A Rare Case of Orbital Apex Syndrome in Herpes Zoster Ophthalmicus
Charudutt Kalamkar1, Nishant Radke2, Amrita Mukherjee3, Snehal Radke4
1 Consultant Ophthalmologist, Department of Neuro-ophthalmology, Orbit and Oculoplasty, Shri Ganesh Vinayak Eye Hospital, Raipur, Chhattisgarh, India.
2 Consultant Ophthalmologist, Department of Retina and Vitreous, Shri Ganesh Vinayak Eye Hospital, Raipur, Chhattisgarh, India.
3 Consultant Ophthalmologist, Department of Anterior Segment, Shri Ganesh Vinayak Eye Hospital, Raipur, Chhattisgarh, India.
4 Consultant Ophthalmologist, Department of Anterior Segment, Shri Ganesh Vinayak Eye Hospital, Raipur, Chhattisgarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Charudutt Kalamkar, Consultant Ophthalmologist, Shri Ganesh Vinayak Eye Hospital, Opposite Colors Mall, Pachpedi Naka, Raipur, Chhattisgarh-492001, India.
E-mail: charudutt03@yahoo.co.in
Orbital Apex Syndrome (OAS) is a rare complication of Herpes Zoster Ophthalmicus (HZO). We are reporting a case of 65-year-old male who developed OAS following HZO. Patient presented with vesicular rash in the typical dermatomal distribution, severe periocular congestion and limited ocular motility in all gazes along with loss of vision. Soft tissue inflammation improved within 4 weeks of initiation of treatment while ocular motility slowly improved over 3 months. Patient did not gain vision despite receiving systemic steroids and systemic anti-viral medication. Variable improvement in ocular motility and visual function in our patient points towards multiple mechanisms involved in pathogenesis of this disease, some of which are yet to be understood.
Antiviral, Methylprednisolone, Ophthalmoplegia, Orbital Apex Syndrome
Case Report
A 65-year-old male presented with a 10 day history of swelling of upper and lower lids of right eye with blurring of vision and pain. He had vesicular rash on tip and side of nose.
Examination revealed vesicular rash on tip and side of nose which was resolving and had started to crust. There was severe periocular congestion, conjunctival chemosis with ptosis. Ocular motility was limited in all gazes indicating total external ophthalmoplegia [Table/Fig-1a]. Best Corrected Visual Acuity (BCVA) was Perception of Light (PL) positive with Inaccurate Projection of Rays (PR) in right eye and 20/200 in left eye.
(a): Clinical picture of patient with rash on tip and side of nose which is resolving and started to crust. Severe periocular congestion, conjunctival chemosis with ptosis. Ocular motility is limited in all gazes. (b): 3 months post treatment image of patient with resolved inflammation, improved ocular motility and ptosis.

Right eye slit-lamp examination revealed superficial punctate keratitis, anterior uveitis (Anterior Chamber cells and fresh keratic precipitates) and senile cataract. Corneal sensations were diminished. Relative Afferent Pupillary Defect (RAPD) was present in the right eye. Intraocular Pressure (IOP) was not possible due to severe lid congestion at initial examination. Fundus examination showed a myopic disc with peripapillary atrophy and chorio-retinal degeneration. There were no signs of inflammation in the posterior segment. Left eye had a normal anterior segment other than senile cataract. Left eye posterior segment also revealed a myopic fundus.
Blood investigations were within normal range (complete blood count, ESR). ELISA for HIV was negative.
