evidence of dysplasia, no increase in blasts and absence of ringed sideroblast on perl’s stain. Clot section revealed 5 normocellular particles and showed normal haematopoiesis [Table/Fig-1]. Bone marrow biopsy was also done, sections showed normocellular biopsy with normal distribution of haematopoiesis and no evidence of myelodysplasia noted [Table/Fig-2]. Immunohistochemistry with CD34 showed no increase in blast (<1%) [Table/Fig-3]. Cytogenetics was done on bone marrow aspirate and G banding was done and showed normal karyotype (46,XY) [Table/Fig-4].
Clot Section- section shows normocellular particle (Leishman, 20X).
Bone Marrow Biopsy: Section shows normocellular bone marrow with normal distribution of all lineages (Leishman, 10X).
IHC (CD34): Normal blood vessels are highlighted by CD34. No increase in blast is seen.
Cytogenetics study shows normal karyogram of the patient (46+XY)
During the stay in hospital, patients Hb, TLC and platelet counts were in declining trend shown in [Table/Fig-5].
Table shows haematological parameters of the patient during the stay in hospital.
| Parameters | At admission1st day | 8th day | 15th day | 20th day | 24th day | 26th day |
|---|
| HB(gm/dl) | 9.5 | 8.2 | 7.7 | 5.8 | 4.2 | 3.1 |
| TLC(cells/cumm) | 3700 | 3600 | 3600 | 3400 | 3400 | 2900 |
| Platelet(cells/cumm) | 89,000 | 85,000 | 60,000 | 53,000 | 50,000 | 27,000 |
Initially patient was started on symptomatic management. Patient was started on haematinic therapy but patient showed no improvement. On day 20 patients Hb dropped to 5.8gm/dl, then he was given two units of packed RBC transfusion (PRBC). There were no signs of active bleed. Despite the above measures patient did not improve clinically. On 24th day, patient had mild gum bleeding followed by nasal bleed, bleed through ryles tube and then several episodes of malena and haemetemesis. A repeat PT INR, APTT, Bleeding time and coagulation profile was done and was within normal limit. Patient developed respiratory distress, tachypnea, tachycardia along with persistent hypotension and went into haemorrhgic shock. After fluid resuscitation and blood transfusions, the patient vitals remain unstable. Ionotropes were started. Massive blood transfusion was given as per our institutional protocols. Due to persistent haemorrhgic shock, patient developed metabolic acidosis secondary to lactic acidosis and then refractory hyperkalaemia and went into cardiorespiratory arrest. The cause of pancytopenia remained unexplained and therefore was diagnosed as Idiopathic fatal pancytopenia.
Discussion
Pancytopenia is defined by reduction of all the three formed elements of blood below the normal reference range [1]. Variety of disorders, haematological and non-haematological can affect the bone marrow primarily or secondarily, resulting in the manifestation of pancytopenia [2]. In cases where a definite cause of persistent cytopenia (without dysplasia and without one of the specific cytogenetic abnormalities) cannot be determined, the condition is regarded as Idiopathic Cytopenia of Undetermined Significance (ICUS) and long term follow-up is recommended to assess the evolution [3].
Idiopathic cytopenia of undetermined significance (ICUS) [3,4] is a recently proposed, provisional diagnostic category that recognizes patients who present with cytopenias of undetermined etiology. The current proposed criteria for diagnosing ICUS include:
Persistent cytopenia (for 6 months): hemoglobin <11 g/dl, neutrophils <1.5 × 109L, and platelets <100×109/L;
No morphologic features of myelodysplasia;
Normal chromosome analysis and
A detailed clinical history and investigation that excludes other secondary causes of cytopenias.
These criteria suggest that there are three major components for an ICUS diagnosis: morphologic examination, cytogenetic analysis, and detailed clinical investigation.
The diagnosis of ICUS should only be established when all potential differential diagnoses (hepatopathy, infectious diseases, chronic inflammation, mastocytosis, others) have been excluded ICUS, a term was also proposed by Dr. G. Mufti (8th International Symposium on MDS, Nagasaki, Japan, 2005) and recommends long term follow up to assess the evolution [3].
The natural history of patients with ICUS is largely unknown and appears to be highly variable [5]. Small studies indicate that some patients will go on to develop frank MDS or a related myeloid malignancy such as AML [6]. Others may follow a more indolent course [7].
