The mental foramen is located on either side of the mandible just below the corners of the lips around the region of the root of the second premolar tooth. The mental nerve and associated blood vessels emerge from the mental foramen. The mental nerve provides sensation to the lower central portion of the face [1,2]. Dentists, oral maxillofacial surgeons, emergency physicians and plastic and reconstructive surgeons are required to be knowledgeable regarding the anatomy of the mental foramen and variations in its position for the purposes of achieving local anaesthesia as well as the planning of various surgical procedures [3].
The position of the mental foramen has been well researched in cadaver specimens, radiographically as well as intraoperatively [4–6]. Thus far panoramic radiographs, periapical radiographs, Magnetic Resonance Imaging (MRI), Conebeam Computed Tomography (CBCT), Spiral Computed Tomography (SCT) and Multi Slice Computed Tomography (MSCT) have all been studied by clinicians to determine the position of the mental foramina [7–12]. Limitations with these modalities include radiation exposure and resultant increased risk of malignancy, increased cost, increased time and the possibility of not detecting the mental foramen [13,14]. Many of these modalities are also not readily available in the developing country setting as well as in lower level of care facilities. The mental foramen and the various modalities useful in locating the mental foramen have been reviewed in detail elsewhere [15].
Materials and Methods
Study design and patient assessment
This prospective, cross-sectional observational study was conducted in a single centre ED (Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), Johannesburg, South Africa) between February 2012 and March 2013. CMJAH is a tertiary care facility in a large urban environment and is affiliated with the University of the Witwatersrand.
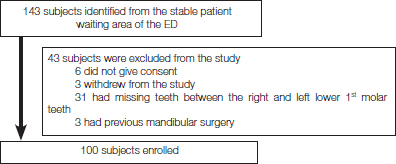
We enrolled a convenience sample of 100 Adult Black and Caucasian (White and Asian) patients, older than 18 years that presented to the CMJAH ED. These patients had passed through the hospital’s triage system and did not require urgent or emergent treatment. Patients did not present with pathology requiring a mental nerve block. Individuals with congenital/acquired facial distortion, a history of mandibular surgery and patients who had mandibular teeth missing between the right and left lower 1st molars were excluded from the study. Details of patient recruitment and exclusion are listed in the flow diagram in [Table/Fig-1].
Exclusions and final sample for analysis.
Subjects were enrolled in the study and written informed consent was obtained. Confidentiality was respected at all times. Data collection sheets did not include personal data. Only relevant demographic data was included. The information gathered was protected by a coded numbering system, which was stored in a password-protected computer that was only accessible to the researchers. Permission to conduct the study was obtained from the Head of Department (HOD) of the CMJAH ED and the hospital management. Clearance was obtained from the Human Research Ethics Committee of the University of the Witwatersrand (certificate no. M110920).
All ultrasound examinations and data collection was conducted by the primary investigator who is emergency ultrasound certified by College of Emergency Medicine of South Africa (official specialist certification body in South Africa). The research was fully supervised by a faculty member of the division of emergency ultrasound of the College of Emergency Medicine of South Africa. Patients were randomly selected from the queue at a time convenient to the researcher. The last patient waiting in the queue was approached first and so on, so as not to increase patient waiting times. Potential participants were given an information leaflet.
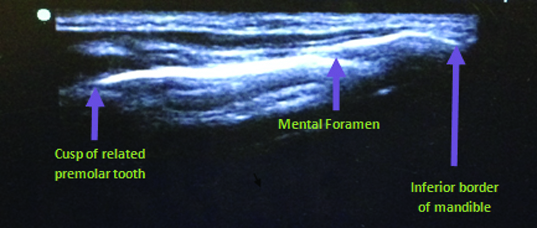
Individuals who volunteered to participate in the study were asked to follow the researcher to a private cubicle. Participants were then questioned regarding exclusion criteria. Individuals who were not eligible to participate were thanked and taken back to their place in the queue. Eligible volunteers, who agreed to participate, were requested to sign informed consent. They were then allocated a participant number to maintain anonymity. The investigation was carried out in the supine position. We used a Toshiba diagnostic ultrasound system (model SSA-510A, serial no. P3C06X5875) and a high frequency (8MHz) transducer (PLF.805ST) with the machine set on the “small parts” preset mode. Sonar gel was applied to the ultrasound transducer once the machine was in running mode. The transducer, with the marker pointing to the participant’s head (cranially), was gently applied above the inferior border of the mandible and just lateral to the mentum. The mental foramen was identified under ultrasound guidance and its relation to the closest mandibular premolar tooth recorded. The mental foramen is easily identified in this region as a break in the continuity of the bone [Table/Fig-2]. There are no other similar ultrasonographic structures that can be confused with the mental foramen in this vicinity. The above procedure was repeated on the opposite side of the face. After documenting relevant data, excess gel was gently cleaned off and the volunteer thanked. All volunteers, as far as possible, maintained their position in the queue waiting to see their clinician. Any difficulties experienced during the investigation were documented.
