Solitary Fibrous Tumour of the Clavicle: A Rare Case Report
Dileep Krishnamoorty Srinivas1, Arjun Ballal2, Mukta Pai3, Kushalappa Subbiah4, H. Ravindranath Rai5
1 Assistant Professor, Department of Orthopaedic Surgery, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
2 Registrar, Department of Orthopaedic Surgery, ARS Hospital, Tirupur, Tamil Nadu, India.
3 Professor, Department of Pathology, A.J Institute of Medical Sciences, Mangalore, Karnataka, India.
4 Postgraduate, Department of Orthopaedic Surgery, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
5 Professor and Head of the Department, Department of Orthopaedic Surgery, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arjun Ballal, Registrar, Department of Orthopaedic Surgery, ARS Hospital, 6/53, 6th Street, Thennampalyam Extension, Palladam Road Tirupur-641604, Tamil Nadu, India.
E-mail: 5arjunballal@gmail.com
A Solitary Fibrous Tumour (SFT) is the preferred term by most of the pathologists than “haemangiopericytoma”. SFT is a heterogeneous group of benign and malignant neoplasms along a morphologic continuum. Here we report a case of SFT of the clavicle in a 26-year-old male patient, who presented to us with complaints of pain and swelling over the dominant shoulder. No signs of metastasis were noted clinically and radiologically. He underwent surgical resection of swelling. At 6 months after resection and after 22 cycles of radiotherapy, he was noted to have excellent prognosis with satisfactory shoulder function.
BCl2, Expansile tumour, Lytic lesion, Oxford score, Satellite nodules
Case Report
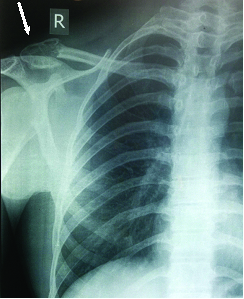
A 26-year-old gentleman reported to the out- patient department with complaints of pain and swelling over the right shoulder [Table/Fig-1] for 4 months. No history of any preceeding trauma, fever, weight loss or loss of appetite was noted. There was no history suggestive of tuberculosis or any other systemic illness. Clinical examination revealed a well-defined solitary swelling, fixed to the bone with a smooth surface and bony hard consistency, noted over the lateral end of the right clavicle. There were no palpable regional lymph nodes or organomegaly.
Swelling measuring approximately 4X3 cm over the right clavicle (The red circle encircling the mass and the arrow pointing the mass).

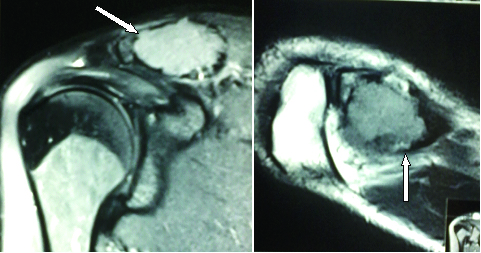
Radiographs revealed an expansile lytic lesion over the lateral end of the clavicle [Table/Fig-2]. Magnetic resonance imaging showed an expansile lytic lesion with altered signal intensity [Table/Fig-3,4].
Radiograph of the right clavicle anteroposterior view showing an expansile lytic lesion over the lateral end of the clavicle.
MRI Images showing an expasile lytic lesion over the lateral end of the right clavicle in the coronal and axial plane.
