A Rare Case of Tamarind Seed Induced Oral Submucous Fibrosis in a 12-Year-Old Indian Boy
Mamata Sharad Kamat1, Rudrayya Shivanand Puranik2, Neelkamal Halappa Hallur3, Varsha Vimal Kumar4, Sharad Basavaraj Kamat5
1 Reader, Department of Oral Pathology and Microbiology, Bharati Vidyapeeth Deemed University Dental College and Hospital, Sangli, Maharashtra, India.
2 Professor and Head, Department of Oral Pathology and Microbiology, PMNM Dental College and Hospital, Bagalkot, Karnataka, India.
3 Professor and Head, Department of Oral and Maxillofacial Surgery, Al Badar Dental College and Hospital, Gulbarga, Karnataka, India.
4 Senior Lecturer, Department of Oral Pathology and Microbiology, Rajarajeshwari Dental College and Hospital, Bangalore, Karnataka, India.
5 Professor and Head, Department of Conservative Dentistry and Endodontics, Bharati Vidyapeeth Deemed University Dental College and Hospital, Sangli, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mamata Sharad Kamat, Reader, Department of Oral Pathology and microbiology, BVDU Dental College and Hospital, Wanlesswadi, Sangli-Miraj Road, Sangli-416414, Maharashtra, India.
E-mail: kmamata@yahoo.com
Oral Submucous Fibrosis (OSMF) is a chronic debilitating, potentially malignant disorder of the oral cavity. It is characterized by restricted mouth opening which results due to abnormal accumulation of collagen in the sub-epithelial layers leading to dense fibrous bands in the mouth. The pathogenesis of the disease is believed to be multifactorial. However, literature reports suggest a strong association of OSMF and arecanut chewing habit. The present paper presents a case of OSMF in a 12-year-old boy without arecanut chewing habit, but with a heavy practice of chewing tamarind seeds.
Alkaloids, Copper, Tannins
Case Report
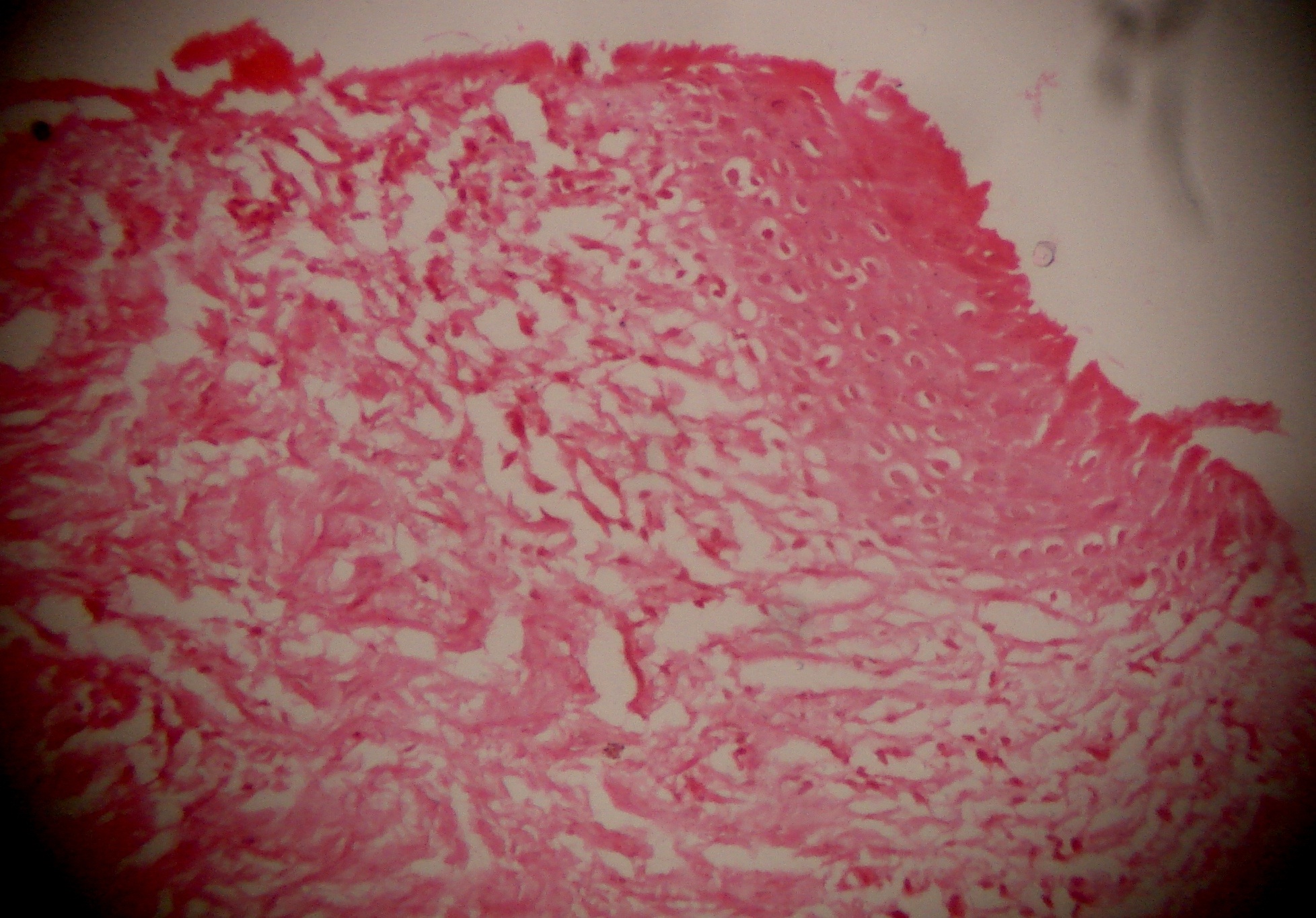
A 12-year-old boy reported to the Department of Oral Pathology and Microbiology, PMNM Dental College and Hospital, Bagalkot, Karnataka, India, with a chief complaint of restricted mouth opening since three years. The patient also gave history of burning sensation of oral mucosa on taking spicy food since two years. The patient did not have arecanut or tobacco chewing habit. The patient revealed a long standing history of chewing raw and roasted tamarind seeds, about 15-20 seeds, two to three times a day since five years. Intra oral examination revealed blanching of oral mucosa [Table/Fig-1a,1b), palpable vertical and circular fibrous bands and shortening of uvula. The mouth opening (interincisal distance) was reduced to 