Sero-Negative Systemic Sclerosis: A Rare Presentation
Rakesh Chander1, Santokh Singh2, Siddhesh Arun Kalantri3, Shiv Charan4, Abhishek Gupta5
1 Assistant Professor, Department of Medicine, Government Medical College, Amritsar, India.
2 Principal and Head, Department of Medicine, Government Medical College, Amritsar, India.
3 Post Graduate Student, Department of Medicine, Government Medical College, Amritsar, India.
4 Associate Professor, Department of Medicine, Government Medical College, Amritsar, India.
5 Post Graduate Student, Department of Medicine, Government Medical College, Amritsar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Siddhesh Kalantri, Flat No 5C, Lee Residency, Lee Road, Opposite Shambunath Hospital, Kolkata-70020, India.
E-mail: sidkalantri@gmail.com
Systemic Sclerosis is a multisystem disease associated with progressive fibrosis of skin and internal organs. It is diagnosed by presence of characteristic clinical findings and is supported by specific serologic abnormalities. ANA is positive in case of systemic sclerosis in 90 percent of cases. We report a rare case of this rare disease where patient was ANA, Antitopoisomerase I (anti-Scl-70), Anticenteromere antibody negative.
Antinuclear antibody, Anticenteromere, Antitopoisomerase I
Case Report
A 62-year-old female presented to medical emergency with complaints of skin thickening and ulceration of legs and hands for last 3 months. This thickening was insidious in onset and started with involvement of both hands and feet. It progressed to involve face (patient complained of difficulty in opening mouth) and trunk. History of Raynauds phenomenon was present for last 3 months. Patient gave history of decreased urine output and bilateral pedal oedema, history of dyspnoea on exertion was present. Patient gave history of pain and swelling in wrist, elbow & knee joints. There was no history of dysphagia.
On examination patient was afebrile. BP was 90/60 mmhg, pulse rate was 104/min & respiratory rate was 24/min. Pallor, icterus, clubbing, cyanosis, lymphadenopathy was absent. Jugular venous pressure was not raised. Skin thickness was present [Table/Fig-1] extending upto the wrist joints, ankle joints, trunk and perioral region-microstomia [Table/Fig-2]. Skin over forearms and abdomen and behind ears showed salt and pepper pigmentation that is depigmentation with perifollicular retention of pigment [Table/Fig-3]. Patient had finger tip ulcerations [Table/Fig-4] with pitting scars. Rest of general examination was normal. On cardiovascular examination second heart sound was loud in pulmonary area. On respiratory system examination Velcro crepitations were audible in right infrascapular area and right axilla. Abdominal and neurological examination was normal. Patient’s total score (ACR/ EULAR score for systemic sclerosis) was 16 (greater than 9) – this was consistent with systemic sclerosis.
Skin thickening over dorsum of fingers and hand.

Perioral Furrowing, Pinched up nose.

Areas of hyper and hypopigmentation (salt and pepper).


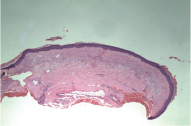
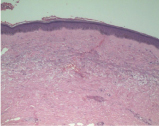
On laboratory evaluation Hb-11.6gm%, TLC-14400mm3, DLC-80% neutrophils, 18% lymphocytes, 1% eosinophils, 1% monocytes. Blood urea-134mg/dl, serum creatinine-5.9mg%, urine examination: protein++, ANA=2.88 (n< 20), Scl-70=2.96 (n< 20), Anti-centromere antibody=1.96(n<20), anti-U1 RNP antibody=0.79(n <5.0). Anti-RNA polymerase III antibody, anti-CCP antibody, RA factor were negative. X-ray chest showed area of fibrosis in right lower lobe. High resolution computed tomography [Table/Fig-5] was consistent with X-ray and there was no evidence of malignancy in chest. Evidence of PAH (Pulmonary Arterial Hypertension) was present on 2D echocardiography and there was evidence of mitral and tricuspid regurgitation. Serum protein electrophoresis did not show any monoclonal band. Skin Biopsy taken from dorsum of right forearm was consistent with systemic sclerosis. It showed marked thickening of collagen bundles in reticular and papillary dermis with hyalinised appearance. The upper reticular dermis showed telangiectasia and eccrine units appear to be present in thickened mid reticular dermis [Table/Fig-6,7].

