Diseases of pancreas have a very variable presentation and imaging plays an important role in the diagnosis and management of pancreatic diseases. Modalities for imaging pancreas range from plain x-ray to Ultrasonography (USG), endoscopic ultrasound, Endoscopic Retrograde Cholangiopancreaticography (ERCP), Computed Tomography (CT), Magnetic Resonance Imaging (MRI), Magnetic Resonance Cholangiopancreaticography (MRCP). Computed Tomography (CT) is highly accurate, and sensitive than USG in both diagnosing as well as demonstrating the extent [1]. CT is a key diagnostic tool in understanding the cause of endocrine and exocrine pancreatic insufficiency in most patients. Pancreatitis is one of most complex and clinically challenging of all abdominal disorders [2].
As early treatment of patients with severe acute pancreatitis can reduce morbidity and mortality. Balthazar in 1990, created the CT Severity Index (CTSI) by combining the original grading system with the presence and extent of pancreatic necrosis. The combined score of CTSI proved to have a better prognostic accuracy than the Balthazar score but it, too, had some drawbacks. The score obtained with the index did not significantly correlate with the subsequent development of organ failure, extra pancreatic parenchymal complications or peripancreatic vascular complications [3,4]. In view of these limitations, a modified and simplified CT scoring system was hypothesized in 2004 by Mortele and colleagues so as to determine if the scores obtained with this could be used to predict the clinical outcome more accurately. The modified Mortele CTSI was easier to calculate and was found to correlate more closely with patient outcome measures like the length of the hospital stay, the need for surgery/intervention, and the occurrences of infection, organ failure and death than the currently accepted Balthazar CT severity index, with similar inter observer variability [5] The revised Atlanta classification system, introduced in 2012, better defined the clinical diagnosis, Computed Tomographic (CT) manifestations and disease course of acute pancreatitis into two morphologic subtypes [6]: Interstitial oedematous pancreatitis and Necrotizing pancreatitis
To assess the prognostic correlation of patient outcome with currently accepted Balthazar and the Modified Mortele Computed Tomography severity indices in acute pancreatitis.
Materials and Methods
It was a prospective study, conducted from November 2013 to November 2015, in the Department of Radio Diagnosis, People’s Hospital associated to People’s College of Medical Sciences and Research Centre, Bhanpur, Bhopal, India.
A total of 50 patients referred from the Department of Emergency Medicine and Department of Surgery, People’s Hospital associated with People’s College of Medical Sciences and Research Centre presented with the chief complaint of epigastric pain, nausea and vomiting and CECT abdomen were suggestive of acute pancreatitis were included in this study.
Assessment of Severity
Assessment of severity of acute pancreatitis was done in all cases by Balthazar CTSI scoring [3] and Mortele Modified [7] CTSI scoring.
Each case was assigned a CT grade from A to E and awarded points from 0-4 as in [Table/Fig-1].
| Grade A: | Normal pancreas | 0 Point |
| Grade B: | Focal or diffuse enlargement of the pancreas (including contour irregularities, non- homogenous attenuation of the gland, dilation of the pancreatic duct and foci of small fluid collections within the gland, as long as there was no evidence of peri-pancreatic disease. | 1 Point |
| Grade C: | Intrinsic pancreatic abnormalities associated with hazy streaky densities representing inflammatory changes in the peri-pancreatic fat. | 2 Point |
| Grade D: | Single ill defined fluid collection (phlegmon). | 3 Point |
| Grade E: | Two or multiple, poorly defined fluid collections or presence of gas in or adjacent to the pancreas. | 4 Point |
The presence and extent of necrosis in each case was classified into four categories and awarded points from 0-6 as follows:
| Necrosis absent | 0 Points |
| < 30% necrosis | 2 Points |
| 30-50% | 4 Points |
| > 50% necrosis | 6 Points |
The Balthazar CTSI was calculated by adding the above points in each case and the total score was then categorized as:
| Mild pancreatitis | CTSI score 0-3 |
| Moderate pancreatitis | CTSI score 4-6 |
| Severe pancreatitis | CTSI score 7-10 |
Mortele Modified CTSI Scoring
| Normal pancreas | 0 Point |
| Intrinsic pancreatic abnormalities with or without inflammatory changes in peripancreatic fat | 2 Points |
| Pancreatic or peripancreatic fluid collection or peripancreatic fat necrosis | 4 point |
The presence and extent of necrosis in each case was scored from 0-4 as follows:
| Necrosis absent | 0 Points |
| < 30% necrosis | 2 Points |
| > 30% necrosis | 4 points |
To the above score, 2 points were added for the presence of extrapancreatic findings.
The Modified CTSI was calculated by summing these values and the total score was then categorized as:
| Mild pancreatitis | Modified CTSI score 0-2 |
| Moderate pancreatitis | Modified CTSI score 4-6 |
| Severe pancreatitis | Modified CTSI score 8-10 |
The severity is classified into three categories based on clinical and morphologic findings according to revised Atlanta classification [8]
Mild – No organ failure and no local or systemic complications.
Moderate – Presence of transient organ failure less than 48h and/or presence of local complications.
