A Rare Mimicker in the Placenta
Akanksha Malik1, Sandhya Sundaram2, Bhuvana Srinivasan3, C.N Saishalini4, V Pavithra5
1 Post Graduate, Department of Pathology, Sri Ramachandra Medical College and Research Institute, Chennai, India.
2 Professor, Department of Pathology, Sri Ramachandra Medical College and Research Institute, Chennai, India.
3 Associate Professor, Department of Obstetrics and Gynaecology, Sri Ramachandra Medical College and Research Institute, Chennai, India.
4 Assistant Professor, Department of Pathology, Sri Ramachandra Medical College and Research Institute, Chennai, India.
5 Assistant Professor, Department of Pathology, Sri Ramachandra Medical College and Research Institute, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sandhya Sundaram, Professor, Department of Pathology, Sri Ramachandra Medical College and Research Institute, Porur, Chennai – 600116, Tamil Nadu, India.
E-mail: sandsrid@gmail.com
Mole, Placenta, Placental mesenchymal dysplasia
A 24-year-old primigravida with monochorionic monoamniotic pregnancy presented to our institution at 31+3 weeks of gestation with leaking per vaginum. The ultrasound findings were that of an enlarged and cystically dilated placenta, which raised the possibility of a differential diagnosis of partial mole. In view of foetal distress she was taken up for emergency caesarean section. Two healthy female twins were delivered with no features of Beckwith Wiedermann syndrome.
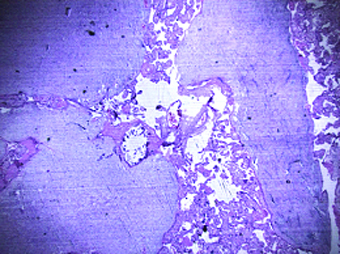
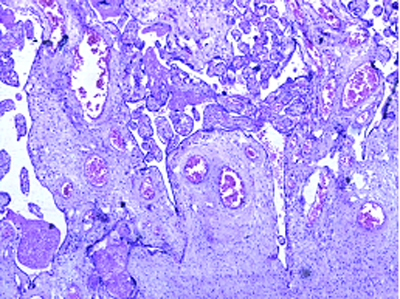
On gross examination the placenta weighed 800 gm and measured 17x15x2.5cm. The two umbilical cords attached measured 20cm and 24cm respectively [Table/Fig-1]. Foetal surface showed prominent, dilated blood vessels. The maternal surface was intact with cotyledons. Tiny, white nodules were seen on the foetal side. The cut surface of the placenta was beefy red with no pale areas. A focal area showed pinkish white vesicle like area [Table/Fig-2].
Enlarged placenta (M) 17x15x2.5cm with two umbilical cords.

Placenta showing multiple grape like vesicles.

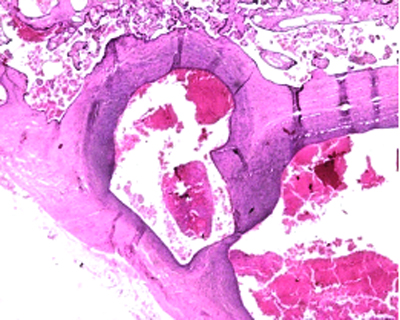
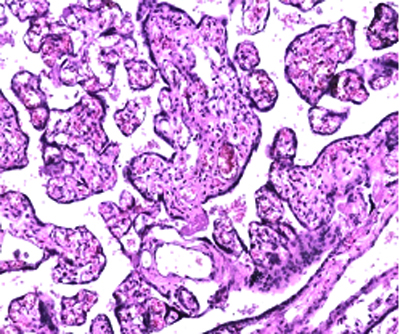
The umbilical cords showed three vessels each. Multiple sections from the placenta showed villi of varying sizes [Table/Fig-3]. Some of the stem villi appeared markedly hydropic with stromal fibroblast proliferation. Concentric fibrosis was seen around the blood vessels [Table/Fig-4]. There was thick walled blood vessels with organising thrombus formation noted [Table/Fig-5]. Rest of the villi showed chorangiosis like change [Table/Fig-6]. Few villi showed central cistern formation, however, there was no trophoblastic proliferation. Sections from the villi appeared unremarkable.
Histopathology showed dilated stem villi (H&E 40x).
Histopathology showed concentric fibrosis in the villi (H&E 100x).
Histopathology showed organising thrombus (H & E 100x).
Histopathology showed increased number of blood vessels per villi, showing chorangiosis like change (H&E 200x).
Discussion
The presence of an enlarged cystically dilated placenta on ultrasound raises the differential diagnosis of partial mole, complete mole with healthy co-twin and placental mesenchymal dysplasia. In PMD (placental mesenchymal disease) the cystic spaces are seen to migrate towards the chorionic plate [1]. Pathological examination is necessary to arrive at a definitive diagnosis in such a scenario.