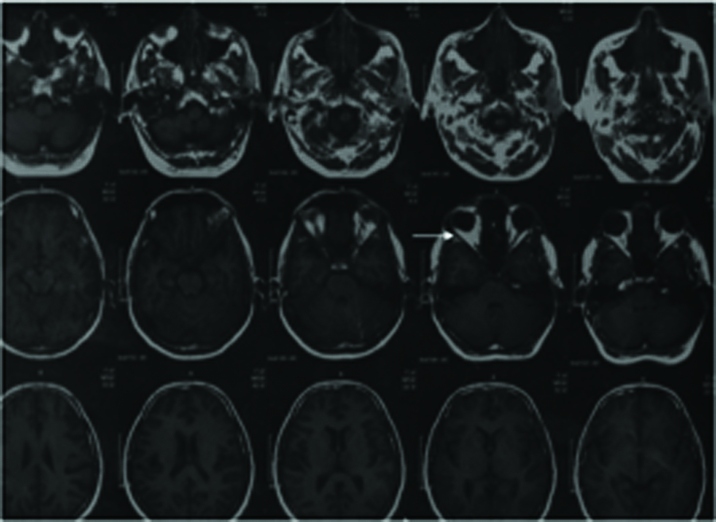
Magnetic Resonance Scanning (MRS) revealed enhancing soft tissue thickening of right eye periocular tissue with oedema of muscle cone but no enhancement of optic nerve in retro-bulbar or intraorbital region [Table/Fig-2]. Visual Evoked Potential (VEP) was done and showed extinguished response in right eye.
MRI showing enhancement of right eye extraocular muscles and soft tissues (Arrow), but no enhancement of optic nerve in retro-bulbar or intraorbital region.
Based on the presence of vesicular rash in typical location with total external ophthalmoplegia and optic nerve involvement, diagnosis of Herpes Zoster Ophthalmicus (HZO) with Orbital Apex Syndrome (OAS) was made.
Patient was admitted and started on injection I.V. Methylprednisolone (1 gm per day for 3 days) along with oral acyclovir 800mg 5 times per day. Acyclovir ointment and cycloplegics were also started topically. After 3 days of I.V. Methylprednisolone, oral steroids were started and slowly tapered over 2 months.
On day 2, patient developed an epithelial defect (dimensions being 3mm by 4mm) which healed by day 5. By 7th day anterior chamber reaction resolved and cornea cleared. Lid oedema and conjunctival chemosis significantly reduced by the end of 1st week of starting treatment. Ptosis resolved completely by day 14. Ocular motility started improving after 1st week and by the end of 3rd month movements were normal in all directions except abduction. Vision did not improve from light perception and RAPD persisted.
At 6 months follow-up, patient had regained ocular motility in all directions except minimal limitation of abduction. Right eye vision was still PL with inaccurate PR. Fundus examination revealed optic atrophy [Table/Fig-1b].
Discussion
HZO causes varied ocular manifestations following reactivation of latent varicella zoster virus (VZV). Ophthalmoplegia with involvement of 3rd, 4th, ophthalmic division of 5th and 6th cranial nerves has been documented in 3.5-10.1% of HZO cases but orbital apex syndrome is a rare complication [1,2]. OAS is associated with optic nerve involvement along with ophthalmoplegia. Good visual prognosis has been reported in literature for immunocompetent patients after receiving systemic steroids and antivirals [3–8]. We report an immunocompetent patient with OAS secondary to HZO, whose visual functions did not improve despite receiving treatment.
HZO commonly causes conjunctivitis, dermatitis, keratitis, anterior uveitis and secondary glaucoma. Orbital apex syndrome is a known but rare complication of this infection [1,2].
In previous studies, most patients were of elderly age group (>60 years), with only 1 case of an immune-deficient 29-year-old being reported [9]. In our case the presentation was severe inspite the fact that patient was immune-competent. Patient had Involvement of 2nd, 3rd, 4th, 5th and 6th cranial nerves along with periocular soft tissue inflammation and myositis. Dermatomal involvement was minimal as compared to the ocular symptoms emphasizing the fact that severity of skin involvement does not correlate well with severity of ophthalmic involvement. Hence even a single HZO skin lesion in nasociliary dermatome should alert the treating ophthalmologist.