Severe – Persistent organ failure > 48 hour.
Outcome Parameters
Clinical follow-up of the patients was done in terms of the following parameters:
Length of hospital stay.
Need for surgery or percutaneous intervention.
Evidence of infection in any organ system.
Occurrence of organ failure- respiratory, cardiovascular, renal, hepatic and haematological system.
Discharged/death.
The clinical outcome was compared with the currently accepted Balthazar’s CTSI and Modified Mortele’s CTSI in all the cases.
Method of data collection clinical diagnosis was based on the symptoms like upper abdominal pain, nausea, vomiting, fever and/or elevation of serum amylase three times the upper limit of normal (normal serum amylase 20-110 U/L).
Inclusion Criteria
Clinically suspected case of acute pancreatitis of all ages.
Exclusion Criteria
Patients with chronic pancreatitis suggested by intraductal calculi, ductal stricture and parenchymal calcification.
Other pancreatic pathology like pancreatic malignancy, cyst.
Any previous pancreatic surgery.
Contraindicated cases for contrast study.
Postoperative cases.
Pregnant females.
Equipments used in the study – Siemens Somatom Sensation mdct 40 slice and Mederton Inkjeterton CT2 (pressure injector).
Statistical Analysis
Data analysis was done using SPSS version 16.0 Data transformation by recoding, counting and cross tabulation was performed and obtained information was processed using Pearson chi-square and Fisher’s-exact test.
Results
Symptoms and signs in patients of acute pancreatitis: Triad of epigastric pain, nausea and vomiting was present in 75% of patients.
Findings in patients of acute pancreatitis: Most common CT findings were peri-pancreatic inflammatory changes in mesentery, greater omentum and transverse mesocolon (88%). Second most common CT finding was pancreatic contour irregularity (80%). Twenty five patients (50%) had necrosis of the pancreas with 14 of them having > 50% necrosis.
Gall stone disease was most common aetiological factor seen; it was more common in females than males. Alcohol was second most common aetiological factor and was noted only in males [Table/Fig-2].
Aetiology of acute pancreatitis.
| Causes | Total | Male | Female |
|---|
| No. of cases | % | No. of cases | % | No. of cases | % |
|---|
| Gall stones | 20 | 40 | 8 | 38 | 12 | 62 |
| Alcohol | 19 | 38 | 19 | 100 | 0 | 0 |
| Trauma | 1 | 2 | 0 | 00 | 1 | 100 |
| Drug induced | 1 | 2 | 0 | 0 | 1 | 100 |
| Idiopathic | 11 | 24 | 8 | 75 | 3 | 25 |
Pleural effusion was the most common extra-pancreatic complication with left pleural effusion being the more common. Isolated right pleural effusion was not seen [Table/Fig-3].
Extra pancreatic complications in patient of acute pancreatitis.
| Findings | No. of Cases | % |
|---|
| Extra pancreatic complications | 34 | 68 |
| Pleural fluid | 23 | 46 |
| • Left pleural effusion | 13 | 26 |
| • B/L pleural effusion | 10 | 20 |
| Ascites | 17 | 34 |
| Solid organ abnormality | 5 | 10 |
| • Infarction | 0 | 0 |
| • Haemorrhage | 0 | 0 |
| • Subcapsular fluid collection | 5 | 10 |
| Vascular complications | 4 | 8 |
| • Venous thrombosis | 4 | 8 |
| • Arterial haemorrhage | 0 | 0 |
| • Pseudoaneurysm formation | 0 | 0 |
| Inflammation of GIT | 12 | 24 |
| • Thickening of wall | 12 | 24 |
| • Intramural fluid collection | 0 | 0 |
Balthazar grading in patients with acute pancreatitis: Balthazar grade C was the most common (40%) followed by grade D and E (25% each).
Correlation of Balthazar grade with Degree of necrosis: Of the 25 (50%) patients, 6 had < 30%, 5 had 30-50% and 14 had > 50% pancreatic necrosis. No necrosis was noted in patients with grade B pancreatitis. Of the 20 patients with Grade C pancreatitis, 9 (45%) patients had gland necrosis with 6 patients having > 50% necrosis. Of the 13 patients with grade D pancreatitis, 7(54%) patients had parenchymal necrosis. Of the 13 patients with Grade E pancreatitis, 9(69%) patients had evidence of necrosis.
Acute peri pancreatic collection was the most common findings [Table/Fig-4].
The morphological classification according to Revised Atlanta classification.
| Acute peripancreatic collection | Acute necrotic collection | Pseudocyst | Walled off necrosis |
|---|
| 36 | 24 | 0 | 0 |
Majority of the cases were categorized as mild pancreatitis according Balthazar CTSI score [Table/Fig-5].
Grading severity of acute pancreatitis using Balthazar CTSI score.
| Severity | Score | No. of patients | % |
|---|
| Mild | 0-3 | 21 | 42 |
| Moderate | 4-6 | 12 | 24 |
| Severe | 7-10 | 17 | 34 |
| Total | | 50 | 100 |
Majority of the cases were categorized as severe pancreatitis using the Modified Mortele CTS score [Table/Fig-6].
