Corneal diseases is the major cause of visual impairment and blindness in developing world [1]. The transparency of the cornea is affected by various infectious and inflammatory conditions which cause corneal blindness and add substantial burden to the community and health care resources all over the world. The data available in 2000 suggests that there are approximately 50 million blind people in the world [2]. In India, there are approximately 6.8 million people who have corneal blindness with vision less than 6/60 in at least one eye, out of which, about 1 million are bilateral corneal blind [3]. Keratoplasty is the only procedure to restore vision in corneal blindness and its success rate is very low in developing countries (46.5%) as compared to developed countries [4]. There are so many reports on indications for penetrating Keratoplasty (PK) in developed and developing countries. The indications of PK with poor prognosis for graft survival are more common in India as compared to the developed world [5].
The purpose of present study was to evaluate the indications and success rate of PK by assessing its outcome in the population of this part of the country and to compare them to the other global reports.
Materials and Methods
We obtained approval from hospital administrators and research committee to conduct this study. Data were obtained by reviewing the medical records of 145 PK’s done from January 2012 to October 2014 retrospectively.
The patients were divided into three age groups 0-14 yrs, 15-49 years, ≥50 years and were analysed for the indications of keratoplasty. Indications of PK were divided into 8 main diagnostic categories-bullous keratopathy, infectious keratitis, corneal opacity or scarring, graft failure, anterior staphyloma, corneal dystrophy, keratoconus and others [Table/Fig-1]. Optical Penetrating Keratoplasty (OPK) was done for purpose of visual regain. Therapeutic Penetrating Keratoplasty (TPK) was performed for active bacterial and fungal corneal ulcers which were included in category of active infectious keratitis. The patients of PK with follow-up less than one year were excluded from the study.
Indications of keratoplasty.
| Bullous keratopathy (PBK + ABK) 36 + 3 = 39 | 39 (26.89%) |
| Active infective keratitis | 30 (20.68%) |
| Corneal scarring | 48 (33.10%) |
| Graft failure | 17 (11.72%) |
| Anterior staphyloma | 4 (2.75%) |
| Corneal dystrophy | 4 (2.75%) |
| Keratoconus | 1 (0.68%) |
| Others (tectonic patch, corneal burns)1+1=2 | 2 (1.37%) |
| Total | 145 (n) |
PBK: Pseudophakic bullous keratopathy
ABK:Aphakic bullous keratopathy
In situ, corneoscleral rim excision was done for all eye donations and donor tissue was collected in Mc Carey-Kaufman (M-K) medium with all aseptic precautions. Tissues were graded by grading chart by National Eye Bank as Grade A, B+, B, B-, C and D [6]. Donor tissues graded A, B+ were used for OPK and Grade B or less were used for TPK.
All OPK’s were done under peribulbar anaesthesia and TPK’s were done under general anaesthesia. Standard technique of keratoplasty with donor grafts 0.5 mm larger than the recipient was followed in all cases. Both interrupted and continuous suturing was done depending upon the indications, vascularity and infection. The recepient button and donor corneoscleral rim were sent for histopathological examination. Routine postoperative medication consisted of topical prednisolone 1% combined with topical antibiotic six times daily along with artificial tears. Routine follow up schedule was weekly for first month, biweekly for second month, monthly for 3 to 6 month and 3 monthly for 1 year. Topical antibiotic were reduced over the subsequent postoperative month and 1% prednisolone tapered down after 6 months with once daily dose lifelong. For post-herpetic cases, prophylactic oral acyclovir was given for one year. We did not use systemic immunosuppressive. The suture removal was done after completion of one year except in few cases where selective interrupted sutures were removed if was associated with infilterates or vascularisation. Best Corrected Visual Acuity (BCVA) with pin hole, glasses and rigid gas permeable lenses for high astigmatism, intraocular pressure (IOP) and graft clarity were recorded postoperative 1, 3, 6 months and 1 year period for all patients. One year follow-up was considered as last follow-up. Records were reviewed for age, sex, preoperative diagnosis, and preoperative BCVA. Surgical details were noted in terms of grades of the graft used and any additional procedures like cataract surgery, trabeculectomy, intraocular lens (IOL) explantation, triple procedure, vitrectomy and goniosynechiolysis, etc.
