Endometrial polyp is a focal hyperplastic growth of endometrial glands and stroma and is benign lesion commonly, which can rarely become malignant. Abnormal Uterine Bleeding (AUB) is the commonest presentation in the reproductive age group as well as postmenopausal age group. Endometrial polyps especially at cornua can be attributed as a cause of infertility also. Sometimes patients will be entirely asymptomatic [1]. With the advent of high-resolution pelvic ultrasound and hysteroscopic diagnosis, it has become clear that AUB in women’s life is associated with endometrial polyp more often than suspected earlier. The prevalence of endometrial polyp ranges from 7.8% to 34.9% depending on the population studied [1].
With increasing use of transvaginal ultrasound as imaging modality in the outpatient clinic, endometrial polyps are diagnosed easily. It typically appears as a hyperechoic lesion, sometimes-cystic spaces within it. Colour Doppler may delineate the feeding vessel [2]. Saline infusion sonography improves the diagnostic accuracy. The improved diagnostic accuracy of polyp by various methods has led to the increased use of hysteroscopy that proves to be the best diagnostic and therapeutic approach. Diagnostic hysteroscopy and blind avulsion of the polyp had been widely practiced by many gynaecologists, though polypectomy by hysteroscopic micro scissors, grasping forceps and resectoscope has taken over now. The small polyps are favoured to be removed as office hysteroscopy-see and treat method. Larger polyps still are better managed by resectoscope. Recently hysteroscopic morcellation is available which cuts the bigger polyp into pieces and aspirates them, useful in myomatous polyps [3].
To study the clinical features of endometrial polyp and the safety and feasibility of blind polypectomy following diagnostic hysteroscopy.
Materials and Methods
This retrospective study was conducted in the obstetrics and gynaecology department at Amrita institute of medical sciences, during the period of January 2008 to December 2014. Total of 256 women who were diagnosed to have endometrial polyp by transvaginal ultrasound, underwent diagnostic hysteroscopy and blind polypectomy by simple avulsion were included in the study. Polyp was confirmed by histopathology. The clinical data was collected from the electronic medical records system.
Women diagnosed with endometrial polyp were posted for diagnostic hysteroscopy in the proliferative phase of menstrual cycle after necessary preoperative investigations and pre-anaesthetic check up. On the day of procedure, Misoprostol (Prostaglandin E1 analogue) 200 microgram was inserted vaginally for cervical preparation two hours prior to the procedure. After informed consent, they were taken up for procedure under short general anaesthesia. Internal os was dilated up to 6 hegars size. Standard rigid hysteroscope (Karl storz) with 5.5mm outer sheath was introduced to know the site and number of polyp. Then internal os was dilated up to 10 hegars dilator size. Small ovum forceps, sponge holding forceps or Kochers forceps was used for removal of polyp without vision. Prior hysteroscopy directed us to target the polyp. The re inspection of the uterine cavity was done by hysteroscope to know the completeness of the polypectomy. The remaining small pedicle was curetted out followed by check curettage. The specimen was sent for histopathology and analysed. The procedure was done as a day care procedure.
After the next cycle, they were followed up by transvaginal ultrasonography, thereafter annually. A total of 76 women were lost to follow-up.
Statistical Analysis
The data was analysed by SPSS software version11.0. Distribution, frequency, Chi square test were used for categorical variables and Students t-test was used for numerical variables.
