Myocarditis is a potentially life threatening inflammatory disorder of the myocardium. About half of the cases of dilated cardiomyopathy in children are due to myocarditis [1]. Since children with myocarditis may be asymptomatic, true incidence is unknown [2]. Because the mortality rates for infants and children with myocarditis may be as high as 75% and 25%, respectively [3], early initiation of therapy is potentially beneficial and prompt diagnosis is imperative [4].
Presentation in acute myocarditis in children varies from mild flu like Illness to a fatal fulminent form. In many instances, the clinical course in acute myocarditis is monophasic with spontaneous recovery after several days of congestive heart failure [5]. On the other hand, some patients rapidly progress into cardiogenic shock before or after hospitalisation [5]. Ventricular arrhythmias, cardiogenic shock or cardiac arrest, are serious complications, during acute phase appearing unexpectedly [6]. Some patients may progress into subacute or chronic forms, with death as the final outcome [6]. Studies related to the mechanisms pertaining to the medley range of clinical manifestation of acute myocarditis have not been fully illuminated and clarified.
Furthermore, the predictors of the mortality in acute myocarditis have not yet been established. In the present study, we examined hemodynamic variables, cardiac biomarkers and echocardiographic findings at admission in patients with suspected myocarditis and their impact on mortality.
Materials and Methods
This was an observational study which enrolled children who presented with the fever of acute onset (less than 15 days in duration), and were diagnosed as suspected myocarditis on the basis of clinical features, Troponin I and echocardiography [7] in Paediatric ward at our institute over a period from August 2014 to December 2015. Children with known cardiac lesions, congenital or acquired, presenting with heart failure were excluded. On admission, children were subjected to detailed history and clinical examination.
Complete blood count, erythrocyte sedimentation rate, C-reactive protein was done in all children. Chest X-ray, cardiac enzymes: Troponin I, BNP (brain natriuretic peptide) and CPK-MB (creatinine phosphokinase) (The Alere Triage® Cardio3 Panel) were done at admission. Detailed echocardiographic examination including M-mode, 2-dimensional, and colour doppler echocardiography with colour-coding character was done in all patients. Echocardiograms were performed in the supine position and left lateral position with the right shoulder slightly raised, using modern digital echocardiographic equipment (Toshiba SSA 380 Power-Vision, Tokyo, Japan). We followed recommendations for standardising measurements made from M mode echocardiograms [8,9]. Centile charts (3rd, 10th, 25th, 50th, 75th, 90th, and 97th centiles) were constructed for each measurement in relation to body surface area [10].
All patients were treated similarly with IV fluids, decongestive therapy and vasopressors when needed. Assessment of the degree of respiratory distress and need for respiratory support (oxygen or Mechanical Ventilation (MV)); assessment of cardiac decompensation and need for cardiac support (inotropes or anti failure drugs) was done.
Patients who expired were compared with those who survived in terms of clinical features, cardiac markers and echocardiography findings.
Statistical Analysis
All statistical analysis was done using graphpad Prism 5 and SPSS statistical software. A Fisher exact p-value <0.05 was regarded as significant.
Results
Seventy patients were diagnosed as suspected myocarditis according to expanded criteria. Eight patients were excluded from the study. Six patients out of eight left against medical advice and could not be followed and two patients were of rheumatic heart disease. So total of 62 patients of suspected myocarditis were observed for this study.
Baseline characteristics of patients with suspected myocarditis.