Outcomes were evaluated in terms of infection cure rate in therapeutic grafts, graft clarity and final BCVA for optical grafts. Complications if any were noted for all cases. Graft rejection was considered mild if there were 1-5 keratic precipitates (KP’s), subepithelial infiltrates, increased corneal thickness without anterior chamber reaction and severe if >5KP’s with stromal infiltrates, endothelial rejection line, increased corneal thickness with anterior chamber reaction. Graft clarity was grade 4 if clear view of iris details was possible, grade 2-3 without good view of iris details and grade 1-0 for opaque graft with no or poor view of anterior chamber details [7]. Graft failure was defined as irreversible loss of graft clarity with rejection episode for 3 months or more.
Statistical Analysis
Data was analysed using Microsoft excel 2010 and SPSS version 22. BCVA were converted from the snellen units to the logarithm of minimal angle of resolution (logMAR). Paired student’s t-test were used for hypothesis testing of grouped values of preoperative and last follow-up BCVA in cases of optical and therapeutic grafts. A p-value < 0.05 was considered statistically significant.
Results
In the present study 145 eyes of 138 patients were reviewed, as six were regrafts and one was bilateral. The age at which PKs were done ranged from 8-83 year (mean 51.64 years SD 18.45 years). In this study males and females were 94(68.11%) and 44(31.88%) respectively. Maximum patients 97(66.89%) were above 50 years of age. Right eye was involved in 75(51.72%) cases.
Indications of PK
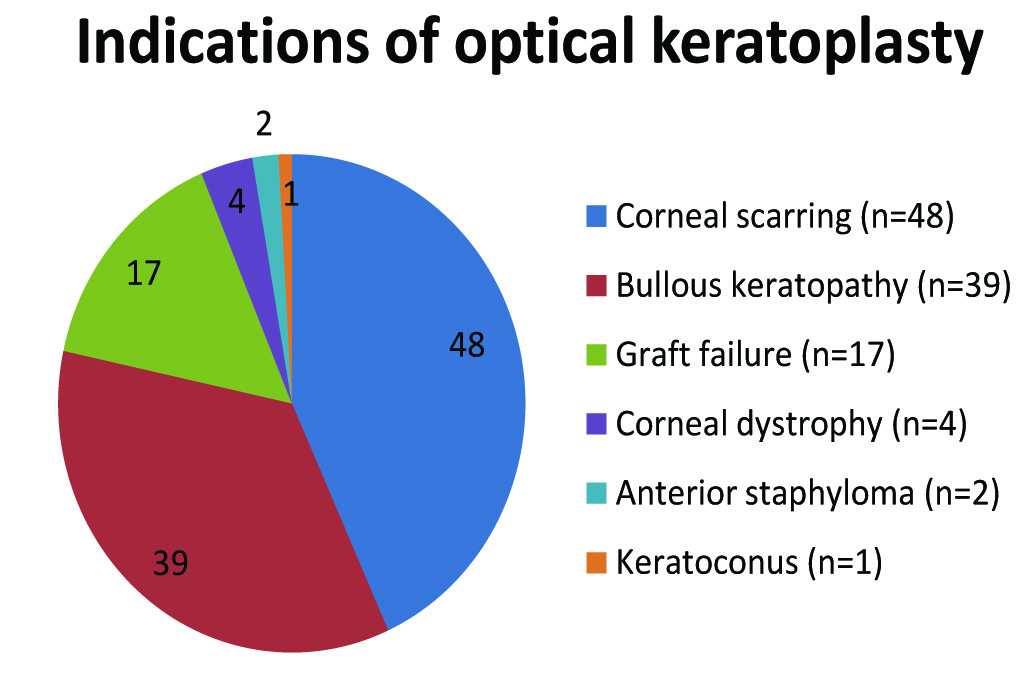
The most common indication for PK was corneal scarring including adherent leucoma 48 (33.10%) and least common indication was keratoconus 1 (0.68%). Corneal dystrophy was seen in 4 (2.75%) cases with Congenital Hereditary Endothelial Dystrophy(CHED) in 1(25%) case and stromal dystrophy (2 eyes of granular dystrophy type 1 and one eye of granular dystrophy type II) in 3(75%) [Table/Fig-1]. There were 111 eyes which underwent OPK, with various indications [Table/Fig-2].