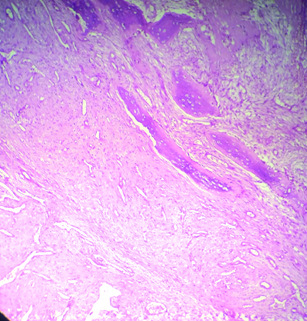
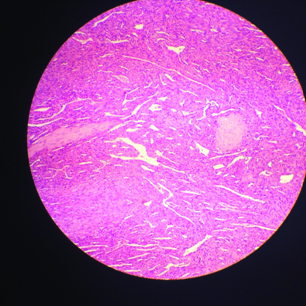
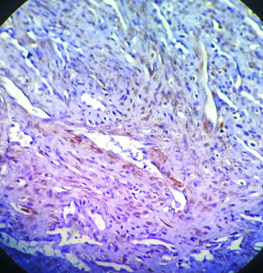
A complete haematological work up was made and the patient was taken up for a radical resection of the lateral end of the clavicle. An anterior approach to the clavicle was done and intraoperatively: a highly vascular expansile tumour, grayish white in colour, confined to the lateral 2 cm of the clavicle was noted. A wide resection of the tumour with one cm resection of the normal soft tissue was done. Post resection the tumour measured to a rough of 2.5 cm [Table/Fig-5]. No signs of local invasion of the tumour were noted. After resection of the lateral end of the clavicle, the coracoclavicular ligament was sutured to the clavicle by making a drill hole through the clavicle. Postoperatively, the patient was started on aggressive shoulder rehabilitation exercises from postoperative day two. Histopathologically; oval to spindle shaped cells were noted with surrounding thin branching vascular spaces infiltratrating the bony trabeculae [Table/Fig-6]. Staghorn vascular pattern was noted [Table/Fig-7]. The immohistochemistry marker BCl2 was diffusely positive [Table/Fig-8]. A diagnosis of solitary fibrous tumour of the clavicle was reported. Patient was referred to a medical oncologist at our hospital and 22 cycles of radiotherapy was instituted and was discharged. He was reviewed on a monthly basis and with asessement of shoulder function and serial radiographs were taken during each review. At 6 months the patient was noted to have full range of shoulder motion [Table/Fig-9a-c] with an ‘Oxford shoulder score’ of 42, which was indicative of satisfactory shoulder function and no signs of metastasis was detected.
Macroscopic: Tumour after resection.

Oval to spindle shaped cells surrounding thin branching vascular spaces infiltrating the bony trabeculae. (H&E x200).
Solitary fibrous tumour with staghorn blood vessels (40X).
BCl2 IHC marker diffusely positive in the tumour cells.
Images showing full range of right shoulder:
a) Abduction
b) External rotation
c) Internal rotation

Discussion
The usage of the term Haemangiopericytoma is now unpopular and has been replaced by Solitary fibrous tumour (SFT), as haemangiopericytoma is considered to be more of a histological pattern seen in different tumours and not a definitive clinical entity [1].
According to the report by Verbeke SL et al., reclassification of haemangiopericytomas of the bone as primary SFT was done [2].
There is a continuing debate as to which term is better to describe tumours. Although haemangiopericytoma is now being described mostly for meningeal and sinonasal tumours. Subtle differences between the two are described in standard textbooks on Soft tissue pathology (Enzinger). They are also described by some authors collectively as Haemangiopericytoma/Solitary Fibrous tumour [1].
Since CD 34 is positive in this case, it ruled out other tumours with ‘haemangiopericytoma/SFT’ like pattern [2,3]. SFT apparently produces more CD34 positivity than hamangiopericytoma [4].
Stout and Murray reported tumours with branching vessels surrounded by pericytic tumour cells [5,6]. These tumours were later termed as haemangiopericytomas and are now considered a cellular variant of SFT [7]. The SFTs are reported to have a glistening surface [8]. Most of them are composed to uniform collagen-forming spindle cells, arranged in interlacing fascicles. They may show associated myxoid changes, necrosis and rarely calcifications. They stain all cases with antibodies vimentin and CD34. They are sometimes referred to have a ‘patternless pattern’ [9].
The treatment of SFT of the bone is primarily surgical. Initial radical resection is mandatory to avoid recurrence. An appropriate surgical plan associated with a previous study of tumour vascular architecture is indicated in certain literature. Radiation therapy has usually been reserved for unresectable and recurrent tumours or for palliative care [10].
Enzinger and Smith observed the importance of tumour size concerning prognosis [11]. In tumours<6.5 cm, survival in 10 years reached 95% and 63% for larger tumours. They also noted that more than two-thirds of the cases that eventually metastasize develop local recurrences first [11]. The lung is the most common site of metastasis [12].