Grading severity of acute pancreatitis using modified mortele CTSI.
| Severity | Score | No. of Cases | % |
|---|
| Mild | 0-2 | 9 | 18 |
| Moderate | 4-6 | 19 | 38 |
| Severe | 8-10 | 22 | 44 |
| Total | | 50 | 100 |
According to revised Atlanta classification majority of the cases were categorized as mild pancreatitis [Table/Fig-7].
Severity of acute pancreatitis according to revised Atlanta classification.
| Severity | Total no. of cases | Organ failure | No. of death |
|---|
| Mild | 42 | 0 | 0 |
| Moderate | 0 | 0 | 0 |
| Severe | 8 | 8 | 7 |
Intervention and length of stay was significantly more (p-value = 0.02 and 0.01 respectively) associated with moderate grade. Infection, organ system failure and death were significantly associated with severe grade [Table/Fig-8].
Patient outcome using currently accepted Balthazar CTSI.
| Outcome Parameter/ No. of patients | Total(n=50) | Mild(n=21) | Moderate(n=12) | Severe(n=17) |
|---|
| No. | % | No. | % | No. | % | No. | % |
|---|
| Average duration of hospital stay (in days) | | | 17 | | 25 | | 23 | |
| Intervention/drainage | 15 | 30 | 3 | 20 | 7 | 46.6 | 5 | 33.33 |
| Surgical debridement | 2 | 4 | 0 | 0 | 0 | 0 | 2 | 100 |
| Infection | 8 | 16 | 1 | 12.5 | 0 | 0 | 7 | 87.5 |
| Organ system failure | 8 | 16 | 1 | 12.5 | 1 | 12.5 | 6 | 75 |
| Death | 0 | 12 | 0 | 0 | 1 | 16.6 | 6 | 83.3 |
Average duration of hospital stay was significant more (p-value = 0.02) with severe grade. Infection, organ system failure and death were also significantly associated with severe grade [Table/Fig-9].