| Parameters | n =62 (%) |
|---|
| Age, mean (SD) | 6.36 (3.48)* |
| Male female ratio | 1.2:1 |
| NYHA functional class |
| I | 6 (9.6) |
| II | 17 (27.4) |
| III | 25 (40.3) |
| IV | 14 (22.5) |
| Hypotension | 29 (46.77) |
| Troponin I > 0.02 ng/l, n (%) | 17 (27.4) |
| Troponin I, mean (SD) | 0.189 (0.997)* |
| CPKMB > 4.3 U/L, n(%) | 30 (48.38) |
| CPK-MB, mean (SD) | 6.46 (8.29)* |
| BNP >100 U/L,n(%) | 32 (51.61) |
| BNP, mean (SD) | 124.27 (127.44)* |
| LV ejection fraction %, mean (SD) | 45.66 (8.76)* |
| OUTCOME |
| Mortality | 11 (17.74) |
| Duration of hospital stay (days), mean (SD) | 6.7 (3.39)* |
| Need for ionotropes | 29 (46.77) |
| Need for ventilation | 9 (14.51) |
NYHA – New York heart association, BNP – brain natriuretic peptide, CPK-MB- creatinine phosphokinase, EF – ejection fraction, * mean(SD)
Mean age of presentation of suspected myocarditis was 6.36 ± 3.48 years with male: female ratio of 1.2:1. Troponin I was increased in 27.4% (n=17) of patients with mean Troponin I of 0.189 ± 0.997 ng/ml. CPK-MB was raised in 48.38 % (n=30) of patients with mean value of 6.46 ± 8.29 ng/ml and lastly BNP was raised in 51.61% (n=32) patients with mean value of 124.27 ± 127.44 pg/ml. Mean ejection fraction in patients was 45.66 ± 8.76. Considering their outcome, mortality in patients of suspected myocarditis was 17.74% (n=11). Duration of hospital stay was 6.7±3.39 days in patients of myocarditis, 14.51% (n=9) patients needed mechanical ventilation and 46.77% (n=29) patients of myocarditis needed ionotropes.
Epidemiological and Clinical Difference between Survivors and Non-survivors