Pie chart showing distribution of indications of optical penetrating keratoplasty.
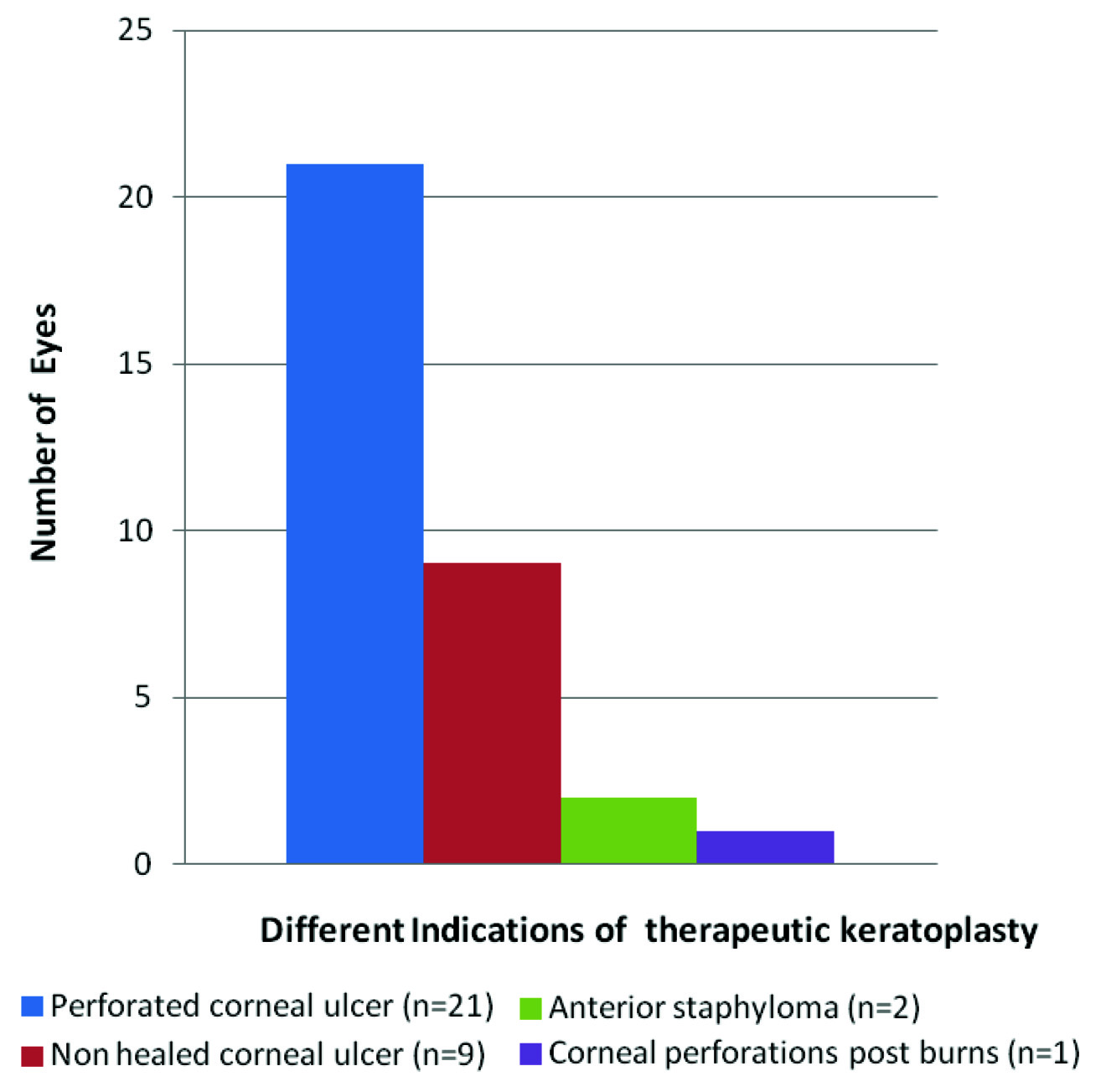
TPK was done for 33 cases. Among 30(20.68%) cases with infectious keratitis, maximum 21(63.63%) cases were perforated corneal ulcers and 9(27.27%) were nonhealing corneal ulcers which were either not responding to treatment or were impending to perforate. Among the infective keratitis cases 7(23.33%) cases were bacterial and 5(16.66%) cases were proven fungal by the histopathological report of the recipient button [Table/Fig-3]. Tectonic grafting was done for corneal perforation in one case in which a large foreign body was removed from anterior chamber.