Ultrasound image of the mental foramen and its hard tissue relations. The mental foramen is easily identified as a break in the continuity of the bone between the corner of the mouth and the inferior border of the mandible.
Statistical Analysis
All data was captured from the data collection sheets by the primary investigator and entered into an electronic spreadsheet (Microsoft® Excel®). STATA ® version12.1 software (StataCorp LP) was used to analyze all data. Each volunteer was placed in an age category: a) 18-30 years; b) 31-40 years; c) 41-50 years; d) 51-60 years; e) 61-70 years. A cross table was used to compare race, gender and age with the position of the mental foramen. The Fisher’s-exact test was used to assess for relationships between two categorical variables (positions 1 – 5 versus age group, gender, and race). Study reporting conformed to STROBE guidelines [18].
Results
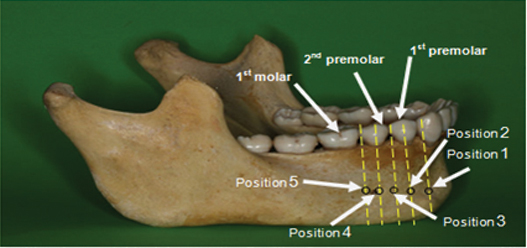
The total sample of 100 subjects consisted of 50 Blacks (27 males and 23 females) and 50 Caucasians (23 males and 27 females). The Caucasians were further subdivided into 25 Asians (13 males and 12 females) and 25 Whites (10 males and 15 females). The overall sex distribution was equal (50 males and 50 females). The overall mean age of the study population was 35.7 years (SD 1.9 years). Sixty nine percent of subjects were under the age of 40 years and only 2% of subjects were older than 60 years. The reason that most of our subjects were under 40 years of age is due to the fact that with advancement in age, the incidences of missing teeth between the right and left mandibular 1st molars are higher. Twenty-two patients older than 60 years were excluded from the study as they had missing teeth between the right and left 1st mandibular molars. All mental foramina (100%) were ultrasonographically identified. The position of the mental foramen was described as: Position 1 - mesial to the 1st premolar; Position 2 - in line with the long axis of the 1st premolar; Position 3 - between 1st and 2nd premolars; Position 4 - in line with the long axis of the 2nd premolar and Position 5 - lateral to 2nd premolar.
[Table/Fig-3] describes the various possible positions of the mental foramen and its vertical relationship to the long axis of the mandibular teeth. [Table/Fig-4] describes the impact of race, sex and age on the position of the mental foramen with regard to the long axis of the mandibular teeth. Fisher’s exact test was used to assess for statistical significant for all comparisons.
Dry mandible specimen and the various possible positions of the mental foramen (black circles) and its vertical relationship to the long axis of the mandibular teeth (yellow lines).
Position 1- mesial to 1st premolar. Position 2- in line with the long axis of the 1st premolar. Position 3-between 1st and 2nd premolar. Position 4- in line with the long axis of the 2 and premolar. Position 5-lateral to 2nd premolar.
The impact of race, sex and age group on the position of the mental foramen with regard to hard tissue relations.