There was no statistically significant difference in survivors and non survivors in terms of age, sex, duration of fever, chest pain, palpitation, swelling of body and features of heart failure. But NYHA class IV dyspnea (p=0.0115) and hypotension (p=0.0174) were significantly more in patients who did not survive [Table/Fig-2].
Clinical features in patients with myocarditis at admission.
| Clinical features | Survivors n=51 (%) | Non-survivors n=11 (%) | p-value † |
|---|
| Age, mean(SD) | 6.31 (3.48)* | 6.6 (3.49)* | 0.803 |
| Males | 26 (50.98) | 8 (72.72) | 0.317 |
| NYHA functional class IV | 6 (11.76) | 6 (54.54) | 0.0115 |
| Fever duration, mean (SD) | 6.54 (2.91)* | 5.63 (3.03)* | 0.354 |
| Hypotension | 20 (39.21) | 9 (81.88) | 0.0174 |
| Chest pain | 15 (29.41) | 3(27.27) | 1 |
| Palpitation | 24 (47.05) | 4 (36.36) | 0.7399 |
| Swelling of body | 29 (56.86) | 5 (45.45) | 0.3198 |
| Signs of CHF | 12 (23.5) | 4 (36.36) | 0.4668 |
CHF-congestive heart failure,
* Mean (SD)
† p<0.05 is significant.
Cardiac Markers in Survivor and Non-survivor Group
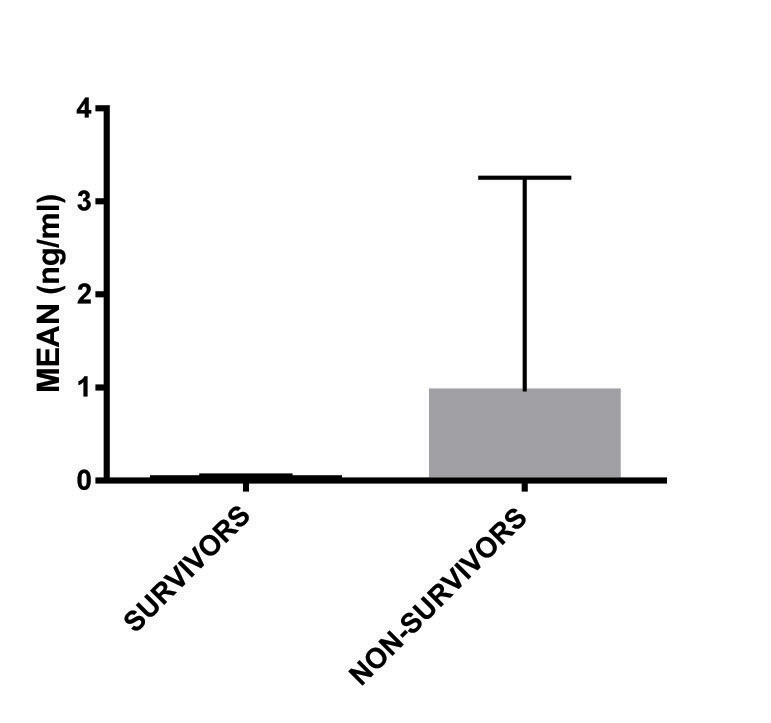
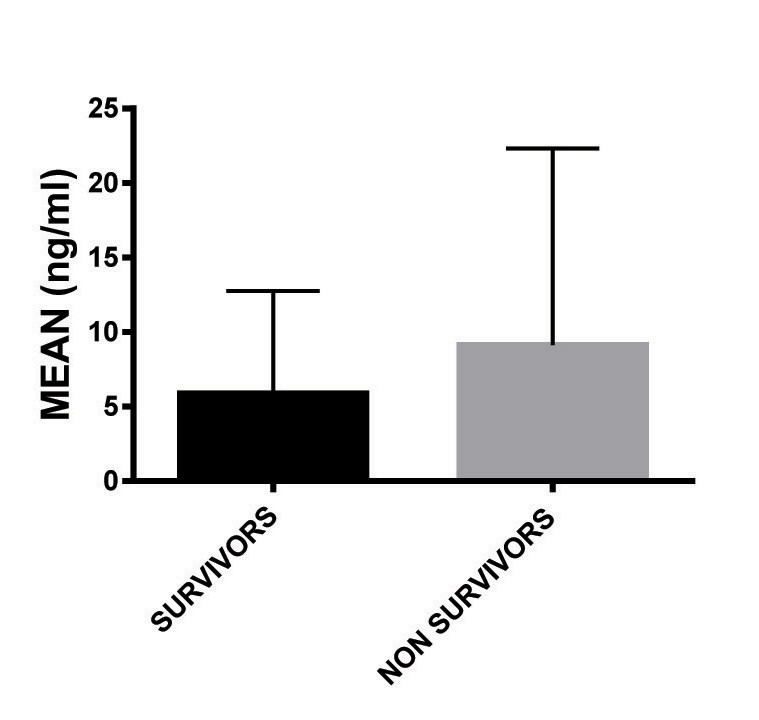
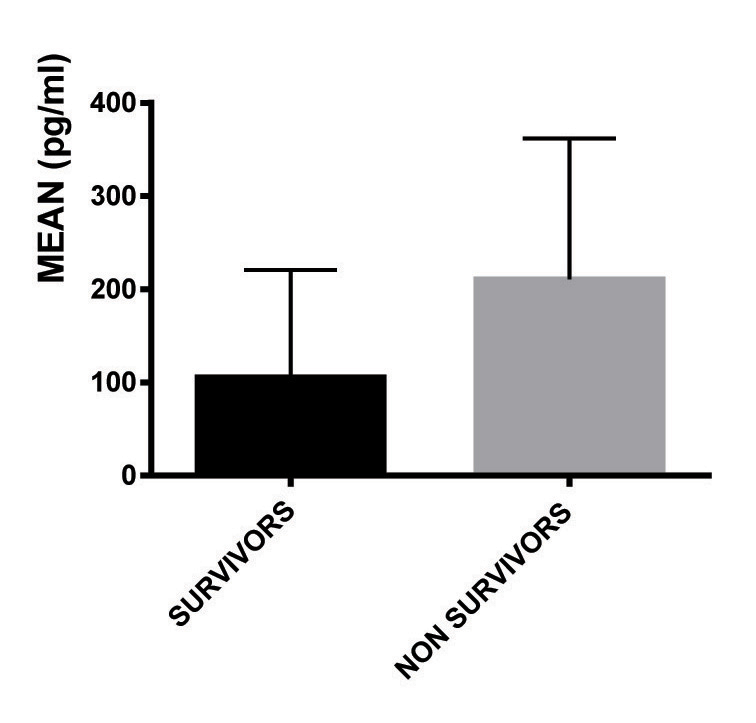
Mean value of CPK-MB was more in patients who died (9.1±9.04), but it was not significant. Similarly there was no significant difference in the number of patients whose CPK-MB was increased. Although, Troponin I was found to be raised in both survivors (23.52%) and non survivors (45.45%) with no significant difference, the mean value was significantly more in the non-survivor group (0.958 ± 1.13ng/ml); (p=0.0074). More number of patients who died had BNP levels increased in their plasma (p=0.0087) with higher mean value (p=0.0175). [Table/Fig-3,4ab,c].
