Effects of Preheated Composite on Micro leakage-An in-vitro Study
Joshua Ng Chor Yang1, James David Raj2, Herald Sherlin3
1 Student, Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Chennai, India.
2 Senior Lecturer, Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Chennai, India.
3 Reader, Department of Oral and Maxillofacial Pathology, Saveetha Dental College and Hospitals, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Joshua Ng Chor Yang, Boys Hostel, Saveetha Dental College and Hospitals, 162, Poonamallee Highroad Vellapanchavadi, Chennai, Tamilnadu, India.
E-mail: ryan.joshng@gmail.com
Introduction
Resin composites have been the pinnacle of direct esthetic restorations ever since its discovery. However, it comes with its own disadvantages. Post-operative sensitivity and marginal discoloration frequently occur due to polymerization shrinkage and micro leakage, which is the major cause of failure in resin composite restorations.
Aim
To evaluate the effects of preheated composite at different temperatures on microleakage.
Materials and Methods
A total of 60 extracted non-carious human premolars were collected and class 1 cavity (1.5x4x 3mm) was prepared in each and were randomly divided into three groups. Group 1 (n=20) was filled with microhybrid resin composite (Heraeus Charisma Smile) at room temperature. Group 2 (n=20) was filled with the same resin composite which was preheated to 50°C and Group 3 (n=20) was filled with resin composite preheated to 60°C. Teeth were subjected to a thermocycling regime (500X, 5 - 55°C), followed by a dye infiltration by immersing in basic fuschin for 24 hours. The tooth was sectioned longitudinally and the extent or absence of micro-leakage was determined by the amount of dye penetration along the resin composite-tooth interface using a confocal microscope.
Results
There was minor micro-leakage detected at the occlusal margin of the control tooth specimen. The sample with preheated composite restoration at 50°C showed an intact tooth-restoration interface with no micro leakage. However, the preheated composite at 60°C showed large amount of microleakage.
Conclusion
Under the current limitation of the study, preheated composite at 50°C showed the least micro-leakage.
Bonding, Class 1 restoration, Marginal integrity, Microhybrid composite
Introduction
Direct composite restorations are gaining an increased popularity over the conventional amalgam restorations due to esthetic demands and concerns regarding mercury in amalgam [1]. The clinical success of the composite restorations is very much dependent on its polymerization and degree of conversion. Highly viscous composites are very hard to adapt accurately to cavity preparations and may leave behind unwanted voids, hence, more flowable composites with less filler content were introduced. There are many factors which affect the viscosity of resin.
One of the greatest limitations of direct resin composite restoration is linked to its high polymerization shrinkage. During polymerization, it changes from a pre gel phase to a post gel phase. During the pre-gel stage, the reactive species can rearrange themselves without generating much internal and interfacial stresses to compensate for any volumetric shrinkage [2–4]. However, in the post gel stage the resin has partially set and can no longer undergo plastic deformation to compensate for any volumetric shrinkage. As a result, tensile stresses are generated at the resin tooth interface and causes pulling of the material away from the tooth surfaces [5,6].
C-factor, also known as configuration factor is the ratio of unbonded to bonded surface which affects the polymerization shrinkage of the restoration. During polymerization of resin composite, any volumetric shrinkage will be compensated by rearrangement or flow of the resin composite. Only free surfaces of a restoration are able to act as a reservoir for plastic deformation in the pre gel stage. Thus, if clinically the C-factor can be decreased, the polymerization shrinkage may be decreased as well.
Composites with less viscous consistency were introduced because it increases adaptation and decreases micro-leakage along the restoration tooth interface. Many attempts have been made including incorporating flowable composites, fiber inserts, or chemical and laser treatments of dentin [7–13]. Chairside warming of composite resins before photopolymerisation is seen to reduce viscosity and increase flowability by increasing the degree of conversion. When temperature increases, both the radical and monomer mobility increases resulting in a more highly cross-linked polymer network [14]. With this increase in conversion, mechanical and physical properties of the resin are also increased. Also, pre-heated composites have a better surface hardness and greater depth of cure [15,16]. A study by Bortolotto and Krejci showed that when temperature was raised from 5°C to 40°C, there is a significant increase in the Vickers Hardness at a curing depth of 0.5mm [17].
Aim
The aim of the study is to determine the effect of temperature on the degree of micro leakage in resin composite restorations.