HPE from right forearm 10x-Hyalanised appearance of dermis.
HPE from right forearm 40x-Thickening of collagen bundles with hyalanisation of papillary dermis.
Discussion
Systemic sclerosis is associated with positive ANA in 90% of cases [1]. In the EULAR Scleroderma Trials and Research (EUSTAR) database 5390 patients who fulfilled the American College of Rheumatology criteria for systemic sclerosis were enrolled and screened for the absence of ANA. In a study it was found that 92.3% cases were ANA positive, 30.4% cases were anti-centromere antibody positive and 36.4 were Scl-70 positive [2]. In another study of 3249 patients, it was noted that (6.4%) were ANA negative [3].
There are case reports where sero-negative systemic sclerosis is associated with malignancy but these patients were also negative for Raynauds phenomenon [4]. It has been found to be associated as paraneoplastic manifestation of secondary malignancies such as Multiple Myeloma or CA breast. Of the seven patients whose data was available in EUSTAR four patients had a malignancy: two had breast cancer, one had multiple myeloma with possible scleromyxoedema and one had bladder carcinoma [2]. SLE and dermatomyositis may present with similar manifestations but other criteria’s are not fulfilled in our case. Our patient did not fulfil any criteria for systemic sclerosis mimic and had no evidence of malignancy.
There are various differential diagnosis of scleroderma like skin thickening which need to be taken into consideration while evaluating patient:
Scleroderma – Usually internal organs not involved, associated with diabetes, prominent thickening of trunk. Can be associated with Myeloma or Monoclonal gammopathy of unknown significance. Biopsy will have increased mucin deposits. Our patient did not have ‘M’ band on electrophoresis and had interstitial Lung disease. Also the involvement was quite diffuse starting distally rather than proximal onset in Sclerederma [5].
Scleromyxoedema — Scleromyxoedema is characterized by yellow and waxy papules arranged in a linear fashion. When the papules coalesce, induration similar to sclerodermatous changes may be noted. This is also common with paraproteinemias [6].
Chronic graft versus host disease – But there was no previous history of Allogeneic Stem Cell Transplant.
Drug induced – Bleomycin and platinum based compounds can cause skin thickening, but there was no history of these drugs administration.
Eosinophilic fasciitis – Eosinophilic fasciitis (diffuse fasciitis with eosinophilia) leads to adherence of skin to underlying fascia. Changes are prominent proximal to the wrists and ankles and usually spare the hands and feet. Sparing of hands and feet is against our case [7].
Endocrine disorders – Diabetes mellitus and myxoedema can be associated with skin thickening. Can be associated with POEMS (Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal gammopathy and Skin changes) syndrome.
Nephrogenic systemic fibrosis – After administration of Gadolinium Contrast in severe renal failure patients, but there is no such history.
Since there can be many conditions which can mimic systemic sclerosis as discussed above, meticulous history taking, examination and thorough diagnostic evaluation is important before labelling patient as sero-negative systemic sclerosis.
Conclusion
Thorough clinical evaluation of patients is needed to rule out mimics of Systemic Sclerosis. This is a rare presentation of relatively rare disease where there was no evidence of underlying malignancy and patient had negative Anti-Nuclear Antibodies.
[1]. Kavanaugh A, Tomar R, Reveille J, Guidelines for clinical use of the antinuclear antibody test and tests for specific autoantibodies to nuclear antigens. American College of PathologistsArch Pathol Lab Med 2000 124:71 [Google Scholar]
[2]. Carreira PE, Derk CT, Deuschle K, Kay J, Morgiel E, Schneeberger D, Systemic sclerosis without antinuclear antibodies or Raynaud’s phenomenon: a multicentre study in the prospective EULAR Scleroderma Trials and Research (EUSTAR) databaseRheumatology (Oxford) 2013 52(3):560-67. [Google Scholar]
[3]. Salazar GA, Assassi S, Wigley F, Hummers L, Varga J, Hinchcliff M, Antinuclear antibody-negative systemic sclerosisSemin Arthritis Rheum 2015 44(6):680 [Google Scholar]
[4]. Chowdhury SU, Mahmud MI, Miah MA, Talukder SI, Islam MN, Islam N, Unusual presentation of progressive systemic sclerosisMymen singh Med J 2008 17:192-96. [Google Scholar]
[5]. Kövary PM, Vakilzadeh F, Macher E, Zaun H, Merk H, Goerz G, Monoclonal gammopathy in scleroedema. Observations in three casesArch Dermatol 1981 117:536 [Google Scholar]
[6]. Gabriel SE, Perry HO, Oleson GB, Bowles CA, Scleromyxoedema: a scleroderma-like disorder with systemic manifestationsMedicine (Baltimore) 1988 67:58 [Google Scholar]
[7]. Shulman LE, Diffuse fasciitis with eosinophilia: a new syndrome?Trans Assoc Am Physicians 1975 88:70 [Google Scholar]