Results
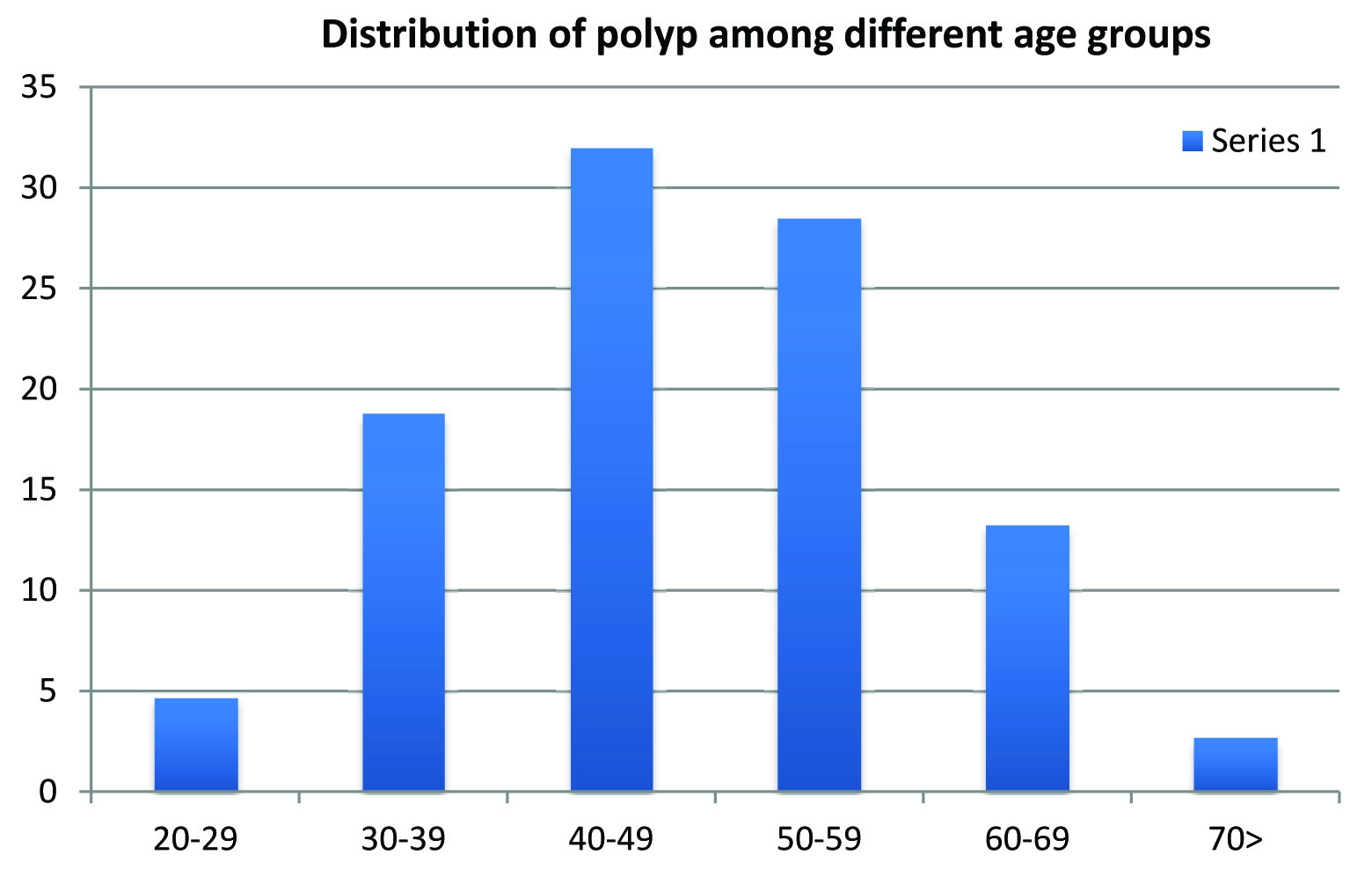
Mean age of the women with endometrial polyp in our study was 48.5+10.88 (range 29-76) [Table/Fig-1]. The prevalence of polyp was more common in the age group of 40-49 years 32% (82) women belonged to this group followed by 28.5% (73) in 50-59years group [Table/Fig-2]. Seven were above 70 years. Out of 256 women, 34.4% (88) were postmenopausal. Polyps manifested as AUB in 45.6% (117) of our study population. 4% women had the characteristic intermenstrual bleeding. A 47.7% (42) postmeopausal women were symptomatic with vaginal bleeding. In 16.8% (43) women, the polyp was diagnosed incidentally by ultrasonogram on routine check-up. Other women presented with vague complaints like lower abdominal pain, backache, vaginal discharge, pruritus vulva and hirsutism. In our study only 5.5% (8) patients had infertility as their main issue. Regarding the number of polyp, single polyp was present in 81.6% (209) of women whereas in 18.4% (47) had more than one polyp. The mean size of the polyp was not significantly different between premenopausal and postmenopausal women. Mean size of the polyp was almost same in single and multiple polyps-1.938±1.08 and 1.90±1.11 respectively (p-value=0.846) Prevalence of risk factors like diabetes, hypertension, size and number of polyps and distribution of polyp according to the site are described in [Table/Fig-1]. The complications associated with diagnostic hysteroscopy and polypectomy were very minimal in our study. One postmenopausal woman had perforation of uterine fundus during the procedure. She was admitted and managed conservatively with antibiotics. Next day she was discharged uneventfully. Another woman, who was having rheumatic heart disease with mitral and aortic valve stenosis, had postoperative pneumonia and treated with parenteral antibiotics and other supportive management. While analysing the associated gynaecological issues, 52% (133) women had concurrent problems such as adenomyosis, myoma uterus, dysfunctional uterine bleeding, ovarian cyst, polycystic ovarian disease and infertility.
