Herpes Zoster Infection Involving Mandibular Division of Trigeminal Nerve and Ramsay Hunt Syndrome with Meningitis in an Immunocompetent Patient: A Rare Association
Vijayan Ganesan1, Dhrubajyoti Bandyopadhyay2, Suvrendu Sankar Kar3, Cankatika Choudhury4, Vivek Choudhary5
1 Post Graduate Trainee, Department of Internal Medicine, RG Kar Medical College, Kolkata, India.
2 Senior Resident, Department of Accident and Emergency, Lady Hardinge Medical College, New Delhi, India.
3 Assistant Professor, Department of Internal Medicine, RG Kar Medical College, Kolkata, India.
4 Post Graduate Trainee, Department of Internal Medicine, RG Kar Medical College, Kolkata, India.
5 Post Graduate Trainee, Department of Internal Medicine, RG Kar Medical College, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dhrubajyoti Bandyopadhyay, Senior Resident, Department of Accident and Emergency, Lady Hardinge Medical College, New Delhi-110001, India. Email- drdhrubajyoti87@gmail.com
Herpes zoster is a unilateral painful vesicular cutaneous eruption caused by the reactivation of the Varicella zoster virus. It commonly affects the older people and immunocompromised individuals. The dermatomes from T3 to L3 are most frequently involved. Its three stages include prodromal stage, active stage and chronic stage. The common complications of the infection include post-herpetic neuralgia, Ramsay Hunt syndrome, Guillain-Barre syndrome, transverse myelitis and encephalomyelitis. This case report summarizes a very rare association of herpes zoster meningitis with the involvement of mandibular division of the trigeminal nerve and facial nerve. The patient improved with intravenous acyclovir and prednisolone treatment.
Painful vesicles, Post-herpetic neuralgia, Vesicular cutaneous eruption
Case Report
A 70-year-old non-diabetic, non-hypertensive female presented to the Department of Medicine with continuous high-grade fever, headache, projectile vomiting, neck pain, photophobia and skin rashes over the right half of the face for four days. She gave history of burning sensation over the right half of the face five days preceding the illness. She had history significant for chicken pox in her late twenties. On examination she was febrile (temperature 101 °F), with pulse rate 116/min, BP- 106/74 mm Hg and respiratory rate 20/min. She had neck rigidity and positive Kernig’s and Brudzinski’s sign. She had tender, multiple, erythematous vesicles with few pustules on the right cheek, chin and in and around the right ear [Table/Fig-1,2]. She had multiple ruptured vesicles, which coalesced to form large ulcers on the right half of the tongue, right half of the lower lip, buccal mucosa, lower labial mucosa, and right sided peri-orbital oedema [Table/Fig-3]. She had right lower motor neuron (LMN) facial nerve palsy as evident by an inability to close her right eye forcefully, deviation of the angle of mouth to the left side and decreased wrinkles in the right half of the forehead [Table/Fig-4]. Written informed consent was taken from the patient for publication of images.
