Clinicopathological and Immunohistochemical Characteristics of Verruciform Xanthoma of the Lower Gingiva: A Case Report
Masashi Kimura1, Hiroyuki Ohto2, Akio Shibata3, Atsushi Enomoto4, Masahiro Umemura5
1 Attending Staff, Department of Dentistry Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, 4-86 Minaminokawa-cho, Ogaki, Gifu, Japan.
2 Chief, Department of Dentistry Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, 4-86 Minaminokawa-cho, Ogaki, Gifu, Japan.
3 Attending Staff, Department of Dentistry Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, 4-86 Minaminokawa-cho, Ogaki, Gifu, Japan.
4 Associate Professor, Department of Pathology, Nagoya University Graduate School of Medicine, 65 Tsurumai-cho, Showa-ku, Nagoya, Japan.
5 Director, Department of Dentistry Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, 4-86 Minaminokawa-cho, Ogaki, Gifu, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Masashi Kimura, Attending Staff, Department of Dentistry Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, 4-86 Minaminokawa, Ogaki, Gifu 503-8502 Japan. E-mail : masashi.kimura009@gmail.com
Verruciform xanthoma (VX) is a rare benign lesion and mainly effects the oral mucosa. This slow-growing asymptomatic lesion typically develops along the gingival margin of the masticatory mucosa, followed by the hard palate, tongue, buccal mucosa, floor of the mouth, alveolar mucosa, soft palate and junction between the hard and soft palate. Moreover, this lesion can also affect the skin and genital organs. Clinically, VX generally presents a sessile or pedunculated appearance, forming a papule or single plaque with verrucous or papillomatous mucosal growth. The colour (white, pink, grey, or yellow) depends on the thickness of the overlying epidermis. In fact, the clinical findings of VX are similar to those of verrucous carcinoma and other benign tumours, such as squamous papilloma, verruca vulgaris and mucosal fibroma. For this reason, clinical and histopathological examinations are essential for accurate differential diagnosis. Histologically, VX is characterized by parakeratosis, rete ridges of uniform depth and the accumulation of foam cells, which are also called “xanthoma cells”. Here, we describe the clinicopathological and immunohistochemical findings of a VX located on the lower gingiva of a 64-year-old male patient.
Immunohistochemistry, Oral cavity, Xanthoma cells
Case Report
A 64-year-old Japanese male presented at our hospital complaining of a mass on the gingiva. He first noticed the painless mass two years ago. Intraoral examination revealed a well-circumscribed, sessile nodule with slight pedunculation on the right lingual aspect of the lower central incisor [Table/Fig-1a]. The nodule was pink and about 7×7 mm in diameter. Slight calculus was also present on the lingual surface of the central incisor.
(a) Intraoral examination revealed a well-circumscribed, sessile nodule with slight pedunculation on the right lingual aspect of the lower central incisor; (b) The lesion was excised with 3-5mm safety margins and removal of periosteal tissue underneath the lesion; (c) Histopathological examination revealed a hyperparakeratinized stratified squamous epithelium with uniform elongated epithelial ridges (H&E, 4x); (d) Numerous large macrophage foam cells (xanthoma cells) had accumulated in the subjacent connective tissues between the epithelial ridges (H&E, 20x); (e) The foam cells exhibited diffuse expression of CD68 (IHC staining 20x); (f) Ki-67; and (g) p63 expression were predominantly observed in the basal or parabasal layers of the epithelium (IHC staining 10x).
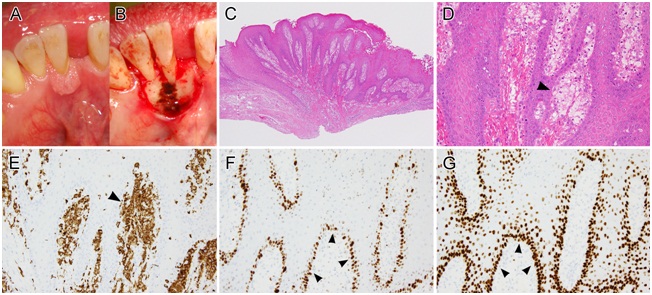
Exfoliative cytology of the lesion revealed epithelial cells exhibiting mild cytologic atypia and few mitoses. Therefore, a provisional diagnosis of epulis was established, and an excisional biopsy was performed to rule out malignancy [Table/Fig-1b]. The lesion was excised with 3-5mm safety margins and removal of periosteal tissue underneath the lesion. Histopathological examination revealed a hyperparakeratinized stratified squamous epithelium with uniform elongated epithelial ridges [Table/Fig-1c]. In addition, chronic inflammatory infiltrate was found in the connective tissue underneath the epithelium. Numerous large macrophage foam cells (xanthoma cells) had accumulated in the subjacent connective tissues, between the epithelial ridges [Table/Fig-1d]. The overlying epithelium showed mild nuclear and cytologic atypia. Based on these findings, a diagnosis of VX was established. Immunohistochemistry revealed that the macrophage foam cells expressed CD68, whereas the expression of Ki-67 and p63 was limited to the basal or parabasal layer, indicative of a hyperproliferative lesion rather than a malignant tumour [Table/Fig-1e-g]. The diagnosis of VX was supported by these immunohistochemical findings. After the lesion was resected, the surgical site underwent normal secondary healing processes. In addition, there was no evidence of recurrent disease during the follow-up period.
