Basal Cell Carcinoma (BCC) is the most common skin tumour constituting about 70% of all skin malignancies. Currently, there is no clear data regarding the prevalence of this tumour in India. It has been rarely studied before in South India [1]. Our aim was to analyse the occurrence of this tumour in the population of Southern Karnataka.
BCC was believed to arise from keratinocytes. There is recent evidence that these cells are derived from immature pluripotent cells of interfollicular epidermis and those present in the outer sheath of the hair follicle [2,3]. Recognition of mutations in PTCH1 has spurred genetic analysis of BCCs. All BCCs, whether sporadic or syndromic, have abnormalities of Hedgehog signaling pathway. This pathway is inhibited by a PTCH1 encoded protein [4,5].
The clinical appearance of BCC can be fairly inconstant. They are clinically divided into five types: nodular-ulcerative, pigmented, sclerodermiform or fibrosing, superficial and fibroepithelioma. It is locally invasive and seldom metastasises. Early diagnosis followed by surgical excision offers complete cure [6].
There is significant difference in the morphology of the BCCs, and therefore, many microscopic subtypes have been described. The microscopic subtypes comprise solid (nodular), micronodular, infiltrating, superficial, fibroepithelial, basosquamous (metatypical), keratotic, basal cell carcinoma with adnexal differentiation, and other variants [1,4]. As of now, histological pattern is one of the few major proven predictors of clinical behaviour of BCC. This study helps to analyse the variants of BCC in this part of the country and hence, the biologic behaviour of this common skin tumour here.
This study was aimed to evaluate the spectrum of basal cell carcinoma in southern Karnataka. The objectives were to analyse clinical data with respect to age, sex, site and size of the lesion, to observe the uncommon entities encountered and to study the concordance between clinical and histological diagnosis.
Materials and Methods
The present study was conducted in Kasturba Medical College, Mangaluru, a tertiary care teaching hospital. A retrospective analysis of 100 BCC cases received at the Department of Pathology from January 2006 to November 2014 was performed. The following clinical parameters were assessed for all the cases: identification data (name, sex, age), location of cancer, history of the disease and clinical diagnosis. The results were analysed after proper diagnosis based upon the clinical history, gross and histopathology findings. Proportions were described as percentages.
Results
Of the 100 cases of BCCs analysed, age ranged from 28 till 95 years out of which the most common age group was 61-80 years. Female patients (54%) were slightly more than male patients (46%) with a male to female ratio of 1:1.3 [Table/Fig-1].
Age and sex distribution of BCC.
| Age (in years) | Males | Females | Total |
|---|
| 21-40 | 0 | 3 | 3 |
| 41-60 | 20 | 15 | 35 |
| 61-80 | 22 | 33 | 55 |
| 81-100 | 4 | 3 | 7 |
| Total | 46 | 54 | 100 |
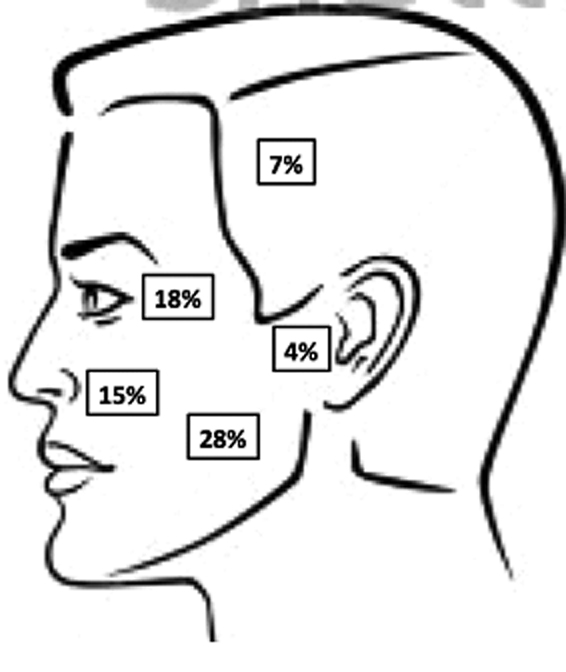
Of the 100 cases, face was the most common site (65%) followed by limbs (7%), scalp (7%) and trunk (4%). For 17 cases, details of the sites involved were unavailable. The distribution of lesion in the head and neck region is illustrated in [Table/Fig-2].
Topographical distribution of cases in head and neck region.
The size of tumour varied from 0.3cm to 6cm in maximum diameter. The distribution of size as per TNM classification is shown in [Table/Fig-3] [4]. For 7 cases, size was not recorded in the clinical data.