Showing distribution of indications for therapeutic penetrating keratoplasty.
Surgical Information
PK was done for optical reasons in majority of 111(76.55%) eyes. Plain OPK and triple procedure was done in 85(76.57%) and 14(12.61%) respectively. In 2(1.80%) cases IOL was not put because of very high myopia in one case and posterior capsular rent in other case where anterior vitrectomy was done [Table/Fig-4]. In all cases, graft graded as A and B+ were used.
| Optical PKa) Plain optical PK=85(76.57%)b) With ECCE+PCIOL=14(12.61%)c) Without PCIOL=2(1.80%)d) IOL explants=10(9%) | 111(76.55%) |
| Therapeutic PK | 33(22.75%) |
| Tectonic PK | 1(0.68%) |
| Total | 145 |
PK: Penetrating keratoplasty
ECCE+PCIOL: Extracapsular cataract extraction+posterior chamber intraocular lens
PCIOL: Posterior chamber intraocular lens
IOL: Intraocular lens
Outcome of Optical Grafts
In all the cases which underwent OPK the preoperative BCVA was <20/200 out of which 105(94.59%) were of BCVA <20/400. At last follow-up maximum cases 50 (45.04%) fell into the level of BCVA of 20/60-20/200 and 36 (32.43%) got BCVA of >20/60 [Table/Fig-5]. All cases of corneal dystrophy and keratoconus got BCVA of >20/60 at last follow up except one case in which graft failed. The BCVA improved from 1.39 logMAR+ 0.022(SD) preoperatively to 0.367 logMAR+0.44(SD) postoperatively at the last follow-up of one year. There was statistically significant difference (p=.0001, n=111) with a mean difference of 1.02.
Showing distribution of visual acuity in optical grafts.
| BCVA | Pre OPK | Last follow-up 12 months post OPK |
|---|
| >20/60 | 0 | 36 (32.43%) |
| 20/60-20/200 | 0 | 50 (45.04%) |
| <20/200-20/400 | 6 (5.40%) | 8 (7.20%) |
| <20/400 | 105 (94.59%) | 17 (15.31%) |
| n=111 | n=111 |
BCVA: Best corrected visual acuity
Pre OPK: Pre optical penetrating keratoplasty
Post OPK: Post optical penetrating keratoplasty
The graft clarity was grade 4 in 83 (74.77%), grade 3 in 12(10.81%) and grade I in 16(14.41%). 11(9.90%) eyes developed post keratoplasty glaucoma (PKG) which was refractory to the three antiglaucoma medication and trabeculectomy with mitomycin C (0.2mg/ml) was done to save the graft in all cases. In (n=2) cases had pre-existing glaucomatous optic atrophy which led to graft failure and in rest (n=9) graft survived with good visual outcome of BCVA (20/60-20/200). Secondary graft failure occurred in 15 (13.51%) eyes due to infection, ≥ 2 episodes of severe graft rejection, endothelial failure and glaucoma in 6(40%), 5(33.3%), 2(13.33%), 2(13.33%) respectively. Out of 6 cases of infection, two cases were recurrent herpetic viral keratitis presented with persistent epithelial defect and graft thinning. Amniotic membrane transplantation was done for these cases to avoid perforation and goal was achieved but graft got opacified. 7 (6.30%) cases had one episode of mild graft rejection and were given methypredinisolone 1 gm intravenous stat followed by oral and topical steroids as well as immunosupressants like topical cyclosporine (0.05%) and rejection was reversed with clear graft. In three cases subconjuctival avastin (2.5mg in 0.1ml) was given for regression of the graft vascularisation ≥2 quadrants. All these cases recovered good graft clarity and visual outcome. In one case of PBK the retained host’s descemet’s membrane was detected after one week of OPK and explantation of PCIOL. After three months descemetorhexis was done which resulted in grade 4 graft clarity and visual outcome of 20/40 with aphakic correction.