21mm [Table/Fig-2]. The patient was advised for complete blood investigation. All haematological values were within normal limits with no evidence of anaemia. An incisional biopsy from buccal mucosa was performed and the tissue was subjected for histopathological examination. Haematoxylin and eosin stained sections of the submitted specimen showed atrophic stratified squamous parakeratinised epithelium with flat epithelial connective tissue interface. Underlying connective tissue showed thickened bundles of collagen fibres with areas of hyalinization [Table/Fig-3]. Moderate amount of vascularity with few inflammatory cells was also noted. Based on information of history from parents, clinical examination and histopathology, the final diagnosis of tamarind seed induced OSMF was rendered.
Clinical picture showing blanching of buccal mucosa.

Clinical picture showing blanching of palate mucosa.

Clinical picture showing interincisal distance (21 mm).

Haematoxylin and eosin stained section showing atrophic epithelium and thickening of collagen fibre bundles (10X magnification).
Discussion
OSMF is a chronic insidious, high risk, potentially malignant disorder with a reported malignant transformation rate of 7.6% [1]. Literature reports reveal that 2.5 million people are affected by this disease worldwide. Hence, OSMF is considered as a public health issue globally, including UK, South Africa and many Southeast Asian countries [2]. OSMF is reported in patients with wide age range, but most often seen between 20 to 40 years [3]. Various factors have been postulated to trigger the disease process including arecanut chewing, ingestion of chillies, genetic and immunologic processes, nutritional deficiencies and other factors. However, studies reveal that components of arecanut play an important role in the pathogenesis of OSMF. Various alkaloids present in arecanut, in dose dependant manner, stimulate fibroblast proliferation and cause increased collagen formation. It is also suggested that large quantities of tannin present in arecanut reduces collagen degradation by inhibiting collagenases. Hence, the combined effect of tannins and alkaloids present in areca nut forms the basis for fibrosis. The other hypothesis of increased collagen in OSMF patients is thought to be due to the presence of high copper content in arecanut and subsequent upregulation of copper dependant enzyme, lysyl oxidase [2,4]. However, it was surprising to know that the boy in the present case was habituated to chew tamarind seeds during the playtime and school hours.