Discussion
Verruciform xanthoma (VX) is a rare tumour-like lesion that was first described in 1971 by Shafer [1]. VX develops in the oral mucosa as well as the skin and genital organs. A worldwide survey of the literature indicated that 282 cases of oral VX have been reported in females (mean age: 54.9 years) and males (mean age: 44.2 years) with a female:male ratio of 1:1.1 [2]. This review showed that 73.4% of all VX lesions occur in the masticatory mucosa. Furthermore, few cases of multiple lesions have been reported [3].
Clinically, VX present as a papule or single plaque with verrucous or papillomatous mucosal growth. The size of the lesion ranges from 2 to 20 mm, whereas they may maintain the normal colour of the oral mucosa, the colour is occasionally yellowish red or brownish, pale or whitish and hyperkeratotic [4]. These clinical findings may be mistaken for malignant lesions, viral warts or benign/premalignant mucosal disease. Thus, histopathological examination is essential for the differential diagnosis.
Histologically, VX is characterized by the papillary or verrucous proliferation of a stratified squamous epithelium, associated with acanthosis and hyperkeratosis. In addition, rete ridges of uniform depth and connective tissue papillae extend up to the surface and lipid-laden foam cells accumulate in the subjacent connective tissue between the rete ridges. Similar histopathological features were detected in the present case. However, exfoliative cytological analysis did not reveal the presence of foam cells in the specimens, suggesting that this collection technique is too superficial to collect cells from connective tissues. On the other hand, immunohistochemical analysis revealed that the foam cells express CD68, indicating that they were derived from macrophages [5]. Positive reactivity for Ki-67 and p63 was predominantly detected in the basal or parabasal layers. Together, these findings support benign characteristics for this case of VX.
Three types of VX have been recognized based on their microscopic surface architecture [6]. Type A (verrucous type) - shows as hyperparakeratosis, acanthosis and elongation of the rete ridges. Type B (papillary type) - shows fingerlike projections of stratified squamous epithelium, containing connective tissue cores. Type C (flat type) - shows mild acanthosis, variable elongation of rete ridges and subtle thin parakeratosis. There are studies which found that the flat type of lesion to be the most common type [6,7]. The present case was identified as a papillary lesion because of the stratified squamous epithelium, the uniform elongated epithelial ridges and the connective tissue cores between the ridges.
The pathogenesis of VX remains largely unknown. Although the mass typically accumulates lipid-containing foam cells in the submucosa or dermis, most patients do not have hyperlipidemia. Ide et al., suggested that highly wet microenvironments, periodontopathic pathogens, mechanical stimuli, tobacco, alcohol, drugs, sensitizing or allergic agents in foodstuff and dental materials are likely to play a pathogenic role, either triggering and/or promoting oral VX formation. Furthermore, this study showed that under the synergistic regulation of T cells, monocyte chemoattractant protein-1 (MCP-1)/chemokine receptor 2 (CCR2)-mediated macrophage recruitment in the sub-basal papillae and the lysosomal engulfment of epithelial lipids by macrophage scavenger receptor-1 (MSR-1)-bearing macrophages may play a crucial role in VX formation [4].
The treatment of choice for VX is complete surgical excision [8] because currently there is no evidence that VX could be a precancerous lesion [2]. Furthermore, the recurrence or malignant transformation of VX are extremely rare, and this lesion usually has a good prognosis [9]. However, a prolonged follow-up is preferred because the cause of this lesion remains unclear.
Conclusion
In conclusion, this lesion may be misdiagnosed clinically as a malignant disorder, such as verrucous carcinoma. The present case illustrates the importance of clinicopathological and immunohistochemical examinations for the diagnosis of VX. Complete resection is an adequate treatment with a favourable prognosis.
Conflict of Interest: The authors have no conflict of interest to declare.
[1]. Shafer WG, Verruciform xanthomaOral Surg Oral Med Oral Pathol 1971 31:784-89. [Google Scholar]
[2]. Philipsen HP, Reichart PA, Takata T, Ogawa I, Verruciform xanthoma—biological profile of 282 oral lesions based on a literature survey with nine new cases from JapanOral Oncol 2003 39:325-36. [Google Scholar]
[3]. Qi Y, Sun Q, Yang P, Song A, A case of multiple verruciform xanthoma in gingivaBr J Oral Maxillofac Surg 2014 52:e1-3. [Google Scholar]
[4]. Ide F, Obara K, Yamada H, Mishima K, Saito I, Kusama K, Cellular basis of verruciform xanthoma: immunohistochemical and ultrastructural characterizationOral Dis 2008 14:150-57. [Google Scholar]
[5]. Shahrabi Farahani S, Treister NS, Khan Z, Woo SB, Oral verruciform xanthoma associated with chronic graft-versus-host disease: a report of five cases and a review of the literatureHead Neck Pathol 2011 5:193-98. [Google Scholar]
[6]. Nowparast B, Howell FV, Rick GM, Verruciform xanthoma. A clinicopathologic review and report of fifty-four casesOral Surg Oral Med Oral Pathol 1981 51:619-25. [Google Scholar]
[7]. De Andrade BA, Agostini M, Pires FR, Rumayor A, Carlos R, de Almeida OP, Oral verruciform xanthoma: a clinicopathologic and immunohistochemical study of 20 casesJ Cutan Pathol 2015 42(7):489-95. [Google Scholar]
[8]. Aggarwal S, Aggarwal A, Gill S, Bakshi Y, Singh HP, Verruciform xanthoma of oral cavity- a case reportJ Clin Diagn Res 2014 8:FD11-12. [Google Scholar]
[9]. Yu CH, Tsai TC, Wang JT, Liu BY, Wang YP, Sun A, Oral verruciform xanthoma: a clinicopathologic study of 15 casesJ Formos Med Assoc 2007 106:141-47. [Google Scholar]