| Position 1 | Position 2 | Position 3 | Position 4 | Position 5 | Statistical Significance (Fisher’s-exact test) |
|---|
| Entire group R | 1% | 12% | 41% | 44% | 2% | N/A |
| Entire group L | 1% | 9% | 44% | 43% | 3% |
| Blacks R | 0% | 8% | 36% | 52% | 4% | p = 0.26 |
| Asians R | 4% | 12% | 40% | 44% | 0% |
| Whites R | 0% | 20% | 52% | 28% | 0% |
| Blacks L | 0% | 6% | 38% | 50% | 6% | p = 0.12 |
| Asians L | 4% | 8% | 40% | 48% | 0% |
| Whites L | 0% | 16% | 60% | 24% | 0% |
| Males R | 2% | 8% | 42% | 46% | 2% | p = 0.77 |
| Females R | 0% | 16% | 40% | 42% | 2% |
| Males L | 2% | 4% | 44% | 46% | 4% | p= 0.39 |
| Females L | 0% | 14% | 44% | 40% | 2% |
| 18-30 years R | 2.5% | 12.5% | 47.5% | 35% | 2.5% | p = 0.52 |
| 31-40 years R | 0% | 6.9% | 44.8% | 48.3% | 0% |
| 41-50 years R | 0% | 18.7% | 25% | 50% | 6.3% |
| 51-60 years R | 0% | 7.7% | 30.8% | 61.5% | 0% |
| 61-70 years R | 0% | 50% | 50% | 0% | 0% |
| 18-30 years L | 2.5% | 10% | 50% | 35% | 2.5% | p = 0.14 |
| 31-40 years L | 0% | 3.4% | 48.3% | 48.3% | 0% |
| 41-50 years L | 0% | 18.8% | 18.8% | 50% | 12.4% |
| 51-60 years L | 0% | 0% | 46.1% | 53.9% | 0% |
| 61-70 years L | 0% | 50% | 50% | 0% | 0% |
R - Right mental foramen position. L - Left mental foramen position. VR - Vertical hard tissue relation on the right side. VL - Vertical hard tissue relation on the left side. Position 1 - mesial to 1st premolar. Position 2 - in line with the long axis of the 1st premolar. Position 3 - between 1st and 2nd premolars. Position 4 - in line with the long axis of the 2nd premolar. Position 5 - lateral to 2nd premolar.
Overall the most frequent position of the mental foramen in relation to vertical hard tissue landmarks was at position 4 on the right (44%) and position 3 on the left (44%). They were closely followed by position 3 on the right (41%) and position 4 on the left (43%). In 4% or less of subjects, the mental foramen was located at position 1 (mesial to the 1st premolar) and position 5 (lateral to the 2nd premolar).
There were no statistically significant differences (p> 0.05) between race groups with regard to the position of the mental foramen in relation to the mandibular premolars on both the right and left sides. In Blacks, the most frequent position of the mental foramen was at position 4 on the right (52%) and left (50%) sides. The second most common position was at position 3 with a frequency of 36% on the right and 38% on the left side. In Asians, the most frequent position of the mental foramen was found to be slightly more frequently at position 4 on the right (44%) and left (48%) sides, then at position 3 with a frequency of 40% on both the right and left sides. In Whites, the most frequent position of the mental foramen was at position 3, on the right (52%) and left (60%) sides. The second most common position was at position 4 with a frequency of 28% on the right and 24% on the left .
There were no statistically significant differences between females and males with regard to the position of the mental foramen and its relation to the mandibular premolars on both the right and left sides (p=0.766 and p=0.387 respectively). The most frequent position of the mental foramen in females was at position 4 on the right (42%) and position 3 on the left (44%) side. The second most common position was at position 3 on the right with a frequency of 40% and position 4 on the left with a frequency of 40%. The most frequent position of the mental foramen in males on the right was at position 4 (46%) and then position 3 at 42%. On the left it was most frequently found at position 4 (46%) and then position 3 at 44%.
There were no statistically significant differences (p >0.05) between the various age categories with regard to the position of the mental foramen in relation to the mandibular premolars on both the right and left sides. The most common position of the mental foramen in subjects in the age group category 18-30 years was at position 3 on the right and left sides. In patients aged 31-60 years position 4 was the most common position, with higher frequencies of subjects at position 4 with advancement of age. In 4% or less of patients, the mental foramen was positioned at position 1 or 5 on both the right and left sides.
Discussion
The position of the mental foramen and its relation to the long axis of the mandibular premolars has been well described in the literature [1,2,10,19,20]. To our knowledge, this landmark study is the first to make use of ultrasonography in a study population to determine the position of the mental foramen.
We did not find any statistically significant differences between race groups, gender and age categories with regard to the position of the mental foramen in relation to the mandibular premolars on both the right and left sides (p >0.05 for all categories).
However, in Blacks the most common position was in line with the long axis of the second mandibular premolar (52% on the right and 50% on the left). In Asians, the most frequent position of the mental foramen was found slightly more frequently in line with the long axis of the 2nd mandibular premolar (44% on the right and 48% on the left) followed closely by position 3, which is between the 1st and 2nd mandibular premolars (40% on either side). In Whites, the most frequent position of the mental foramen was between the 1st and 2nd mandibular premolars on the right (52%) and left (60%) sides.