Cardiac biomarkers in patients with suspected myocarditis at admission.
| Cardiac markers | survivors n=51 (%) | non survivors, n=11 (%) | p-value † |
|---|
| Troponin I > 0.02ng/l, n (%) | 12 (23.52) | 5 (45.45) | 0.1553 |
| Troponin I, mean (SD) | 0.023 (0.99)* | 0.958 (1.13)* | 0.0074 |
| CPKMB > 4.3 u/l, n (%) | 23 (45.09) | 7 (63.63) | 0.1816 |
| CPK-MB, mean (SD) | 5.88 (8.29)* | 9.1 (9.04)* | 0.2544 |
| BNP >100 U/L, n (%) | 24 (47.05) | 8 (72.72) | 0.0087 |
| BNP, mean (SD) | 105.66 (127.44)* | 210.58 (137.2)* | 0.0175 |
CPK MB – creatinine phosphokinase – MB, BNP- brain natriuretic peptide
* Mean (SD)
† p<0.05 is significant.
Troponin I in patients myocarditis.
CPK-MB in patients of myocarditis.
BNP in patients of myocarditis.
Echocardiography in Survivor and Non-survivor Group
LV ejection fraction was decreased more in non survivor group with mean value of 37±8.09% as compared to survivor group with mean value of 46.6±10.5%, (p=0.006) [Table/Fig-4d,5]. Rest all parameters of echocardiography were abnormal equally in both the groups [Table/Fig-5].
Ejection fraction in patients of myocarditis.

Echocardiography finding in patients with myocarditis at admission.
| Echocardiographic findings | Survivors n=51(%) | Non-survivors n=11(%) | p-value † |
|---|
| LV ejection fraction, %, mean (SD) | 46.6 (10.5)* | 37 (8.09)* | 0.006 |
| Cardiac dilatation | 3 (5.88) | 2 (18.18) | 0.2121 |
| Regional wall motion abnormalities | 22 (43.13) | 4 (36.36) | 0.7479 |
| Regional cardiac hypertrophy | 10 (19.60) | 4 (36.36) | 0.2493 |
* Mean, (SD)
† p<0.05 is significant.
On multivariate logistic regression analysis, NYHA IV dyspnea (p=0.0113, log odds=15.53), BNP (p=0.015, log odds=1) and ejection fraction (p=0.0284, log odds=0.9046) independently were the predictors of mortality in our study group [Table/Fig-6].
Multivariate logistic regression analysis of predictors of mortality.
| parameters | logistic coefficient | log odds | t value* | p-value* |
|---|
| Nyha IV | 2.7 | 15.53 | 2.53 | 0.0113 |
| Echo - EF† | 1 | 0.9046 | 2.19 | 0.0284 |
| BNP | 0.0081 | 1 | 2.43 | 0.015 |
| Hypotension | 1.6 | 4.9 | 1.46 | 0.1453 |
The above table shows that for each unit increase in NYHA-IV dyspnea, the chance of mortality increases by 15.53 times, for each unit decrease in ECHO-EF, the chance of mortality increases to 0.9 and for each unit change in BNP-value, there is equal change in the chances of cardiac death.
*p-values<0.05 imply statistical significance along with t-values greater than 2.
† ejection fraction
Discussion
Mean age of presentation of myocarditis patients was somewhat similar to Soongswang et al., study where mean age was 5.4±5.1 years [11]. Male: female ratio is 1.2:1. A slight male predominance is noted in this study. It is more common in men due to cardioprotective effects of hormones in women [12].
The aim of the present study was to determine whether clinical features, any cardiac marker or echocardiographic findings at the time of admission are able to prognosticate the lethal outcomes in patients with acute myocarditis.
We observed that among the clinical markers, NYHA functional class IV and hypotension were able to predict mortality in myocarditis in children. These parameters imply that the patients who died were already in the condition of cardiogenic shock and congestive heart failure at the time of admission to the hospital. Intensive care should start when patients show symptoms of hypotension. Similarly, Hsiao HJ et al., also found hypotension to be the predictor of mortality in myocarditis in children [13]. Advanced heart failure symptoms (NYHA classes III or IV) have also been reported previously to predict a poorer prognosis [14].