Multiple, erythematous vesicles with few pustules over the right cheek, chin.

Erythematous lesions and vesicles around the right ear.

Multiple coalescent ulcers on the right half of tongue with candidiasis on the left half.

Right sided lower motor neuron type facial nerve palsy.

Initial Treatment
The patient initially was administered intravenous ceftriaxone (2gm/day), vancomycin (1gm 12 hourly), ampicillin (2gm every 6h), acyclovir and steroids (dexamethasone 10 mg IV every 6 hours).
Investigations
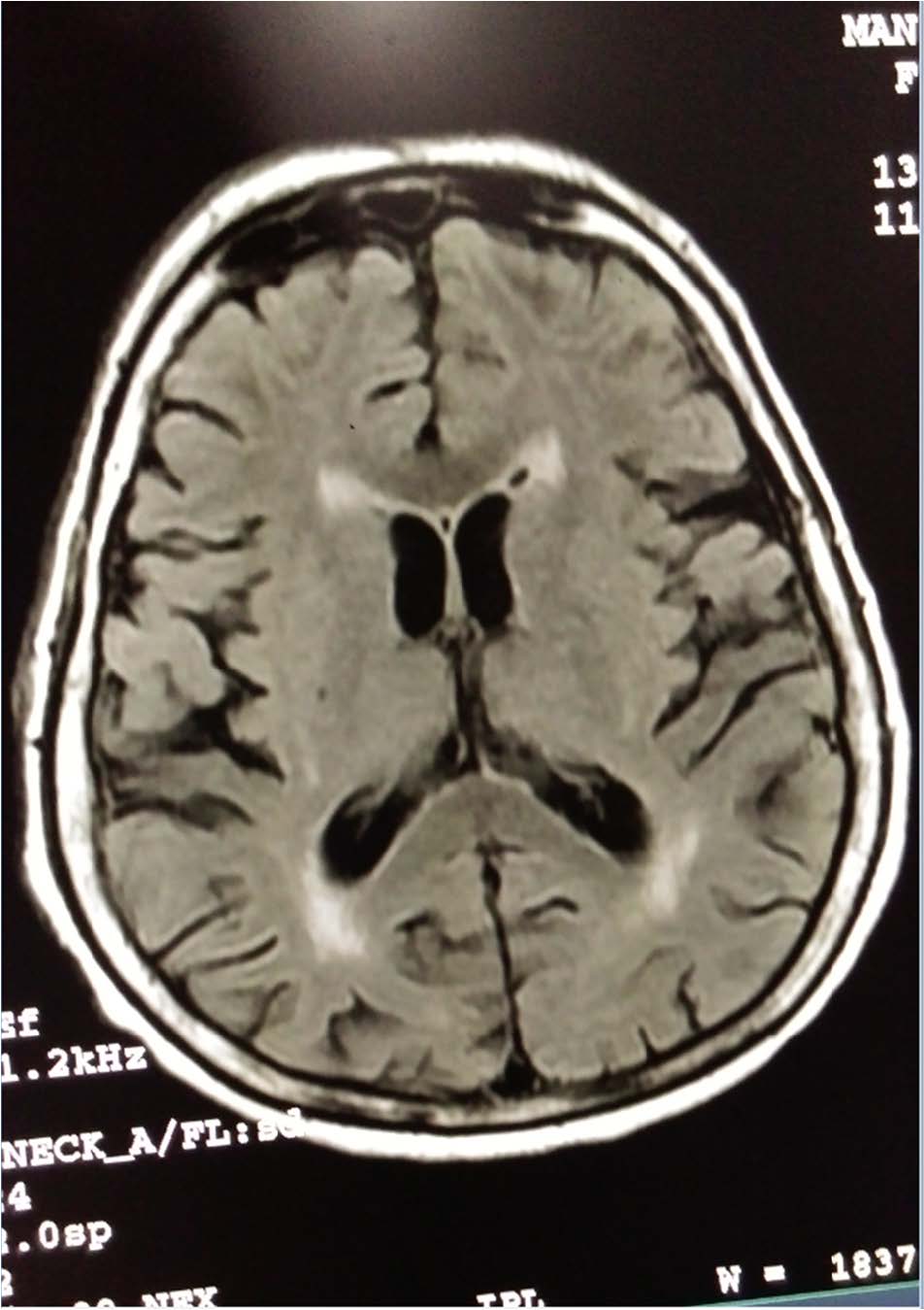
Routine blood investigations revealed a Haemoglobin-12gm%, WBC count of 13000/cmm with lymphocytes 55%, neutrophils 42%, and monocytes 3%. Blood parameters like urea (Ur), creatinine (Cr), sodium (Na), potassium (K), fasting blood sugar (FBS) and postprandial blood sugar (PPBS) were normal. Anti-HIV 1 and 2 antibody were negative. CSF report showed cell count - 50cmm (all lymphocytes), protein-90 mg/dl, sugar-63 mg/dl. Culture for bacteria in the CSF was negative. The presence of VZV IgM antibody in CSF by immunofluorescence assay and positive CSF Polymerase Chain Reaction (PCR) for VZV DNA confirmed VZV infection. The electroencephalogram, CT brain, and contrast-enhanced MRI brain didn’t reveal any abnormality [Table/Fig-5].
MRI brain showing no significant abnormality.
Follow-up
Injection ceftriaxone, vancomycin, and ampicillin were omitted. Injection acyclovir (10 mg/kg three times daily) and corticosteroid were continued for two weeks. She was also given Tramadol hydrochloride injection (50mg) for severe pain. Neck rigidity was improved on the fourth day, with peripheral WBC count dropping down to 9400/cmm. The right sided periorbital oedema subsided, and skin lesions started to crust. CSF study was repeated after two weeks and revealed cell count 15/cmm, protein 47 mg/dl and sugar 62 mg/dl.
Discussion
Herpes zoster infection may affect any sensory ganglia and its cutaneous nerve. The T3-L2 dermatome is affected most commonly and about 13% of patients present with the disease involving any of the three branches of the trigeminal nerve. The 1st division of the trigeminal nerve is commonly affected, whereas the 2nd and the 3rd divisions are rarely involved [1]. Involvement of the mandibular branch (V3) of the trigeminal nerve are localized to the lateral head, external ear, external auditory meatus, lower lip, lip mucosa, mandibular gums and lateral neck [2].
Patients with Herpes zoster infection usually progress through three stages: 1) prodromal stage; 2) active (eruptive) stage); 3) chronic stage [3]. In most patients a two-three day primary acute or pre-eruptive phase with pain, burning or tingling in the involved dermatome believed to represent the viral degeneration of the nerve fibrils [4]. The eruptive phase is characterized by erythematous macules, papules, vesicle and bullae formation with unilateral dermatomal distribution. The recurrent meningeal branch (Arnold’s nerve) involvement may lead to meningeal irritation [5].