Clinical factors of polyp among premenopausal and postmenopausal women.
| Premenopausal | Postmenopausal | p-value |
|---|
| Menopausal | 168(65.6%) | 88(34.4%) |
|---|
| Number of polypSingle Multiple(2 and above) | 14226 | 6721 | 0.100 |
| Sites-FundalAnteriorPosteriorLateralMultiple | 16(9.5%)44(26.2%)32(19%)53(31.5%)23(13.7%) | 2(2.3%)22(25%)21(23.9%)27(30.7%)16(18.2%) | |
| Mean size of the polyp in Cms | 1.823±0.99 | 2.141±1.21 | 0.025 |
| HypertensionYesNo | 13(7.7%)155(92.3%) | 33(37.5%)55(62.5%) | 0.000 |
| Diabetes mellitus YesNo | 8(4.8%)160(95.2%) | 31(35.2%)57(64.8%) | 0.000 |
| HypothyroidismYesNo | 19(11.3%)149(88.7%) | 6(6.8%)82(93.2%) | 0.250 |
| DyslipidemiaYesNo | 3(1.8%)165(98.2%) | 14(15.9%)74(84.1%) | 0.000 |
| HistopathologyBenignPremalignant and malignant lesions | 153(91.1%)15(8.9%) | 68(77.3%)20(22.7%) | 0.002 |
| RecurrenceYesNoHysterectomy | 5(4.5%)93(83.8%)13(11.7%) | 2(2.9%)49(71%)18(26.1%) | 0.044 |
Diagram showing the prevalance of endometrial polyp of different age groups
Histopathological study of the polyp showed two malignant polyps in our study population. Premalignant lesions i.e. endometrial hyperplasia without atypia and with atypia was found in 33 women. Another interesting finding is the presence of atypical polypoid adenomyoma in 2 women. Rest of the women had benign polyps.
On follow-up for few months to the maximum of six years, 76 women were lost to follow. Out of 180 women, 31 women had to undergo hysterectomy for various other reasons of premalignant and malignant lesions, adenomyosis, fibroid uterus, prolapse uterus and ovarian cyst. Seven persons had recurrence at varying intervals.
Discussion
Endometrial polyp is a common gynaecological condition, the prevalence of which increases with increasing age. In our study population, prevalence peaks were seen in the fourth decade followed by fifth decade of life. In a larger series study by E.Ricciardi et al., 79.8%women were below 60years of age [4]. AAGL practice report says that increasing age is the risk factor for the presentation of an endometrial polyp [5]. A total of 66% women in our study presented with AUB which is the commonest symptom for the endometrial polyp, similarly found in various other series. AUB due to endometrial polyp has been classified as AUB-P for premenopausal women endorsed by FIGO. In our study 47.7% postmenopausal women with polyp and 75.6% premenopausal women were symptomatic with abnormal uterine bleeding. In a study by Preutthipan et al., 76.3% premenopausal women, 20% postmenopausal women had AUB [6]. Prevalence of intermenstrual bleeding was 2.4%. Almost one third of the women had associated myoma uterus and adenomyosis.
Risk factors for the development of endometrial polyp are age, hypertension, obesity and tamoxifen use. In our study 18%women had associated hypertension and it was more in postmenopausal age group. Two women using tamoxifen had polyp in our study out of which one had recurrence of polyp after 3years which showed focal atypia for which she underwent hysterectomy.
Polyps were single in 81.6% and multiple in 18.4%. Multiple polyps were comparatively more in postmenopausal women. In a study by Hassa et al., 29.2%women had multiple polyps and he found that polyp number, site, size were not correlated with symptomatology which was supported by another study by Bulent et al., [7,8]. In our study mean size of the polyp was not statistically different between single and multiple polyps, premenopausal and postmenopausal women, benign and premalignant and malignant lesions. In a study by Preutthipan et al., mean size of the polyp was comparatively bigger in premenopausal women 3.4±0.9cm than postmenopausal women 2.5±0.8cm [6]. In our study it was 1.82±0.99 and 2.14±1.21 respectively. When the site of the polyp was analysed, lateral walls either right or left were the commoner locations followed by anterior and posterior walls. This may be attributable as one of the causes of infertility in women with polyp obstructing the tubal ostia. We had only 5.5% women presented with infertility.