Biomarkers have become an increasingly important clinical tool for assessing cardiovascular disease and progression to heart failure. Biomarkers are used in early detection of sub-clinical disease, diagnosis, risk stratification, monitoring disease state, and to determine therapies [15]. Many biomarkers are also risk factors directly involved in the pathogenesis of disease.
In our study cardiac markers, Troponin I, CPK-MB and BNP were elevated in large number of patients at admission (27.4 %, 48.38% and 51.61% respectively). We have found that Troponin I and CPK-MB at admission were not able to predict mortality in suspected myocarditis patients. But mean value of Troponin I was higher in the non-survivor group. So it can be said that, higher Troponin I level is associated with the worst outcome. Cardiac biomarkers are elevated in about one-third of patients with acute myocarditis [16,17] and are of help in making the clinical diagnosis [18]. Elevation of cardiac Troponin I is more common than creatine kinase MB as seen from available clinical and experimental data [17]. Troponin I has limited sensitivity (34%) in the setting of acute myocarditis [19]. Cardiac markers elevate in acute myocarditis in proportion to the myocardial damage, i.e., less in focal compared to diffuse form [20] and more in fulminant than in non-fulminant cases [21]. For the same reason the degree of cardiac enzyme elevation is less in the initial stages of the disease and worsens during the clinical course with greater myocardial tissue necrosis. Therefore, the initial CPK-MB or Troponin I levels could not predict the disease course of the patients with acute myocarditis, but their higher levels at admission is probably associated with diffuse myocardial damage and worst outcome as seen in or study in case of Troponin I.
In our study higher levels of BNP were related to higher mortality. In contrast to cardiac troponins that are released due to cell wall compromise, BNP is synthesized in healthy cardiac myocytes from its precursor NT-pro-BN [22,23]. Many literature reveal BNP to be elevated in serum of patients with myocarditis or DCM and in animal models of myocarditis [24–28]. Several studies have proclaimed an association of higher levels of circulating BNP with the diagnosis of heart failure and fatal outcome [25,29]. As a predictor of death BNP levels are better than endothelin-1 or norepinephrine [22]. Although, several studies have found that NT-pro-BNP was better than BNP for predicting death or re-hospitalization for heart failure, probably due to the longer half-life of NT-pro-BNP in sera [30,31], Anand IS et al., had revealed the prognostic role of BNP for an unfavourable outcome in patients with heart failure or asymptomatic left ventricular dysfunction [32]. Noncardiac conditions that increase plasma BNP levels such as age, race, obesity and renal dysfunction should be taken into consideration when using this biomarker. Altogether, BNP and NT-pro-BNP are biomarkers with a high sensitivity and specificity in predicting heart failure in a number of conditions including myocarditis and DCM.
In our study no echocardiographic feature except ejection fraction at admission predicted mortality on bivariate analysis (p=0.006) and multivariate analysis (p=0.0284). Earlier Schultz et al., had conveyed that the prognosis for patients with acute myocarditis depends on ejection fraction (EF), clinical presentation and pulmonary artery pressure [33]. In a series of biopsy-proven lymphocytic myocarditis cases, Magnani et al., used a multivariate predictive model and identified presentation with syncope, bundle branch block, or an EF <40% as significant predictors of increased risk of death or transplantation [34].
Our study has certain limitations. As our primary objective was to know the risk factors associated with poor outcomes, considering feasibility of data collection in limited time period, we have taken consecutive samples and no formal sample size calculation was done. Also we had not done endomyocardial biopsy to diagnose myocarditis which is the gold standard test [35] due to non availability of expertise in our institution. Another concern is that we had not done follow-up of our patients to deduce the long term outcome of our patients who survived.
Conclusion
Children with myocarditis with Hypotension and having Troponin I and BNP markedly raised in their plasma with decreased ejection fraction should be aggressively treated in the intensive care unit as they are more prone to die. NYHA IV dyspnea, higher levels of BNP and decreased ejection fraction are independently related to worst outcome. This could help clinicians to understand the course of disease. These data support the necessity for future large longitudinal follow-up studies to definitely establish the predictor of cardiac death in patients of paediatric myocarditis, as well as to evaluate the factors that could lead to development of dilated cardiomyopathy in children.