The chronic stage is often seen in 10% of all patients in Herpes zoster, and it is termed as post-herpetic neuralgia. It is defined as a sharp, recurrent shooting, deep pain remaining for over a month or 3 months after the healing of the mucocutaneous lesions. The risk of occurrence of postherpetic neuralgia increases significantly after 60 years may be due to decline in cell-mediated immunity [6].
Approximately 12% of all peripheral facial nerve palsies are caused by VZV. Pain in the affected area develops before a vesicular rash in 14-50% of VZV patients [7]. The rate of full recovery is around 67.7% in RHS, but only 27.3% of patients with multiple cranial nerve involvement [7]. Although our patient had improved dramatically, concomitant diseases such as diabetes and chronic renal failure might lead to an aggressive course.
Skin manifestations in some situations may suggest the cause of aseptic meningitis. Examples include a vesicular rash of varicella zoster, the genital lesions of HSV-2, or a mild maculopapular rash occurring in summer and fall months with some enteroviruses [8].
Enterovirus infection is the most common cause of viral meningitis in the immunocompetent adult. The reactivation zoster rash of VZV is very rarely associated with aseptic meningitis. VZV infection should be considered as one of the possibilities if a patient presents with CNS disease without rash [8]. PCR may help to clinch the diagnosis the diagnosis in the absence of the cutaneous eruption.
No published data is revealing significant benefit of acyclovir therapy in VZV meningitis. But if a zoster rash is found, it is important to consider the early initiation of antiviral therapy. We should consider the use of steroids which helps to repress the inflammation process and alleviates oedema, thereby decreasing pain and preventing neuralgia after herpes zoster. The use of corticosteroids without antiviral therapy is not recommended [8]. In a study by Kinishi and colleagues, 91 Ramsay Hunt syndrome patients were treated with acyclovir and corticosteroids compared to 47 patients treated with corticosteroids alone. Improvement seen in 82 of the 91 patients (90%) treated with both acyclovir and corticosteroids compared to 30 of the 47 patients (64%) treated with corticosteroids alone [9]. The timing of initiation of treatment was the most crucial factor in early recovery. The highest rate of recovery was seen when treatment was initiated within three days of onset of symptoms.
Varicella-zoster vaccination is now a part of children vaccination program in the US and the incidence of chickenpox, herpes zoster (HZ) and sequelae has reduced dramatically. Reduction of the incidence of HZ and post-herpetic pain of more than 50% has been shown in person 60 years age or older by vaccination [7].
Herpes zoster infection in our case has involved the right mandibular division of the trigeminal nerve and the facial nerve (Ramsay Hunt Syndrome) with meningitis. VZV meningitis with the involvement of the mandibular division of the trigeminal nerve and Ramsay Hunt Syndrome is a very rare association. Vaccination against VZV is an interesting new development which has the potential to reduce the incidence of VZV-associated disease altogether. The effectiveness of the VZV vaccine and its outcome in Ramsay Hunt syndrome are needed to be studied further.
Conclusion
Herpes Zoster virus infection should be considered during the evaluation of a patient with meningitis and cutaneous vesicular eruption. Meticulous examination of other cranial nerves in a patient with viral meningitis is necessary. Early institution of antiviral and steroid are the most important factors in determining the prognosis of such patients.
[1]. Carbone V, Leonardi A, Pavese M, Raviola E, Giordano M, Herpes zoster of the trigeminal nerve: a case report and review of the literatureMinerva Stomatol 2004 53(1-2):49-59. [Google Scholar]
[2]. Eastern JS, Herpes ZostereMedicine September 18, 2006 [Google Scholar]
[3]. Carmichael JK, Treatment of herpes zoster and postherpetic neuralgiaAm Fam Physician 1991 44:203-10. [Google Scholar]
[4]. Tidwell E, Hudson B, Bukhart N, Gutmann JL, Ellis CD, Herpes zoster of the trigeminal nerve branch: a case report and review of literatureInt Endod J 1999 32:61-66. [Google Scholar]
[5]. Makos C, Noussios G, Peios M, Balabanis G, Evangelinou C, Herpes Zoster Of The Trigeminal Nerve-Two Cases ReportsThe Internet Journal of Neurology 2010 13(2) [Google Scholar]
[6]. Mac Farlane LL, Simmons MM, Hunter MH, The use of corticosteroids in the management of Herpes zoster in children and adolescentsPaedInf Dis J 1998 17:905-08. [Google Scholar]
[7]. Rasmussen Virology Discovery 2014 2:1DOI : 10.7243/2052-6202-21 [Google Scholar]
[8]. Cooper CJ, Said S, Teleb M, Rosa P, Didia SC, An immunocompetent patient with a vesicular rash and neurological symptomatologyCase Reports in Medicine 2013 doi:10.1155/2013/168943 [Google Scholar]
[9]. Kinishi M, Amatsu M, Mohri M, Saito M, Hasegawa T, Hasegawa S, Acyclovir improves recovery rate of facial nerve palsy in Ramsay Hunt syndromeAuris Nasus Larynx 2001 28:223-26. [Google Scholar]