Patient outcome using modified Mortele CTSI.
| Outcome Parameter/ No. of patients | Total(n=50) | Mild(n=8) | Moderate(n=20) | Severe(n=22) |
|---|
| No. | % | No. | % | No. | % | No. | % |
|---|
| Average duration of hospital stay (in days) | | | 9 | | 22 | | 29 | |
| Intervention/drainage | 15 | 30 | 0 | 0 | 7 | 46.6 | 8 | 53.33 |
| Surgical debridement | 2 | 4 | 0 | 0 | 0 | 0 | 2 | 100 |
| Infection | 8 | 16 | 0 | 0 | 1 | 12.5 | 7 | 87.5 |
| Organ system failure | 8 | 16 | 0 | 0 | 1 | 12.5 | 7 | 87.5 |
| Death | 7 | 12 | 0 | 0 | 1 | 14.2 | 6 | 85 |
Organ failure, death seen in only severe category in revised Atlanta classification, moderate and severe category in modified Mortele CTSI, mild, moderate, severe category in Balthazar CTSI [Table/Fig-10]. Few illustrations of cases have been provided in [Table/Fig-11,12,13,14,15,16,17 and 18].
Comparison of outcome according to the currently accepted balthazar ctsi and mortele modified ctsi and revised atlanta classification (N=50).
| Grading System | Severity | Organ Failure | No of death |
|---|
| Balthazar CTSI | MildModerateSevere | 116 | 16 |
| Modified Mortele CTSI | MildModerateSevere | 017 | 016 |
| Revised Atlanta Classification | MildModerateSevere | 008 | 007 |
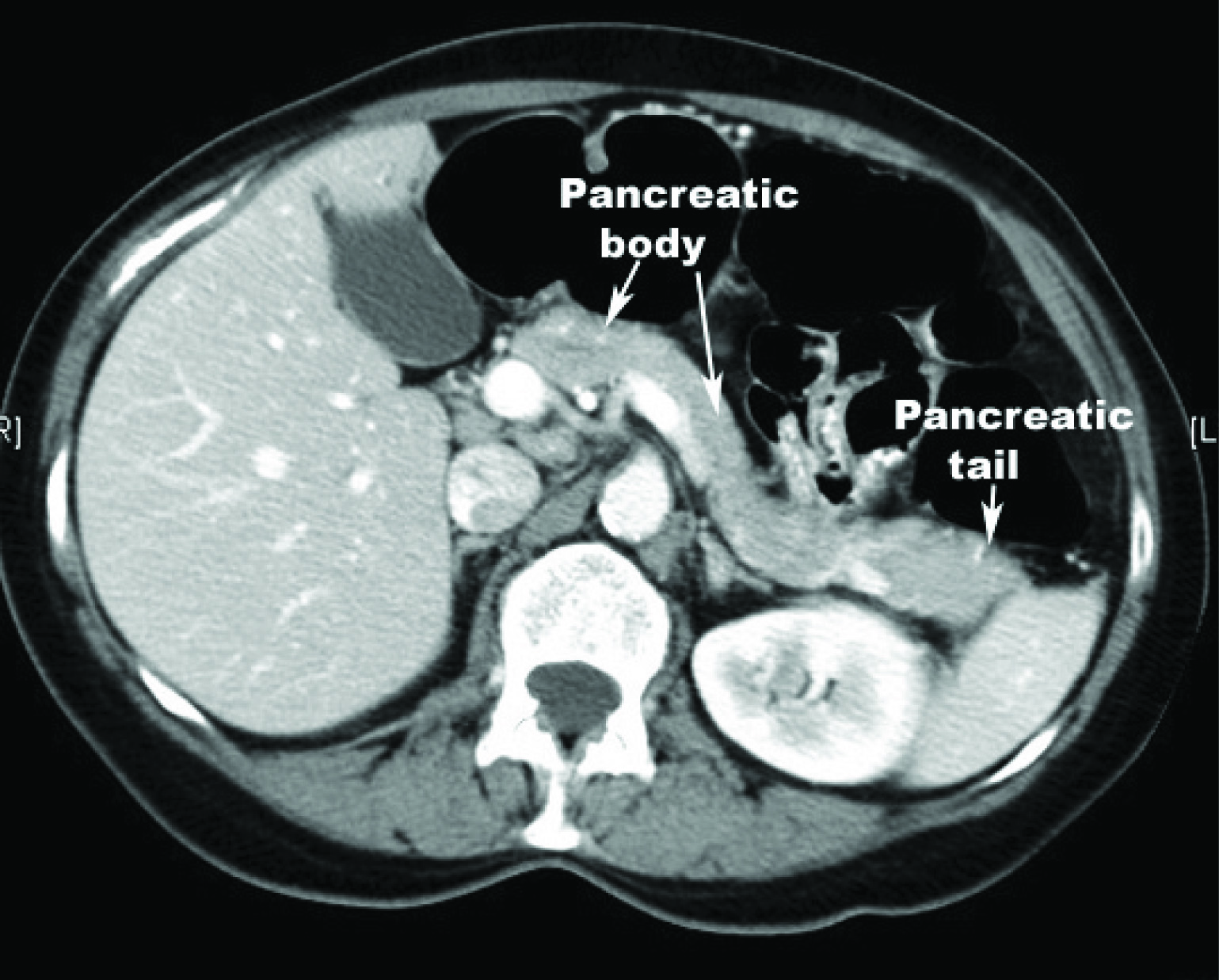
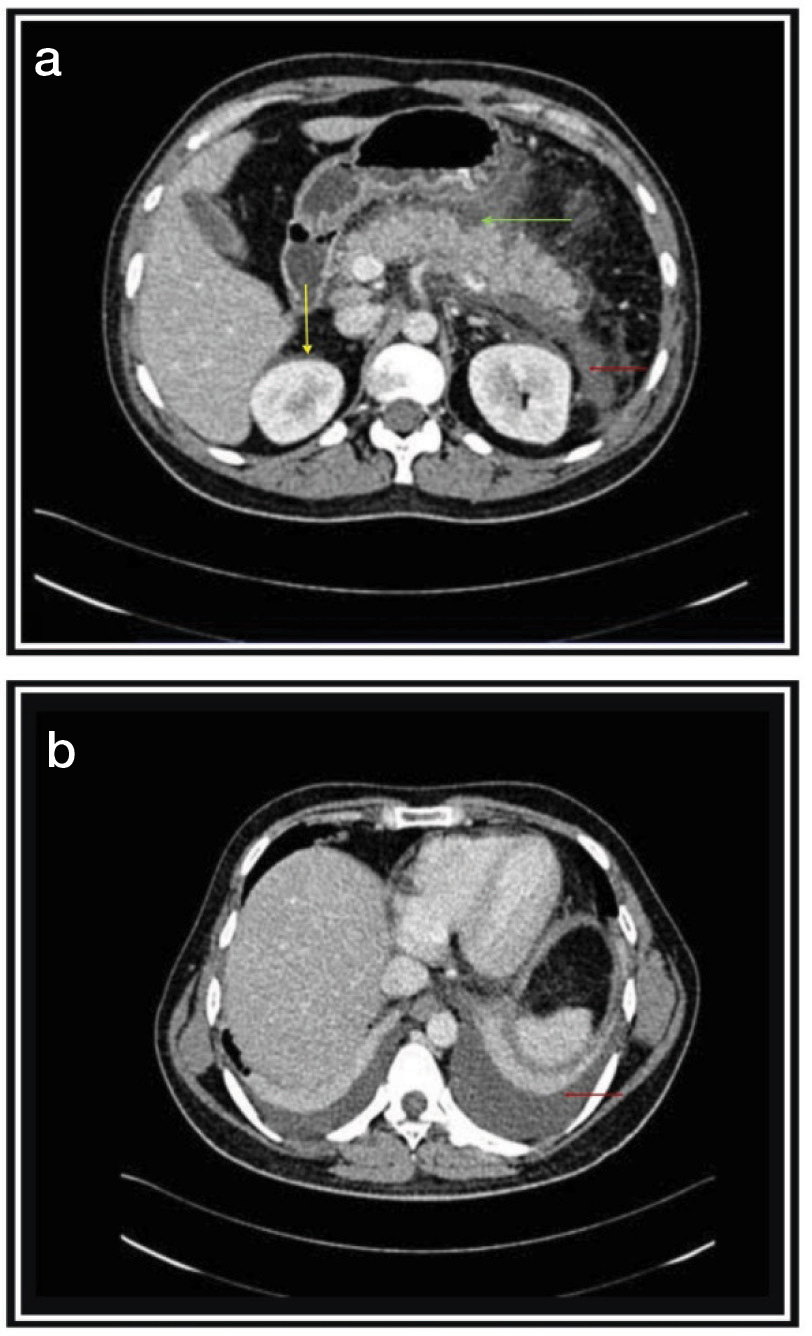
Axial CT image of abdomen reveals normal anatomy of Pancreas (arrows).