Distribution of size of the lesion [4].
| Size (in cm) | No. of cases (n=93) |
|---|
| <2 (pT1) | 67 |
| 2-5 (pT2) | 25 |
| >5 (pT3) | 1 |
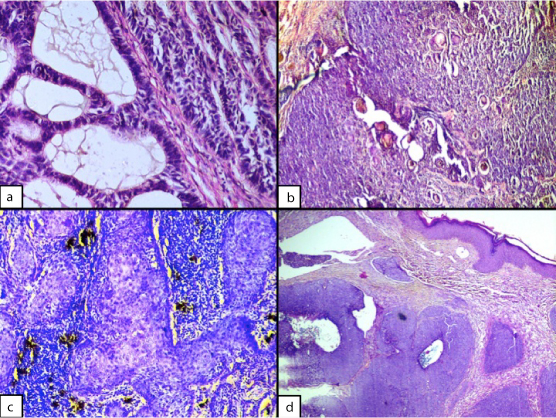
Majority of the BCCs were of the nodular/solid type (50%) on histopathology. The other common types were infiltrating (13%), pigmented variant (12%) and basosquamous/metatypical (6%). Other variants included pigmented (12 cases), adenoid (6 cases) and infundibulocystic (1 case) BCC [Table/Fig-4a-d]. One of the cases showed a mixed solid and adenoid pattern. [Table/Fig-5] shows the distribution of the various histopathological types.
(a) Adenoid BCC (H&E, 40x). (b) Keratotic BCC (H&E, 20x). (c) Metatypical BCC (H&E, 40x). (d) Nodulocystic BCC (H&E, 20x).
Histopathological types of BCC [4].
| Type | No. of cases |
|---|
| Nodular/solid | 50 |
| Infiltrating | 13 |
| Basosquamous/metatypical | 6 |
| Superficial | 4 |
| Keratotic | 3 |
| Micronodular | 3 |
| BCC with adnexal differentiation | 1 |
| Other variants (Pigmented, adenoid, infundibulocystic) | 19 |
| Mixed (solid and adenoid) | 1 |
| Total | 100 |
The clinical diagnosis and pathological diagnosis were concordant in 63 cases while the common discordant clinical diagnoses were seborrheic keratosis, nevus, malignant melanoma and squamous cell carcinoma. Few cases were clinically diagnosed as pyogenic granuloma, actinic keratosis, keratoacanthoma, hypertrophic scar, sarcoma and fibroepithelioma.
Discussion
BCC is the commonest skin malignancy in human beings. Squamous cell carcinoma is the most prevalent of the non-melanoma skin cancers in our country [7]. The incidence of BCC is not clearly known in our country, assumed to be because of the safeguarding effect of melanin on ultraviolet light (UVL)-generated injury [8]. The occurrence of BCC seems to be growing globally in the past decades [9]. The significant increase of the incidence in the last three decades was characterized by the phrase “silent epidemic of the twentieth century”.
Previous studies show that majority of skin cancers are seen in individuals aged 50 years or older [4,7–10]. Older people are more prone to develop BCC, however, they have also been reported in young adults and children [1]. In our study, 55% of the cases belonged to the seventh and eighth decades.
The frequency of skin cancers in men and women is different. BCCs are more widespread in males, supposedly because of more vocational and recreational subjection to UV rays. Recent trends show a slight increase in female patients, both young and old. This could be attributed to the fact that women are more cosmetically conscious and consult a specialist much earlier than men. Present study shows a slight female preponderance comparable to other studies [10–13]. A comparison of the results of previous studies done in India on BCC has been shown in [Table/Fig-6].
Comparison of previous studies on BCC in India.
| Author | Study period (years) | No. of cases | Age range (years) | Commonest site | Size range (cm) | Commonest histological pattern |
|---|
| Saldanha et al., [1] | 4 | 25 | 50-95 | Periorbital | 0.4–4 | Nodular |
| Malhotra et al., [9] | 3 | 34 | 28-102 | Periorbital | 0.5-8 | Nodular |
| Kumar et al., [11] | 3 | 36 | 29-92 | Nose | 0.5-5 | Nodular |
| Present study | 9 | 100 | 28-95 | Cheek | 0.3-6 | Nodular |
Most of the BCCs in our study measured <2cm. Giant BCC is normally defined as a BCC measuring more than 5cm at its largest diameter and constitutes less than 0.5% of all types [14–16]. In our study, there was one case of giant BCC measuring 6x5cm reported in an 87-year-old man, which presented as a mass in left shoulder and was clinically diagnosed to be a sarcoma.
BCCs in women tend to have smaller size, suggesting greater health care and early medical attention [6]. This observation was made in our study as well.