Outcome of Therapeutic Grafts
Therapeutic Success
Therapeutic success was defined as complete eradication of primary infection after keratoplasty with appropriate adjunctive medical therapy. For visual acuity and graft clarity assessment one case of tectonic graft was considered under group of TPK as the donor cornea used was of grade B-. Of the 34 patients 30 (88.25%) patients achieved therapeutic success maintaining structural integrity as (n=1) underwent evisceration and (n=3) got phthisical. Therapeutic failure was defined as recurrent graft infection despite medical and surgical intervention. Therapeutic failure occurred in 3(8.82%) cases, in two cases amniotic membrane transplantation was done to avoid graft melting and stabilisation of infection was achieved and one eye underwent evisceration. Complications other than reinfection were glaucoma in 5(14.7%) cases that underwent trabeculectomy, choroidal detachment in one case which resolved later on with oral steroids and glaucomatous optic atrophy in one case. All cases had BCVA <20/400 at presentation. At last follow-up only 1(2.94%) eye had BCVA of > 20/60 and maximum cases 19(55.88%) fell in the group of <20/400 [Table/Fig-6]. The graft clarity was grade 4, 3 and 1 in 9(26.47%), 7(20.58%) and 18(52.94%) cases respectively.
Showing distribution of visual acuity in therapeutic grafts.
| BCVA | Pre TPK | Last follow-up 12 months post TPK |
|---|
| >20/60 | 0 | 1 (2.94%) |
| 20/60-20/200 | 0 | 13 (38.23%) |
| <20/200-20/400 | 0 | 1 (2.94%) |
| <20/400 | 34 (100%) | 19 (55.88%) |
| n = 34 | n = 34 |
BCVA: Best corrected visual acuity
Pre TPK: Pre therapeutic penetrating keratoplasty
Post TPK: Post therapeutic penetrating keratoplasty
The BCVA improved from 1.4 logMAR+ .000(SD) preoperatively to 0.16 logMAR+.0.57 (SD) postoperatively at the last follow up. There was statistically significant difference (p=.0001, n=34) with the mean difference of 1.23.
Discussion
PK can visually rehabilitate corneally blind patients with various corneal pathologies. Its prognosis and outcome depends on the pathology responsible for corneal blindness or visual impairment [8].
Infective keratitis was common component in both optical and therapeutic grafts as healed and active keratitis in respective grafts. As compared to present study the corneal scarring has been reported to be the proportionally less indication in developed world [9,10]. Bullous keratopathy was second common indication for PK in the present study of 39(26.89%) of total indications which is comparable to other studies [5,11]. In this study pseudophakic bullous keratopathy (PBK) was more common than aphakic bullous keratopathy (ABK). Corneal dystrophies and keratoconus formed very small proportion of indications as compared to developed countries where keratoconus made up higher proportion of the indications for PK ranging from 7.0% to 31% with a median value of 17.1% [12–14]. Infective keratitis formed the major indication (40.9%) for keratoplasty in Nepal [15] which is very high as compared to Indian studies [Table/Fig-7] [5,11,15–17].
Comparison of indications of PK in different parts of the world.
| Indications | Rahman et al., (U.K) [17] | Bajracharya et al., (Nepal) [15] | Dandona et al., (India) [5] | Sony et al., (India) [11] | Laxman et al., (India) [16] | Present study |
|---|
| Corneal scarring | | 26.8% | 28.1% | 38.03% | 60.7% | 33.10% |
| Infective keratitis | 9% | 40.9% | 12.2% | 28.38% | 2.94% | 20.68% |
| Bullous keratopathy | 21% | 9.0% | 22.4% | 13.45% | 8.82% | 26.89% |
| Graft failure | 20% | 11.3% | 17.1% | 11.5% | 12.7% | 11.72% |
| Corneal dystrophy | 14% | 1.7% | 8.4% | 3.85% | | 2.75% |
| Keratoconus | 24% | 7% | 6% | 2.37% | 1.96% | 0.68% |
The OPK and TPK were done for different indications but the difference of visual outcome preoperatively and last follow-up was statistically significant in both indications.