Placental mesenchymal dysplasia is a recently described entity by Moscoso et al., as a condition characterised by stem villous hyperplasia [2], elevated alfa foeto protein and enlarged cystically dilated placenta on ultrasound. It is a rare entity with an incidence of 0.02% [3]. Less than 100 cases have been reported in literature till date. In around one fourth of the cases it has been found to be associated with Beckwith Wiedermann syndrome [1].
Differentiation from gestational trophoblastic disease is essential as the prognosis and treatment modalities differ. The delivery of normal twins ruled out the diagnosis of complete mole.
Around one fourth of the cases are associated with Beckwith-Wiedermann syndrome, characterized by macrosomia, exomphalos, macroglossia, omphalocele, internal visceromegaly, placentomegaly and increased childhood tumours [4]. However, in our case there were no external features of Beckwith-Wiedermann syndrome and the twins had no gross abnormalities.
The clinical presentation is raised maternal alpha feto protein, normal to slightly increased BHCG (beta human chorionic gonadotropin) which resolves soon after delivery. The presentation in the third trimester can be that of complications associated with PMD such as intrauterine growth retardation and intrauterine demise.
The elevated alpha feto protein in this scenario is thought to be of foetal origin as there is increased surface area for exchange [2].
Pathogenesis may be related to hypoxia of unknown aetiology leading to fibroblast proliferation, increased expression of vascular endothelial growth factor eventually leading to angiogenisis [1]. There is a distinct female preponderance reported with the female to male ratio being 3.6:1 [1]. In our case both the babies were female.
In the cases where ploidy studies have been carried out, majority of PMD cases with rare exception were found to be diploid. This may help to distinguish from partial mole where the karyotype results are triploid [1]. These tests, however, do not contribute to exclude the other differential diagnoses of complete mole with co twin as they are also diploid.
Grossly the placenta is large for gestational age. The chorionic plate vessels are abnormally dilated and tortuous. Some may show abnormal branching. There can be thrombus formation in the vessels and rupture leading to further compromise in foetal growth [1]. Cystic vesicles ranging from 0.3 to 2.5cm can be visible grossly, which may arise the possibility of molar gestation.
Microscopically, placental mesenchymal dysplasia has distinct features which exclude other diagnoses. The placentas with PMD show fibro muscular hyperplasia of the chorionic plate blood vessels. There may be luminal obstruction as a result of fibrinoid necrosis and organizing thrombus. The stem villi in PMD are enlarged with fibroblast proliferation and myxoid stroma. Some villi may exhibit cistern formation with gelatinous areas. Interspersed amongst the dilated stem villi, normal villi are present [1].
The vessels in the villi range from normal to showing chorangiomatous changes. In the case presented here, there were few areas showing chorangiomatous areas.
The features which differentiate PMD from molar gestation are lack of trophoblastic proliferation and absence of scalloping [1]. In our case, none of the aforementioned was present hence, the diagnosis of molar pregnancy was ruled out.
The complications of PMD in the foetus range from prematurity, intrauterine growth restriction and intrauterine death. However, these are postulated to arise due to hypoxia [1]. Rare complications such as vascular hamartoma and hepatic mesenchymal hamartoma have been reported [1,5]. There is no direct relation between PMD and maternal complications like polyhydramnios and gestational diabetes, but is hypothesised to be linked to the degree of vascularity [1].
PMD is rare however, it should be kept in mind as a differential diagnosis to prevent unnecessary termination of pregnancy, since majority of the foetuses have normal genotype.
[1]. Parveen Z, Tongson-Ignacio JE, Fraser CR, Killeen JL, Thompson KS, Placental mesenchymal dysplasiaArch Pathol Lab Med. College of American Pathologists 2007 131(1):131-37. [Google Scholar]
[2]. Moscoso G, Jauniaux E, Hustin J, Placental vascular anomaly with diffuse mesenchymal stei villuos hyperplasia: a new clinico-pathological entity?Pathol Pract 1991 187(2)Elsevier:324 [Google Scholar]
[3]. Robertson M, Geerts LTGM, de Jong G, Wainwright H, Mesenchymal dysplasia in a monochorionic diamniotic twin pregnancy with review of the differential diagnosis of cystic changes in the placentaJ ultrasound Med. Am inst Ulrrasound Med 2007 26(5):689-93. [Google Scholar]
[4]. Taga S, Haraga J, Sawada M, Nagai A, Yamamoto D, Hayase R, A case of placental mesenchymal dysplasiaCase Rep Obstet Gynecol 2013 2013Hindawi Publishing Corporation [Google Scholar]
[5]. Francis B, Hallam L, Kecskes Z, Ellwood D, Croaker D, Kent A, Placental mesenchymal dysplasia associated with hepatic mesenchymal hamartoma in the newbornPediatric and Developmental Pathology 2007 10(1):50-54. [Google Scholar]