[Table/Fig-5] Summarizes the most common position of the mental foramen in various population groups previously studied [1,2,5,6,19–41].
Summary of the various population groups reviewed with regard to the position of the mental foramen.
| Author | Year | Population group | Race | Study size | Study method | Most common position* |
|---|
| Africa – North to South |
| Mbajiorgu E et al., [20] | 1998 | Zimbabwean | Black | 32 | Cadaver | B |
| Igbigbi P et al., [21] | 2005 | Malawian | Black | 70 | Cadaver | B |
| Fabian F [22] | 1976 | Tanzanian | Black | 100 | Cadaver | B |
| Mwaniki D et al., [23] | 1992 | Kenyan | Black | 79 | Cadaver | B |
| Olasoji H et al., [19] | 2004 | Nigerian | Black | 157 | PR | A |
| Asia – East to West |
| Kim I et al., [6] | 2006 | Korean | Asian | 112 | Intra-op and PR | B |
| Green R [24] | 1987 | Chinese | Asian | 87 | Cadaver | B |
| Guo J et al., [25] | 2009 | Chinese | Asian | 21 | Cadaver | B |
| Ngeow W et al., [26] | 2003 | Malaysian | Asian | 169 | PR | B |
| Neo J [5] | 1989 | Singaporean | Asian | 158 | PR | B |
| Shankland W [27] | 1994 | Indian | Asian | 69 | Cadaver | B |
| Sankar D et al., [28] | 2011 | Indian | Asian | 90 | Cadaver | A |
| Udhaya K et al., [29] | 2013 | Indian | Asian | 90 | Cadaver | B |
| Gada S et al., [30] | 2014 | Indian | Asian | 300 | PR | A |
| Haghanifar S et al., [2] | 2009 | Iranian | Asian | 400 | PR | A |
| Khojastepour L et al., [31] | 2015 | Iranian | Asian | 156 | CBCT | B |
| Al Jasser N et al., [32] | 1998 | Saudi Arabian | Asian | 414 | PR | B |
| Al–Khateeb T et al., [1] | 2007 | Jordanian | Asian | 860 | PR | A |
| Europe & North America – East to west |
| Aktekin M et al., [33] | 2003 | Turkish | White | 58 | Cadaver | A |
| Yesilyurt H et al., [34] | 2008 | Turkish | White | 70 | Cadaver | B |
| Kqiku L et al., [35] | 2013 | Kosovarian | White | 500 | PR | A |
| Smajilagic A et al., [36] | 2004 | Bosnian | White | 20 | Cadaver | B |
| Voljevica A et al., [37] | 2015 | Bosnian | White | 150 | Cadaver | B |
| Phillips J et al., [38] | 1992 | North American | White | 75 | PR | B |
| Moiseiwitsch J [39] | 1998 | North American | White | 105 | Cadaver | A |
| Pria C et al., [40] | 2011 | North American | White | 500 | PR | A |
| South America |
| Chu R et al., [41] | 2014 | Brazilian | | 191 | Cadaver | A |
PR – panoramic radiograph, CT – computed tomography, CBCT – cone beam computed tomography
* Most common position in relation to the mandibular premolar teeth: A – between the 1st and 2nd premolars; B – in line with the long axis of the 2nd premolar.
Overall, in only 3% of cases on the right and 4% of cases on the left, the mental foramen was found to be mesial to the 1st premolar or lateral to the 2nd premolar. When the mental foramen was found mesial to the 1st premolar, frequencies of between 1% and 5% have been reported in the literature [1,5,26,42]. Frequencies of between 4% and 51.5% have been reported for the position lateral to the 2nd premolar [1,10,22,42,43]. Shah and colleagues in their study commented that the mental foramen lies either mesial to the first premolar or lateral to the first molar in only 1–2% of cases [44].
A limitation to our study is that we excluded patients with congenital / acquired facial distortion, patients with a history of mandibular surgery and patients who had mandibular teeth missing between the right and left lower 1st molars. Perhaps the mental foramen may not have been as easily found with ultrasonography in these patients as a result of positional change or distortion of the mental foramen. Chrcanovic et al., reported a change in the position of the mental foramen with age and loss of teeth. With loss of teeth and resultant bone resorption, the alveolar crest shifts downwards and closer to the mental foramen [45]. Another study reported that the mental foramen was situated at an average of 3.8mm lower in edentulous jaws than in dentulous jaws with respect to a superior reference point (the alveolar crest) [46]. A study in Hong Kong found there to be a significant correlation between tooth wear and position of the mental foramen [4]. Since only two subjects in our study were older than 60 years, we cannot fully comment on the effect of ageing on the position of the mental foramen.