Histopathological examination of the endometrial polyps showed 86.3% benign lesions. In a study by E. Ricciardi et al., 95.78% polyps out of 973 were benign. These polyps can exhibit the premalignant changes which can turn into malignancy in 0% to 12.9% of polyps in case series reported to date. E. Ricciardi’ series, 2.67% were premalignant and 1.54% was malignant [4]. In our study 12.9% were premalignant and 0.8% malignant. The prevalence of premalignant polyps was relatively higher in our series. Hysterectomy was performed in 2 women with atypical polypoidadenomyoma, which has the tendency for progression to malignancy. Atypical polypoid adenomyoma with complex glands the risk of myometrial invasion and they can coexist with other enomterial neoplasms [9,10].
Regarding the polypectomy, the surgical trend has moved from blind avulsion to diagnostic hysteroscopy and polypectomy under vision to outpatient hysteroscopic polypectomy now. AAGL guideline says that hysteroscopic polypectomy remains the gold standard treatment for polyp (Level B). There does not appear to be differences in clinical outcomes with different hysteroscopic polypectomy techniques (Level C). Hysteroscopic polypectomy using resectoscope, bipolar forceps, grasping forceps and microscissors are some of the techniques used. Each has its own merits and demerits [5].
There is good direct and circumstantial evidence that hysteroscopic resection of endometrial polyps under vision is safe simple and superior to blind techniques. The problems posed in the review of the management of endometrial polyps in the 21st century by Annan et al were that blind avulsion can miss out the malignancy [11]. But in our study, the prevalence of premalignant and malignant polyps is 13.7% which is comparable to other series. As per the hospital protocol, blind polypectomy was followed by check curettage and check hysteroscopy to ensure the completeness of the procedure. Blind avulsion needs excessive cervical dilatation which can lead to false tracks, uterine perforations etc., [11]. Prior cervical ripening with misoprostol, the prostaglandin E1 analogue minimized the lot of intraoperative complications like cervical tear, false tracks, uterine perforation etc. In our study we had one uterine perforation, one cervical tear, one false passage and one patient had mild bleeding after the procedure. Preutthipan et al., had higher incidence of complications (8.8%) -14 women in resectoscope group that included 9 cervical tears. The reasons cited were bigger size of the polyps, larger diameter of the resectoscope negotiating through smaller cervix [6]. In another study by Lienge et al., the complication rate was 7.8%-perforation being the common complication [12].
Not many studies have mentioned about the recurrence of endometrial polyp. In our study, in the mean follow-up period of 37.57±28.12 months, 3.9% (7 women) had recurrence. In the follow up period of 16.56±18.96 months, 78.9% women didn’t have recurrence. Preutthipan et al., claimed that there was 0% recurrence with resectoscopic method and 3.2% with other methods like microscissors, grasping forceps, electric probe [6]. In contrast to this study, Paradisi R et al., showed that in the follow up period of 26.3±19.7 months, the recurrence rate was 13.3% following resectoscopic method. But the hyperplastic polyps tend to recur more than benign ones [13]. Eight women with premalignant polyp didn’t have recurrence. Two women had recurrence of premalignant lesion of endometrium after 5months and 2 years period respectively. Nine women were lost to follow. The persons with recurrent endometrial polyp in our study had benign polyps and one with multiple polyps. Recurrence occurred from 7months to 6years period. Only one woman had the risk factor of tamoxifen exposure.
As the glycin was not used as distension medium in diagnostic hysteroscopy and blind polypectomy, the associated complications like fluid overload, electrolyte imbalance were avoided.
Limitation
Being a retrospective study, the inherent problem of data collection regarding follow up was there. So the exact incidence of recurrence of endometrial polyp after this procedure could not be found.
Conclusion
Endometrial polyp commonly occurs in fourth decade of life. Abnormal uterine bleeding is the most common presenting symptom. Prevalence of premalignant and malignant polyps is more common in postmenopausal women. As per our study diagnostic hysteroscopy and blind polypectomy has low complication rate and recurrence rate. It is technically feasible option in low resource setting for the practicing gynaecologists who has basic training in diagnostic hysteroscopy. With the recent advancements in operative hysteroscopic techniques, polypectomy under vision is the method of choice.