Optical Keratoplasty
The commonest indication of OPK in this study was corneal opacity due to scarring which is comparable to the results of other published Indian studies [5,9,16]. On the contrary, corneal scarring was not the indication for OPK at all in western countries but keratoconus was the major indication for PK in 24% [17] which was quite high as compared to the present study of (0.68%) [Table/Fig-5]. All cases of corneal dystrophy and keratoconus were there in the group of BCVA of > 20/60 except one case of corneal dystrophy in young child of 8 years where triple procedure was performed but graft failed. In present study, corneal dystrophy and keratoconus were good prognosis cases as reported by Dandona et al., [18]. All four cases of ABK developed glaucoma due to which graft failed in three cases but one graft could survive due to early trabeculectomy. ABK was one of the worst prognosis in optical grafts as supported by other study [18].
Therapeutic Keratoplasty
The success of TPK lies in eradication of the primary infection and salvagability of the globe. The patients may lose their sight and possibly their eye due to severe infection and inflammation. Poor prognosis is expected in patients receiving emergency therapeutic transplantation for severe infectious keratitis. Following stabilization of the eye, repeat keratoplasty can be performed on an elective basis for optical purposes. Of the 34 patients 29 (85.29%) patients achieved therapeutic success maintaining structural integrity and stabilization of the eye which is comparable to the results of Ti et al., [19]. In present study only 14(41.17%) cases regained BCVA >20/200 [Table/Fig-6] which is comparable to the results of Ti et al [19] where the number of eyes with BCVA >6/60 (20/200) was 58.5%. Graft clarity varied by indications for transplantation as in corneal scarring, infective keratitis and keratoconus. The graft clarity was comparable to Indian study by Varghese et al., [20]. For bullous keratopathy graft clarity in present study was comparable to the studies conducted by Randleman et al., and Zare et al., [21,22] [Table/Fig-8].
Comparison of graft clarity based on indications of PK in different parts of the world.
| Indications | Varghese et al., (Kerala) [20] | Randleman et al., (Atlanta) [21] | Zare et al., (Iran) [22] | Present study |
|---|
| Corneal scarring | 81.38% | 66.7% | 68.6% | 83.4% |
| Infective keratitis | 41. 45% | 40% | 32.6% | 42.4% |
| Bullous keratopathy | 95.5% | 76.5% | 75% | 79.5% |
| Graft failure | 69.76% | 39.1% | 46.7% | 82.35% |
| Corneal dystrophy | 93.66% | | | 75% |
| Keratoconus | 96.88% | 87.5% | 88.9% | 100% |
All indications of PK represent the pattern of corneal blindness among those who have undergone keratoplasty in this institute being the only registered eye bank of the state.
Limitations
There are few limitations to the present study as we did not analyse donor details like age of donor, cause of death of donor, death to enucleation and death to preservation time of donor tissue which can affect graft survival. Specular microscopy of donor eye was lacking due to non-availability of this facility. For cases of corneal dystrophy deep anterior lamellar keratoplasty was not done due to restraints of the facility required for the same. Visual outcome assessment is based on BCVA but the data regarding astigmatism is not available for the whole series.
Conclusion
In this study, ulcerative keratitis either active or healed was the major cause for both types of PK’s with good visual recovery. Infective keratitis was found to be common due to predominance of occupation of farmers in this part of Indian subcontinent. Before transplantation 95.17% eyes were blind (visual acuity <3/60) but after PK that percentage dropped to 24.82% at last follow-up. The data reported in this paper suggest that PK can be a reasonably successful procedure for visual outcome in this part of developing world for most of the indications.
PBK: Pseudophakic bullous keratopathy
ABK:Aphakic bullous keratopathy