Earlier studies [Table/Fig-5] used various methods such as cadaver specimens, various radiological modalities as well as intraoperative studies to determine the location of the mental foramen. In terms of radiological modalities, panoramic radiographs, periapical radiographs, Magnetic Resonance Imaging (MRI), Cone Beam Computed Tomography (CBCT), Spiral Computed Tomography (SCT) and Multi Slice Computed Tomography (MSCT) have all been studied by clinicians to determine the position of the mental foramina [7–12].
Periapical and panoramic radiographic techniques have their limitations. Linear measurements may need to be corrected for rotation and radiographic distortion [14]. In a study by Bou and colleagues, there was a tendency for panoramic radiographs to overestimated distances when compared to spiral or computed tomography [7]. Panoramic X-rays also distort the position of the mental foramen as they do not take curvatures and angling of the mandible into account [6,38,47]. Size reduction through compression has also been shown to effect image quality [48]. In contrast, in the study by Phillips et al., on PR’s there was a 23% increase in size and a distal shift of the mental foramen [38]. Forni et al., also found that images on panoramic radiographs were magnified by 36.6% compared to computed tomography [49]. Periapical and panoramic radiographs are also limited in their ability to detect the mental foramen. Two studies in this line only detected the mental foramen in 84% and 94% of panoramic radiographs respectively [14,50] and the second of these studies commented that only 49% of mental foraminae were clearly visible [14]. With periapical views, the yield is even lower. A study conducted by Fishel et al., using periapical films reported that the mental foramen was detected in only 46.8% of cases [51]. In contrast our study detected the mental foramen, bilaterally in all enrolled subjects. This suggests that ultrasound may be more sensitive than periapical and panoramic radiographs in detecting the mental foramen. With regard to other radiological modalities, CBCT was superior to MSCT in detecting the mental foramen and also used lower radiation doses [11]. Another study found MRI to be more accurate than CBCT in determining the position of the mental foramen and nerve [9]. The drawback with these modalities is much higher radiation doses, increased cost, the need for a radiology service and extra time taken to transport the patient to the radiology department and to carry out the investigation.
Ultrasound
Ultrasonography is a cost effective, safe, time saving, non-invasive modality with no risk of radiation exposure and can be performed at the bedside. It may be used as a diagnostic as well as an interventional tool in medicine [13,16]. Its use in anaesthesia and the emergency department for regional nerve block anaesthesia has been well described [37]. Another potential benefit is that the mental nerve may be blocked under direct vision, using real time ultrasound guidance as a tool. This would increase first time success rates, decrease failure rates and decrease the chances of neurological injury in trained and experienced hands [17].
Traxler et al., used ultrasound to determine the alveolar ridge width for purposes of dental implants. He also commented that ultrasound provided accurate information about the position of the mental foramen, as a secondary finding [52].
A limitation to the use of ultrasound is the fact that ultrasonography is operator dependent [16]. Therefore all ultrasound examinations and data collection was conducted by the primary investigator who is emergency ultrasound certified by the College of Emergency Medicine of South Africa. The study was fully supervised by a faculty member of the division of emergency ultrasound of the College of Emergency Medicine of South Africa.
Conclusion
In conclusion, point of care/hand held ultrasound devices and recent developments in 3D ultrasound have the potential to revolutionize the practice of dento-maxillofacial surgery. Further studies using ultrasound to locate not only the mental foramen, but also other clinically important related anatomy in the vicinity are required.
R - Right mental foramen position. L - Left mental foramen position. VR - Vertical hard tissue relation on the right side. VL - Vertical hard tissue relation on the left side. Position 1 - mesial to 1st premolar. Position 2 - in line with the long axis of the 1st premolar. Position 3 - between 1st and 2nd premolars. Position 4 - in line with the long axis of the 2nd premolar. Position 5 - lateral to 2nd premolar.
PR – panoramic radiograph, CT – computed tomography, CBCT – cone beam computed tomography
* Most common position in relation to the mandibular premolar teeth: A – between the 1st and 2nd premolars; B – in line with the long axis of the 2nd premolar.