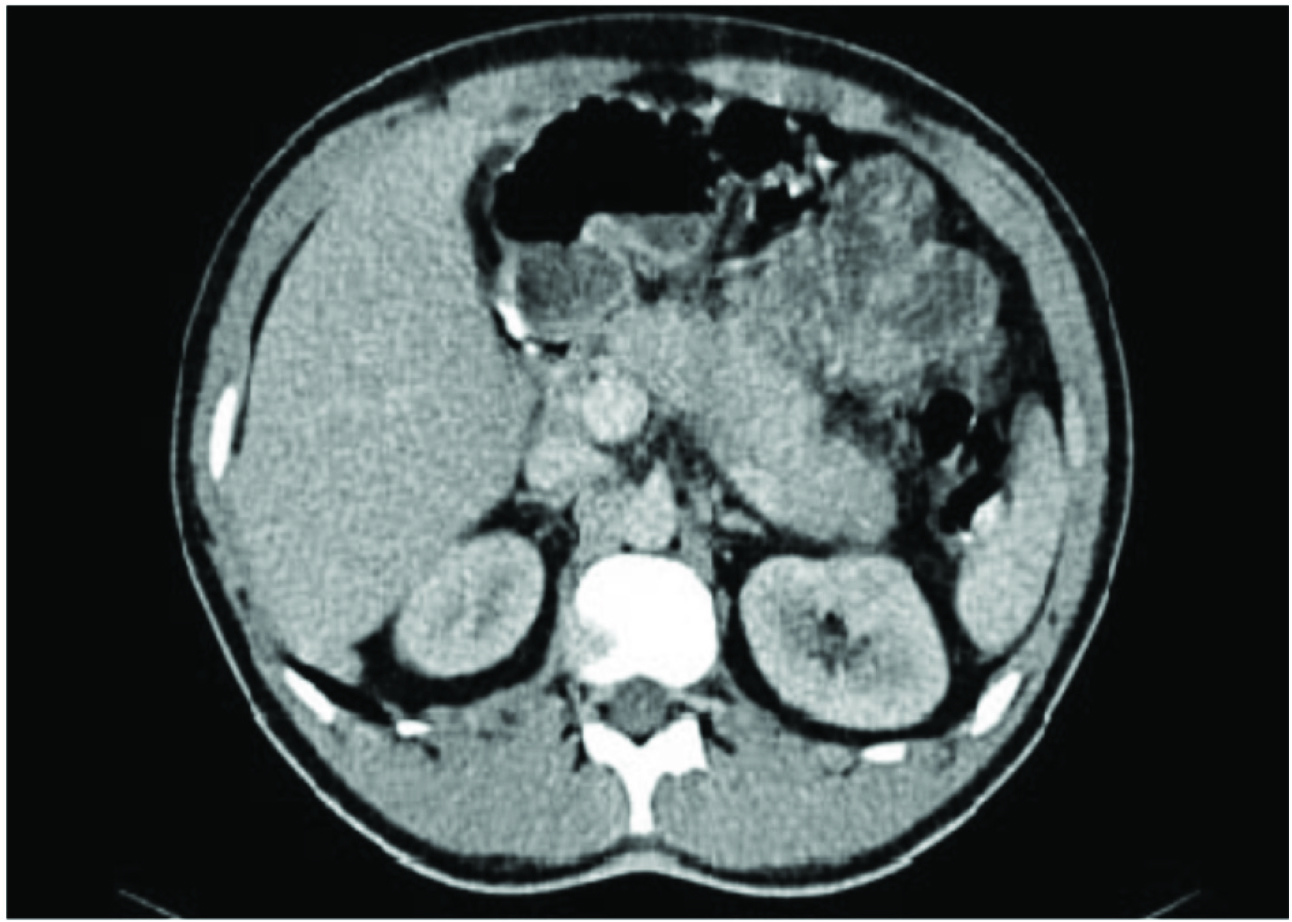
Bulky pancreas both Balthazar CTSI 1 and modified CTSI score 2 suggestive of mild pancreatitis.
(a) Bulky pancreas with heterogeneous enhancement; (b) Bulky pancreas with mild ascites (Red Arrow) both Balthazar and modified CTSI score 4 suggestive of moderate pancreatitis.