Materials and Methods
The study was conducted in Saveetha Dental College, Chennai, India and was approved by the Scientific Review Board Committee. A total of 60 extracted non carious premolars, previously stored in hydrogen peroxide at room temperature were used. Class 1 preparations were made in each tooth in the central groove with a high-speed hand-piece with a #245 carbide bur (MANI, INC). The cavity was made with a pulpal floor depth of 1.5mm, 4mm mesiodistal width and 3mm width buccolingually. The specimens were randomly assigned to the three groups. Group 1 (n=20) were filled with composite at room temperature (37°C), Group 2 (n=20) were filled with preheated composite at 50°C and Group 3 (n=20) were filled with preheated composite at 60°C. All restorations were placed by a single operator. Tooth was etched with acid etchant (Eco-etch, Ivoclar Vivadent) for 15 seconds and rinsed with saline and air dried gently. Bonding agent (Te-Econom Bond, Ivoclar Vivadent) is applied using an applicator tip and light cured for 20 seconds. Micro hybrid resin composite (Heraeus Charisma® Smile) was then placed in increments of 1mm with a Teflon coated instrument using an oblique technique and light cured for 20 seconds. Occlusal adaptation of composite was done with a Teflon coated instrument and finished with a flame shaped finishing bur. Composite was placed as mentioned in those specimens subjected to the control group. The roots of the tooth specimens were sealed with Glass Ionomer Cement (Glass Ionomer Cement Type 2 Shofu) to prevent penetration of dye from the apical region. Restorations in the preheated resin composite treatment were placed using resin composite heated externally by a waterbath to a temperature of 50°C and 60°C.
Teeth were then subjected to thermocycling, according to the International Organization for Standardization standard 11405 for 500 cycles at 5°C-55°C with a 30sec dwell time. Dye infiltration with basic fuschin was used to examine the micro leakage between the resin composite-tooth interfaces. Specimens were painted with 2 coats of finger nail varnish, leaving a 1 mm margin around the cavity to prevent dye penetration from any other occlusal irregularities. Tooth was then placed in a solution of basic fuschin for 24 hours. After 24 hours, the tooth specimens were sectioned longitudinally, in a mesiodistal direction through the middle of the restoration using a diamond disc. The extent or absence of micro-leakage was determined by the amount of dye penetration along the resin composite-tooth interface visually with a confocal microscope.
Results
The statistical analysis was done using one way ANOVA [Table/Fig-1] to test for any significance. Comparison between Group 1 and Group 2 revealed statistical difference as well with the comparison between Group 1 and Group 3. There were significant differences between all groups as shown by the Post-hoc Tukey test [Table/Fig-2].
One way ANOVA to compare mean micro-leakage between the control Group 1 at 37°C with groups which received preheated treatment, Group 2(50°C) and Group 3(60°C).
| Group | N | Mean | Std. Dev | f-value | p-value |
|---|
| Group–1(37°C) | 20 | 109.20 | 3.139 | 4012.701 | <0.001 |
| Group–2(50°C) | 20 | 89.75 | 2.099 |
| Group–3(60°C) | 20 | 160.15 | 2.346 |
| Total | 60 | 119.70 | 30.041 |
Statistically Significant (p<0.05)
Tukey HSD Post Hoc tests showing pair wise comparison between the control Group 1 at 37°C with groups which received preheated treatment, Group 2(50°C) and Group 3(60°C).
| Group | N | Mean Difference | p-value |
|---|
| Group – 1 (37°C) | Group–2 (50°C) | 19.450 | <0.001 |
| Group–3(60°C) | 50.950 | <0.001 |
| Group – 2 (50°C) | Group–3 (60°C) | 70.400 | <0.001 |
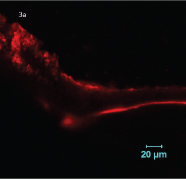
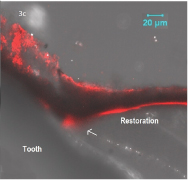
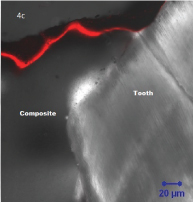
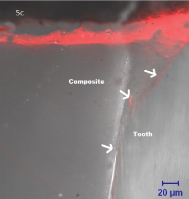
There was minor micro-leakage detected at the occlusal margin of the control tooth specimen [Table/Fig-3a,b,c]. The sample with pre-heated composite restoration at 50 °C showed an intact tooth-restoration interface with no micro leakage [Table/Fig-4a,b,c]. The preheated resin composite at 60 °C however showed large amount of micro leakage at the resin tooth interface [Table/Fig-5a,b,c].