In our case, patient presented with persistent pancytopenia since 8 months and there is evidence of persistent decrease in haematological parameters further leading to death.
Wimazal F et al., published a series of 10 cases which were diagnosed as ICUS. All of them were followed up and the period of follow-up ranged from few months to few years [8]. It is pertinent to mention that all the 10 patients were alive at least for a period of six months. The term ‘undetermined significance’ was used in ICUS since the cytopenia was stable and the patient were alive for at least 6 months. In our case ICUS- pancytopenia could not be offered, as the entity was not of unknown significance but of grave significance as even after an exhaustive clinical and laboratory work-up, no cause of pancytopenia was found and the patient died without a definite diagnosis. We therefore suggest the term “Idiopathic fatal pancytopenia (IFP)” for such cases.
Various international studies reported few cases of pancytopenia with normal marrow which ranged from 3.38% to10.5% [9–12]. But no follow-up of the patient was described in these studies. No study has reported the phenomenon of IFP.
Conclusion
We report for the first time a new entity “Idiopathic Fatal Pancytopenia (IFP)” for pancytopenic patients in whom a definite etiology cannot be established even after an exhaustive workup and who eventually succumb to the complication of pancytopenia. Further research is necessary to elucidate the underlying pathology and potential drugs to halt the inevitable death.
[1]. Williams DM, Wintrobe’s Clinical Haematology 1993 10th editionBaltimoreWilliam and Wilkins:1449-84. [Google Scholar]
[2]. Khodke K, Marwah S, Buxi G, Vadav RB, Chaturvedi NK, Bone marrow examination in cases of pancytopeniaJ Academy Clin Med 2001 2:55-59. [Google Scholar]
[3]. Valent P, Horny HP, Bennett JM, Fonatsch C, Germing U, Greenberg P, Definitions and standards in the diagnosis and treatment of the myelodysplastic syndromes: Consensus statements and report from a working conferenceLeukemia Research 2007 (31):727-36. [Google Scholar]
[4]. Valent P, Bain BJ, Bennett JM, Wimazal F, Sperr WR, Mufti G, Idiopathic cytopenia of undetermined significance (ICUS) and idiopathic dysplasia of uncertain significance (IDUS), and their distinction from low risk MDSLeukemia Research 2012 (36):1-5. [Google Scholar]
[5]. Kwok B, Hall JM, Witte J S, Xu Y, Reddy P, Lin K, MDS-associated somatic mutations and clonal haematopoiesis are common in idiopathic cytopenias of undetermined significanceBlood 2015 126(21):2355-61. [Google Scholar]
[6]. Schroeder T, Ruf L, Bernhardt A, Hildebrandt B, Aivado M, Aul C, Distinguishing myelodysplastic syndromes (MDS) from idiopathic cytopenia of undetermined significance (ICUS): HUMARA unravels clonality in a subgroup of patientsAnn Oncol 2010 21(11):2267-71. [Google Scholar]
[7]. Busque L, Patel JP, Figueroa ME, Vasanthakumar A, Provost S, Hamilou Z, Recurrent somatic TET2 mutations in normal elderly individuals with clonal haematopoiesisNat Genet 2012 44(11):1179-81. [Google Scholar]
[8]. Wimazal F, Fonatsch C, Thalhammer R, Schwarzinger I, Müllauer L, Sperr WR, Idiopathic cytopenia of undetermined significance (ICUS) versus low risk MDS: the diagnostic interfaceLeuk Res 2007 31:1461-68. [Google Scholar]
[9]. Jha A, Sayami G, Adhikari RC, Patna AD, Jha R, Bone marrow examination in cases of pancytopeniaJ Nepal Med Assoc 2008 47:12-17. [Google Scholar]
[10]. Pathak R, Jha A, Sayami G, Evaluation of bone marrow in patients with pancytopeniaJournal of Pathology of Nepal 2012 2:265-71. [Google Scholar]
[11]. Lakhey A, Talwar OP, Singh VK, KC SR, Clinico-haematological study of pancytopeniaJournal of Pathology of Nepal 2012 (2):207-10. [Google Scholar]
[12]. Pudasaini S, Prasad KBR, Rauniyar SK, Shrestha R, Gautam K, Pathak R, Interpretation of bone marrow aspiration in haematological disorderJournal of Pathology of Nepal 2012 2:309-12. [Google Scholar]