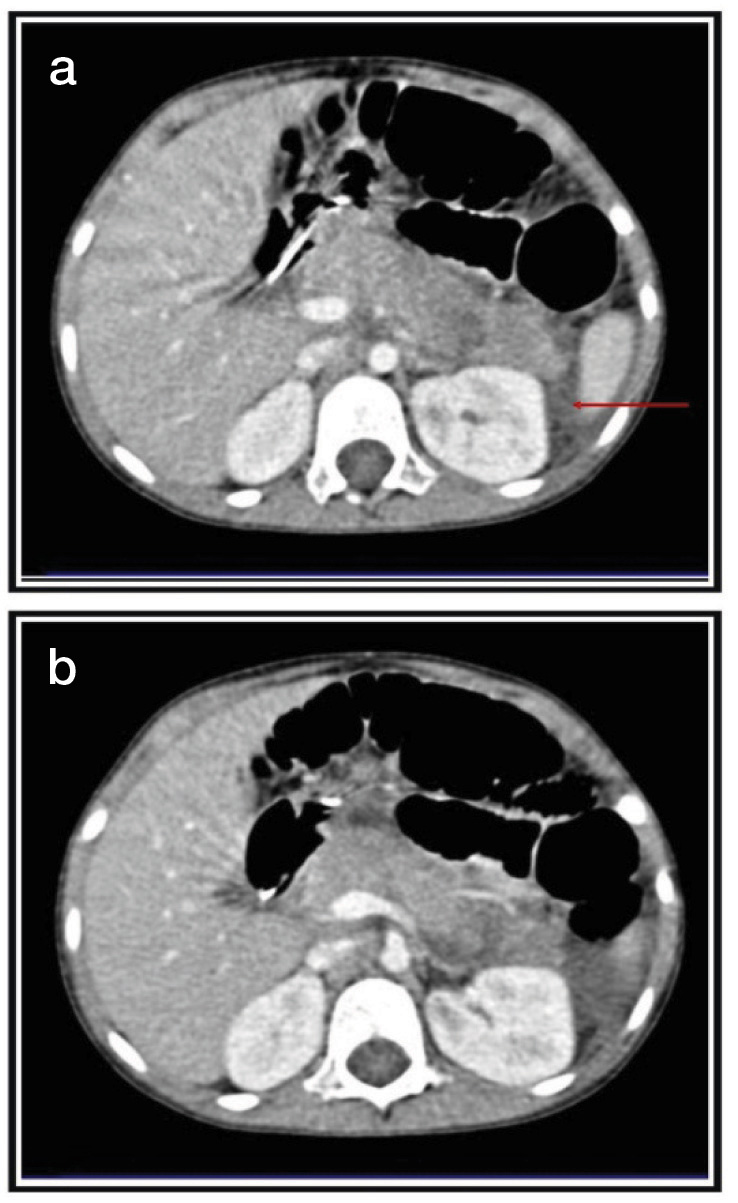
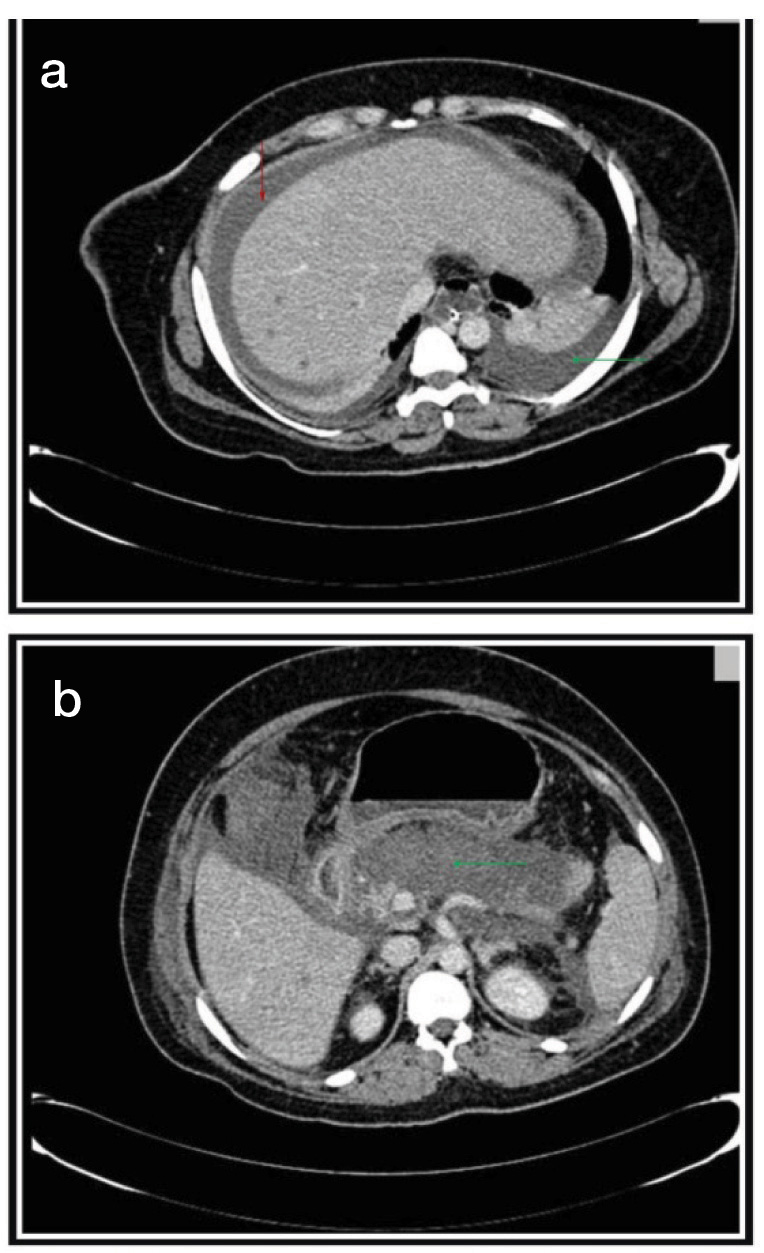
(a) Bulky, heterogeneous pancreas with peri pancreatic fat standing (red arrow) & few necrotic areas seen withing pancreas (<30%), (yellow arrow) and thickened gerota’s fascia (green arrow). (b) Minimal bilateral pleural collection and basal subsegmental atelectasis (red arrow) balthazar CTSI score 6 and modified CTSI scores 8 suggestive of intermediate and severe pancreatitis respectively.