Confocal fluorescence image of control group teeth without pre-heating resin composite (37°C) showing mild micro leakage.
Confocal phase contrast image of control group teeth without pre-heating composite (37°C) showing mild micro leakage.
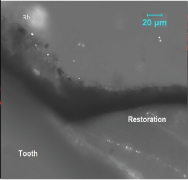
Confocal superimposed image of control group teeth without pre-heating resin composite (37°C) showing mild microleakage at the pointed arrow.
Confocal fluorescence image of sample pre-heated to 50 °C showing an intact restoration tooth interface with no micro leakage.

Confocal phase contrast image of sample pre-heated to 50 °C showing an intact restoration tooth interface with no micro leakage.
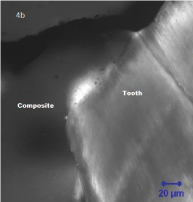
Confocal superimposed image of sample pre-heated to 50 °C showing an intact restoration tooth interface with no micro leakage.
Confocal fluorescence image of sample pre-heated to 60 °C showing the restoration tooth interface with microleakage.

onfocal phase contrast image of sample pre-heated to 60 °C showing the restoration tooth interface with micro leakage.
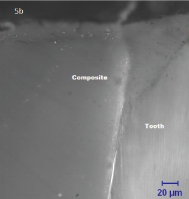
Confocal superimposed image of sample pre-heated to 60 °C showing the restoration tooth interface with micro leakage at the pointed arrows.
Discussion
The aim of this in vitro study was to evaluate the effects of preheated composite restorations on the marginal fit and micro leakage compared to restoring a cavity under normal physiological situations. Observation with confocal microscope was used as it is a non destructive technique which can clearly indicate leakage limits and eliminate stain spread due to specimen sectioning.
From the results of the study, preheated treatment at 50°C showed optimum restoration tooth interface with the least or no micro leakage compared to the preheated treatment at 60°C and the control sample. This was in accordance to a study done by Nivea Regina et al., in which pre-heated composite samples showed better marginal adaptation compared to those at room temperature [18]. This is due to better adaptation of the composite to the cavity walls as the viscosity of composite decreases when heated. Thermal vibrations causes the composite monomers to move further apart thus allowing them to glide alongside each other more readily [19]. This allows more effective wetting of the cavity walls.
The preheated sample to 60°C showed the greatest amount of micro-leakage contrary to the presumed results that the higher the temperature the better the marginal fit. This may be due to the likelihood of temperature drop between the heating process and filling and curing of the resin in the cavity. When the resin composite is cured, it has probably already reached a lower temperature where the enhanced mechanical properties due to increased temperature have diminished. As described by Daronch et al., a significant 50% of the temperature attained will be lost after 2 minutes and close to 90% after 5 minutes of composite removal from heating device [20]. In a study done by Wagner et al., delaying the curing of preheated composite after placement was also found to be counter productive as the drop in temperature of composite allowed the viscoelastic nature of the restoration to pull away from the walls of the tooth surface faster [21]. Due to the higher temperature it was heated to, the elastic deformation was even faster [21]. Another study also revealed that when resin composites are heated to temperatures of 54°C to 68°C, a significant increase in volumetric shrinkage is seen [22]. In the clinical practice, there are concerns regarding placing pre heated composite of higher temperature into cavities as it may cause thermal injury to the pulp. However, Daronch et al., found out that there was no significant difference between the preheated resin composites and resin composites that are not heated [23].
Limitation
One of the limitations of this study would be the size of the sample. It could be increased for a better result. Also, the method for pre heating composite could be better with a more standardized device. Also, this in vitro study was done using only one type of composite. More clinical studies should be carried out with other variant composites at different temperatures to give a more conclusive result.
Conclusion
In a clinical scenario, composites can be warmed to mimic flowable composites in achieving better adaptability to the cavity walls by reducing viscosity and thereby reducing micro leakage, without losing its mechanical properties as to a flowable composite which has lesser filler particles. With preheated composites, there is an ease of composite manipulation as it can be easily injected into a cavity without using hand instruments. However, it is advised to work at a quicker pace while using preheated composites so as to prevent dissipation of heat.