Considering these above mentioned facts, the occurrence of OSMF in a 12-year-old child, absence of arecanut chewing habit and the associated practice of heavy tamarind seed chewing habit make the present case unique.
In India, tamarind seeds are eaten by the rural people/certain ethnic groups such as Kurumba, Iulas, Malayali and Dravidian tribes [5]. The testa (seed coat) is removed, roasted or boiled and are eaten instead of betel nut. The roasted seeds are claimed to be superior to peanuts in flavour [6]. However, the patient in the present case practiced chewing both raw and roasted seeds. Tamarind seeds contain high levels of proteins and lipids and other nutrients with good nutritional quality. The seeds have been reported to exhibit potential antidiabetic, antihyperlipidemic and antioxidant activity. Literature reveal that despite the desirable nutritional features, the presence of certain anti-nutritional compounds (like total free phenolics, tannins, L-Dopa, phytic acid, oligosaccharides, lectins and protease inhibitors) make the whole tamarind seeds unsuitable for human consumption. Presence of high levels of total free phenolics and tannins especially in the seed coat necessitates the removal of seed coat [5].
Literature also suggested that tamarind seeds contain alkaloids like colchines and vinca. The presence of alkaloids in the tamarind seeds is of interest because alkaloids have dual functions. At low concentrations, these alkaloids are capable of inhibiting mitotic cell division; phagocytosis and can encourage lymphotoxic activities that are dangerous to health. At high concentrations seed alkaloids are toxic [7]. The other factor is that the copper content of tamarind seeds range from 1.6 – 19 mg/100g [6]. However, the recommended average daily intake of copper from diet in developing countries is between 0.6 – 1.6 mg/day [8]. Prolonged chewing of tamarind seeds in the present case might also be linked to increased availability of copper released by seeds which also play an important role in collagen synthesis.
To the best of our literature search, cases of OSMF associated with tamarind seed chewing habit have not been reported previously. Considering the presence of tannins, certain alkaloids and increased release of copper from tamarind seeds, the heavy, prolonged, continuous, daily intake of tamarind seeds may be involved in the causation of OSMF in the present case as the other factors related to OSMF were not observed.
Conclusion
It is plausible that this case report illustrates tamarind seed as a non-arecanut based source of alkaloid as an etiologic agent of OSMF. However, further research with more number of such reports is required to clarify the biological mechanisms involved. The present case report also highlights the need for awareness of such an association among health professionals, so that appropriate preventive measures and treatment can be rendered.
[1]. Rajendran R, Oral submucous fibrosis: etiology, pathogenesis, and future researchBull World Health Organ 1994 72:985-96. [Google Scholar]
[2]. Rajalalitha P, Valli S, Molecular pathogenesis of oral submucous fibrosis- a collagen metabolic disorderJ Oral Pathol Med 2005 34:321-28. [Google Scholar]
[3]. Pindborg JJ, Odont Copenhagen Sirsat SM, Oral submucous fibrosisOral Surg Oral Med Oral Pathol 1996 22(6):764-79. [Google Scholar]
[4]. Tilakaratne VM, Klinikowski MF, Saku T, Peters TJ, Warnakulasuriya S, Oral submucous fibrosis: review on aetiology and pathogenesisOral Oncol 2006 42:561-68. [Google Scholar]
[5]. Vadivel V, Pugalenthi M, Evaluation of nutritional value and protein quality of an under-utilized tribal food legumeIndian J Tradit Knowle 2010 9:791-97. [Google Scholar]
[6]. El-Siddig K, Gunasena HPM, Prasad BA, Pushpakumara DKNP, Ramana KVR, Vijayanand Tamarind, Tamarindus indica 2006 Southampton, UKSouthampton Centre for Underutilised Crops [Google Scholar]
[7]. Akajiaku LO, Nwosu JN, Onuegbu NC, Njoku NE, Egbeneke CO, Proximate, mineral and antinutrient composition of processed (soaked and roasted) tamarind (Tamarindus Indica) seed nutCurr Res Nutr Food Sci 2014 2(3):136-45. [Google Scholar]
[8]. Khan S, Chatra L, Prashanth SK, Veena KM, Rao PK, Pathogenesis of oral submucous fibrosisJ Cancer Res Ther 2012 8(2):199-203. [Google Scholar]