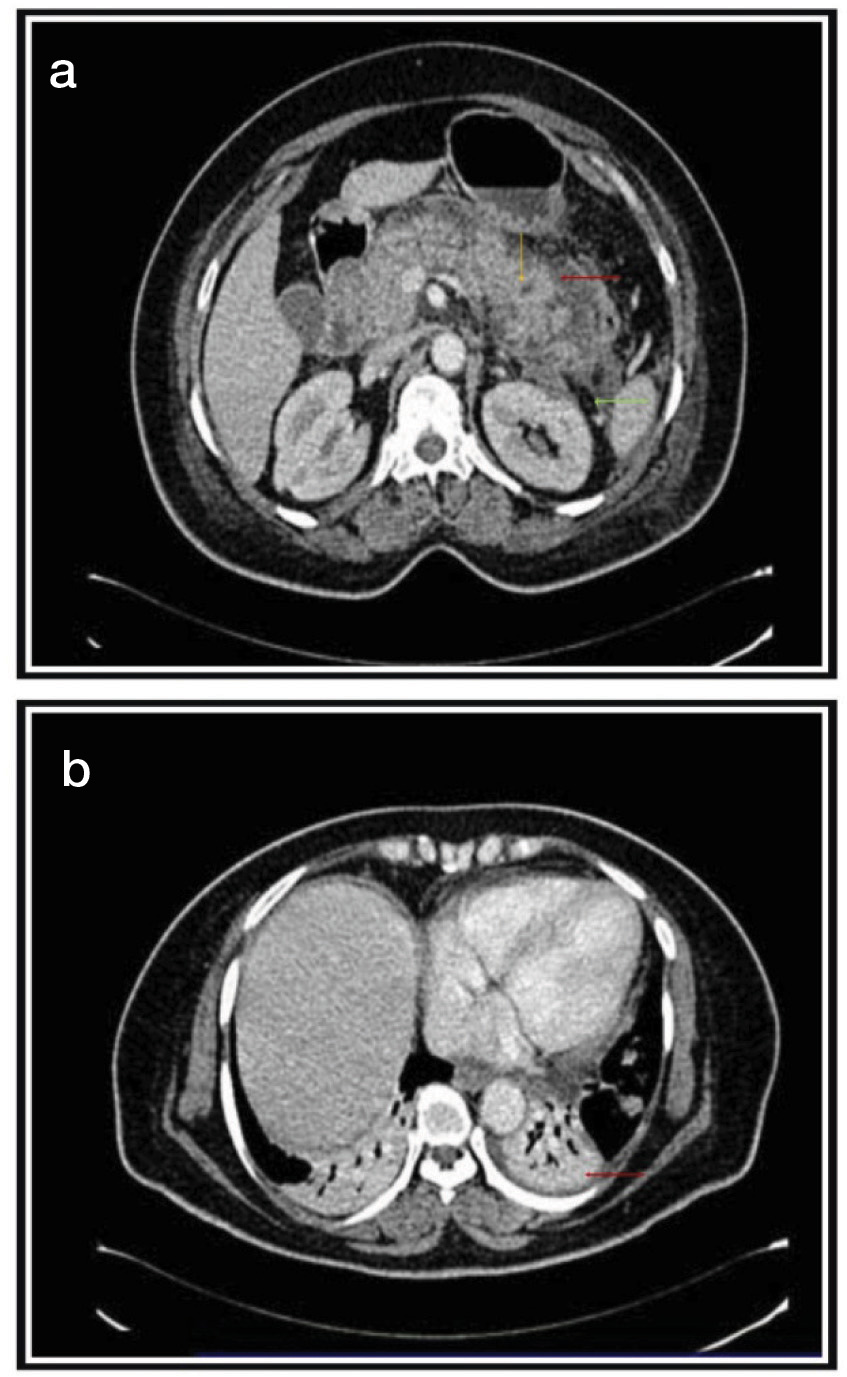
(a) Diffusely edematous pancreas with peripancreatic fat sranding (green arrow), fluid collection (yellow arrow) and perinephric fascial thickening (red arrow). (b) Bilateral pleural effusion and basal sub segmental atelectasis (red arrow) Balthazar CTSI score 5 and modified CTSI score 6 suggestive of intermediate and moderate pancreatitis respectively.