Statistically Significant (p<0.05)
[1]. Christensen G, Should resin-based composite dominate restorative dentistry today?The J Am Dent Assoc 2010 141(12):1490-93. [Google Scholar]
[2]. Ferracane JL, Mitchem JC, Relationship between composite contraction stress and leakage in class V cavitiesAm J Dent 2003 16(4):329-43. [Google Scholar]
[3]. Peutzfeldt A, Asmussen E, Determinants of in vitro gap formation of resin compositesJ Dent 2004 32(2):109-15. [Google Scholar]
[4]. Davidson C, De Gee A, Relaxation of polymerization contraction stresses by flow in dental compositesJ Dent Res 1984 63(2):146-48. [Google Scholar]
[5]. Hilton TJ, Can modern restorative procedures and materials reliably seal cavities? In vitro investigation. Part 1Am J Dent 2002 15(3):198-210. [Google Scholar]
[6]. Lopes GC, Baratieri LN, Monteiro S Jr, Vieira LC, Effect of posterior resin composite placement technique on the resin dentin interface formed in vivoQuintessence Int 2004 35(2):156-61. [Google Scholar]
[7]. Sadeghi M, Lynch C, The effect of flowable materials on the microleakage of class II composite restorations that extend apical to the cemento-enamel junctionOper Dent 2009 34(3):306-11. [Google Scholar]
[8]. Ozel E, Soyman M, Effect of fiber nets, application techniques and flowable composites on microleakage and the effect of fiber nets on polymerization shrinkage in class II MOD cavitiesOper Dent 2009 34(2):174-80. [Google Scholar]
[9]. Xie H, Zhang F, Wu Y, Chen C, Liu W, Dentine bond strength and microleakage of flowable composite, compomer and glass ionomer cementAust Dent J 2008 53(4):325-31. [Google Scholar]
[10]. Korkmaz Y, Ozel E, Attar N, Effect of flowable composite lining on microleakage and internal voids in class II composite restorationsJ Adhes Dent 2007 9(2):189-94. [Google Scholar]
[11]. Belli S, Orucoglu H, Yildirim C, Eskitascioglu G, The effect of fiber placement or flowable resin lining on microleakage in class II adhesive restorationsJ Adhes Dent 2007 9(2):175-181. [Google Scholar]
[12]. El-Mowafy O, El-Badrawy W, Eltanty A, Abbasi K, Habib N, Gingival microleakage of class II resin composite restorations with fiber insertsOper Dent 2007 32(3):298-305. [Google Scholar]
[13]. Siso HS, Kustarci A, Göktolga EG, Microleakage in resin composite restorations after antimicrobial pre-treatments: effect of KTP laser, chlorhexidine gluconate and clearfil protect bondOper Dent 2009 34(3):321-27. [Google Scholar]
[14]. Daronch M, Rueggeberg F, De Goes M, Giudici R, Polymerization kinetics of pre-heated compositeJDR 2006 85(1):38-43. [Google Scholar]
[15]. Lucey S, Lynch C, Ray N, Burke F, Hannigan A, Effect of pre-heating on the viscosity and microhardness of a resin compositeJ Oral Rehabil 2010 37(4):278-82. [Google Scholar]
[16]. Muñoz CA, Bond PR, Sy-Muñoz J, Tan D, Peterson J, Effect of pre-heating on depth of cure and surface hardness of light-polymerized resin compositesAmJ Dent 2008 21(4):215-22. [Google Scholar]
[17]. Bortolotto T, Krejci I, The effect of temperature on hardness of a light-curing compositeJDR 2003 82(Special Issue A):0119 [Google Scholar]
[18]. Fróes-Salgado N, Silva L, Kawano Y, Francci C, Reis A, Loguercio A, Composite pre-heating: effects on marginal adaptation, degree of conversion and mechanical propertiesDent Mater 2010 26(9):908 [Google Scholar]
[19]. Didron P, Chrzanowski W, Ellakwa A, Effect of temperatures on polymerization stress and microleakage of class V composite restorationsOJCM 2013 03(04):107-12. [Google Scholar]
[20]. Daronch M, Rueggeberg F, Moss L, De Goes M, Clinically relevant issues related to preheating compositesJ EsthetRestor Dent 2006 18:340-50. [Google Scholar]
[21]. Wagner W, Aksu M, Neme A, Linger J, Pink F, Walker S, Effect of pre-heating resin composite on restoration microleakageOper Dent 2008 33(1):72-78. [Google Scholar]
[22]. Walter R, Swift E, Sheikh H, Ferracane J, Effect of temperature on composite resin ShrinkageQuintessence Int 2009 40(10):843-47. [Google Scholar]
[23]. Daronch M, Rueggeberg F, Hall G, De Goes M, Effect of composite temperature on in vitro intrapulpal temperature riseDent Mater 2007 23(10):1283-88. [Google Scholar]