Quick resolution of inflammatory signs on starting systemic steroids points towards immune mediated mechanism of damage rather than infectious. As other cases in literature have shown, HZO with orbital apex involvement responds to treatment with systemic antivirals and systemic steroids leading to resolution of nerve palsies [3–8]. In most reported cases of HZO induced optic neuritis in immune-competent patients, patient regained vision after treatment, though anisocoria may persist. In our case adduction and ptosis resolved but abduction deficit persisted. Residual deficits in extraocular motility have been reported in literature [7–10]. Also, the optic nerve function did not improve. Non improvement of vision in our case inspite of starting systemic steroids could have been due to the fact that treatment was started after 7 days of initial symptoms. Treatment started within 72 hours of the onset of rash gives the best possible outcomes. Apart from the inflammation, ocular ischemia has also been postulated to contribute to the optic nerve dysfunction, which may also explain the non-resolution of optic nerve dysfunction [7]. Soft tissue oedema causing compressive effect and direct infiltration of nerves by virus have also been postulated as mechanisms of ophthalmoplegia by Arda et al., [11]. MRI showing non-enhancement of optic nerve points towards this mechanism in our case. Similar findings of non-improvement of visual acuity has been documented by Shirao et al., and Dhingra et al., [10,12]. In most other cases optic neuritis resolved after treatment.
Duration of steroid treatment varies in literature from 14 days to 6 months. Duration to resolution of symptoms and signs also varies from as early as 3 days to 6 months [3–5,7,8,10]. In our patient improvement in symptoms began within 7 days of starting treatment and maximum recovery occurred in the first 3 months. Similar to our case, in most other reported cases, ophthalmoplegia and optic nerve involvement started with in the first 2 weeks after onset of rash [3–5,8,10].
Conclusion
Orbital apex syndrome is a rare but severe complication of HZO and can occur in immune-competent patients. Treatment with systemic antivirals and steroids should preferably be started within 72 hours of onset of rash. Delay in initiation of treatment may lead to residual deficits in ocular motility and visual functions. Pathogenesis of optic nerve dysfunction needs to be evaluated further.
[1]. Womack LW, Liesegang TJ, Complications of herpes zoster ophthalmicusArch Ophthalmol 1983 101(1):42-45. [Google Scholar]
[2]. Marsh RJ, Cooper M, Ophthalmic herpes zosterEye (Lond) 1993 7(Pt 3):350-70. [Google Scholar]
[3]. Kattah JC, Kennerdell JS, Orbital apex syndrome secondary to herpes zoster ophthalmicusAm J Ophthalmol 1978 85(3):378-82. [Google Scholar]
[4]. Krasnianski M, Sievert M, Bau V, External ophthalmoplegia due to ocular myositis in a patient with ophthalmic herpes zosterNeuromuscul Disord 2004 14(7):438-41. [Google Scholar]
[5]. Bourke RD, Pyle J, Herpes zoster ophthalmicus and the orbital apex syndromeAust N Z J Ophthalmol 1994 22(1):77-80. [Google Scholar]
[6]. Baha Ali T, Moutaouakil A, Ouaggag B, Khoumiri R, Orbital apex syndrome secondary to herpes zoster infection. A case reportBull Soc Belge Ophtalmol 2008 307:39-43. [Google Scholar]
[7]. Kurimoto T, Tonari M, Ishizaki N, Monta M, Hirata S, Oku H, Orbital apex syndrome associated with herpes zoster ophthalmicusClin Ophthalmol 2011 5:1603-08. [Google Scholar]
[8]. Lee C, Tsai H, Lee SS, Chen Y, Orbital apex syndrome: an unusual complication of herpes zoster ophthalmicusBMC Infectious diseases 2015 15:33 [Google Scholar]
[9]. Saxena R, Phuljhele S, Aalok L, Sinha A, Menon V, Sharma P, A rare case of orbital apex syndrome with herpes zoster ophthalmicus in a human immunodeficiency virus-positive patientIndian J Ophthalmol 2010 58(6):527-30. [Google Scholar]
[10]. Shirato S, Oshitari T, Hanawa K, Adachi-Usami E, Magnetic resonance imaging in case of cortical apex syndrome caused by varicella zoster virusOpen Ophthalmol J 2008 2:109-11. [Google Scholar]
[11]. Arda H, Mirza E, Gumus K, Oner A, Karakucuk S, Sırakaya E, Orbital apex syndrome in herpes zoster ophthalmicusCase Rep Ophthalmol Med 2012 2012:1-4. [Google Scholar]
[12]. Dhingra S, Williams G, Pearson A, Severe permanent orbital disease in herpes zoster ophthalmicusOrbit 2008 27(4):325-27. [Google Scholar]