Up to 80% of all BCCs are found on head and neck with face being the most common site [17]. About 15% develop on the shoulders or trunk. There are unique reports of involvement of lower limbs [18], perianal region [19], clitoris and vulva [20], etc. Nevoid basal cell epithelioma (Gorlin) syndrome is associated with development of multiple BCCs [21]. In this study, 65% of all the cases were seen involving the face, which demonstrates the major influence of sun exposure in the development of skin cancers. This corroborates the result of a previous study by Souza et al., [22]. No other statistically significant trends were found with respect to any of the body sites in either males or females.
BCCs are defined as a group of malignant cutaneous tumours characterized by the presence of lobules, columns, bands or cords of basaloid cells (“germinative cells”) with peripheral palisading [1,4]. Most of the cases show adherence to the epidermis. Tumour islands are surrounded by a newly formed and different appearing stroma. Artefactual retraction spaces are often seen between the tumour and stroma. Inflammatory infiltrate is usually present in variable amounts.
Many histopathological types have been described [4,23]. Superficial BCC consists of superficial lobules of basaloid cells extending from the epidermis or from follicles or eccrine ducts into dermis and surrounded by a loose myxoid stroma [1,4]. Four cases in our series showed this pattern. Nodular (solid) BCC shows massive lobules of basaloid cells with peripheral palisading of nuclei that extend into the deeper dermis or further [4,13]. The most common histopathological pattern was the nodular (solid) in our study similar to other studies [24–26].
Micronodular variant has tiny nodules that invade dermis [1,4]. Three cases in our study showed this feature. Infiltrative patterns of BCC appear as cords, strands and columns of basaloid cells with little cytoplasm. This pattern is especially related to perineural invasion [1,23]. Thirteen cases in our study showed an infiltrating pattern. None of the carcinomas in our series showed perineural or vascular invasion. Cords of basaloid cells extending from epidermis downwards in an arborizing or fenestrating configuration characterizes fibroepithelial BCC [12].
BCC with adnexal differentiation includes sebaceous, ductal, trichilemmal components and basaloid buds [4,12]. We have solitary case of giant BCC in our study showing trichilemmal differentiation. Basosquamous (metatypical) carcinoma denotes basal cell carcinoma with squamous differentiation [Table/Fig-4]. This variant has a more invasive behaviour and is associated with local or extensive metastases [4,27]. The present study has 6 cases belonging to this type. Keratotic BCC is marked by the presence of notable keratin organization (horn cysts) in centers of tumour islands [1,11] [Table/Fig-4]. Three cases in our study belonged to this type.
Other variants constitute less than 10% of all BCCs. Adenoid variant consists of thin basaloid cell strands arranged in reticulate pattern [1]. Six cases of adenoid BCC were recorded in our study [Table/Fig-4]. Infundibulocystic variant is made up of tiny infundibular-like formations with central keratinous plug and peripheral element of basaloid cells [12,23]. One of our cases belonged to this group. Pigmented variant consists of melanocytes interspersed through the tumour nests and melanophages in the stroma [1,4]. Twelve cases in our study showed pigmentation. Other variants described are cystic, sclerosing (morpheiform) and miscellaneous variants with clear cells, granular cells, signet ring cells and giant (monster) cells [4,12,23].
Mixed pattern is fairly common [26], and has been documented from India [28]. In our study also, we have one case showing a mixed solid and adenoid pattern.
Multiple recurrences with deep residual tumour are associated with distinct morbidity as BCCs can ultimately penetrate even the bone. In our study, 11 cases included were recurrent BCCs. BCC recurrences are more common in lesions in the nasal area, however, this may be due to the difficulty in attaining adequate margins in these sites. Distance to the closest resection margin is a significant predictor of BCC recurrence. Precise microscopic evaluation of relapsing BCCs is very difficult for the pathologist because the tumour structure is significantly modified by scar formation and overproduction of the fibrous tissue, which alters the original morphology as well as the character of tissue infiltration [29].
Even though majority of BCCs are slow growing and comparatively non-aggressive, a minority have an invasive behaviour with local tissue damage and infrequently, metastasis [30]. Metastasis has been reported only in 0.0028-0.5% of all cases [6,31]. The present study showed absence of metastasis.
Limitation
Limitations of this study include lack of follow-up and absence of pediatric cases of BCC with syndromic manifestations.
Conclusion
BCCs comprise a significant proportion of all skin cancer patients in the world. Substantial amount of work exists in Indian literature, which is an evidence of a wide array of cases of BCC occurring in this country. The role of pathologists is irreplaceable in the diagnostic process because, in addition to giving the correct diagnosis, they also describe important morphological parameters of the tumour, some of which are of valuable prognostic significance. This study reveals the morphological spectrum of the disease in the population of southern Karnataka, India.