Lin Y J et al., reported a case in the axis bone and concluded that surgical excision and post operative radiotherapy was the main mode of management in the bone [13]. Sare Sipal et al., published a report of a case in the parietal bone in which no recurrence of the tumor or any metastasis was noted after nine months of excision [12]. Sahin Akhyar et al., described a patient with primary tumour in the tibia and concluded surgical excision had favourable prognosis for the tumour [14]. Enrique Palacios et al., published a set of seven cases and concluded that five of his cases had no recurrence of the tumor or complications after resection [15].
Conclusion
The intraosseus presentation of a primary solitary fibrous tumour of the lateral end of the clavicle is a rare occurrence and early detection with surgical resection with postoperative radiotherapy has favourable functional outcome with no signs of recurrence at 6months of follow-up.
[1]. Penel N, Amela EY, Decanter G, Robin YM, Berard PM, Solitary fibrous tumours and so-called hemangiopericytoma. review articleSarcoma 2012 2012:6902516 pages [Google Scholar]
[2]. Verbeke SL, Fletcher CD, Alberghini M, Daugaard S, Flanagan AM, Parratt T, A reappraisal of hemangiopericytoma of bone; analysis of cases reclassified as synovial sarcoma and solitary fibrous tumour of boneAm J Surg Pathol 2010 34(6):777-83. [Google Scholar]
[3]. Warraich I, Dunn DM, Oliver JW, Solitary fibrous tumour of the orbit with epithelioid featuresArch Pathol Lab Med 2006 130(7):1039-41. [Google Scholar]
[4]. Marchevsky AM, Varshney D, Fuller C, Mediastinal epithelioid solitary fibrous tumourArch Pathol Lab Med 2003 127(4):e212-15. [Google Scholar]
[5]. Stout AP, Murray MR, Hemangiopericytoma: a vascular tumour featuring Zimmermann’s pericytesAnn Surg 1942 116:26-33. [Google Scholar]
[6]. Stout AP, Hemangiopericytoma; a study of 25 casesCancer 1949 2:1027-54. [Google Scholar]
[7]. Gengler C, Guillou L, Solitary fibrous tumour and haemangiopericytoma: evolution of a conceptHistopathology 2006 48:63-74. [Google Scholar]
[8]. Magdeleinat P, Alifano M, Petino A, Solitary fibrous tumours of the pleura: clinical characteristics, surgical treatment and outcomeEuropean Journal of Cardio-Thoracic Surgery 2002 21(6):1087-93. [Google Scholar]
[9]. McMaster MJ, Soule EH, Ivins JC, Haemangiopericytoma: a clinico-pathological study and long term follow-up of 60 patientsCancer 1975 36(6):2232-44. [Google Scholar]
[10]. Mira JG, Chu FC, Fortner JG, The role of radiotherapy in the management of malignant hemangiopericytoma: Report of eleven new cases and review of the literatureCancer 1977 39:1254-59. [Google Scholar]
[11]. Enzinger FM, Smith BH, Hemangiopericytoma: An analysis of 106 casesHum Pathol 1976 7:61-82. [Google Scholar]
[12]. Sipal S, Demirci E, Calık M, Gundogdu B, Sengul G, Gundogdu C, Primary Hemangiopericytoma of the Parietal Bone: A Case ReportThe Eurasian Journal of Medicine 2009 41:205-07. [Google Scholar]
[13]. Lin YJ, Tu YK, Lin SM, Shun CT, Primary hemangiopericytoma in the axis bone: case report and review of literatureNeurosurgery 1996 39(2):397-400. [Google Scholar]
[14]. Sahin-Akyar G, Fitoz S, Akpolat I, Saglik Y, Erekul S, Primary hemangiopericytoma of bone located in the tibiaSkeletal Radiol 1997 26(1):47-50. [Google Scholar]
[15]. Enrique P, Santiago R, Luciano M, Lorusso Giovanni D, Rafael R, Sinonasal hemangiopericytomas: Clinicopathologic and imaging FindingsENT-Ear, Nose & Throat Journal 2005 :99-102. [Google Scholar]