(a) Acute necrotising pancreatitis affecting >50% pancreas (red arrow). (b) Acute necrotising pancreatitis with peripancreatic fluid collection (green arrow) perinephric fascial thickening and ascites with cholelithiasis (red arrow) both Balthazar & modified CTSI score 10 suggestive of severe pancreatitis.
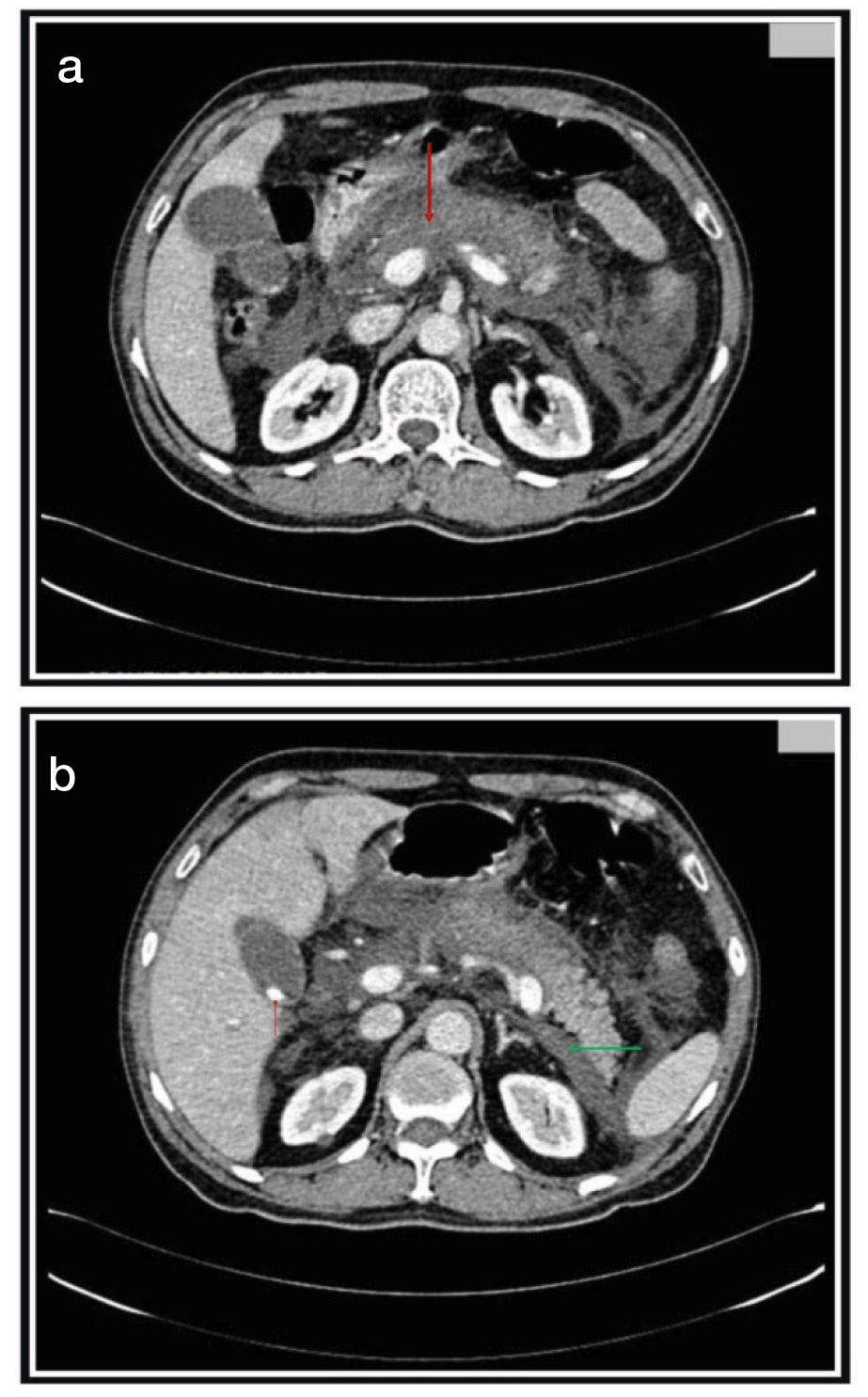
(a) Acute necrotizing pancreatitis with ascites (red arrow) and pleural effusion (green arrow), (b) Acute necrotising pancreatitis (>50%) (green arrow) both Balthazar and modified CTSI score 10 suggestive severe pancreatitis.
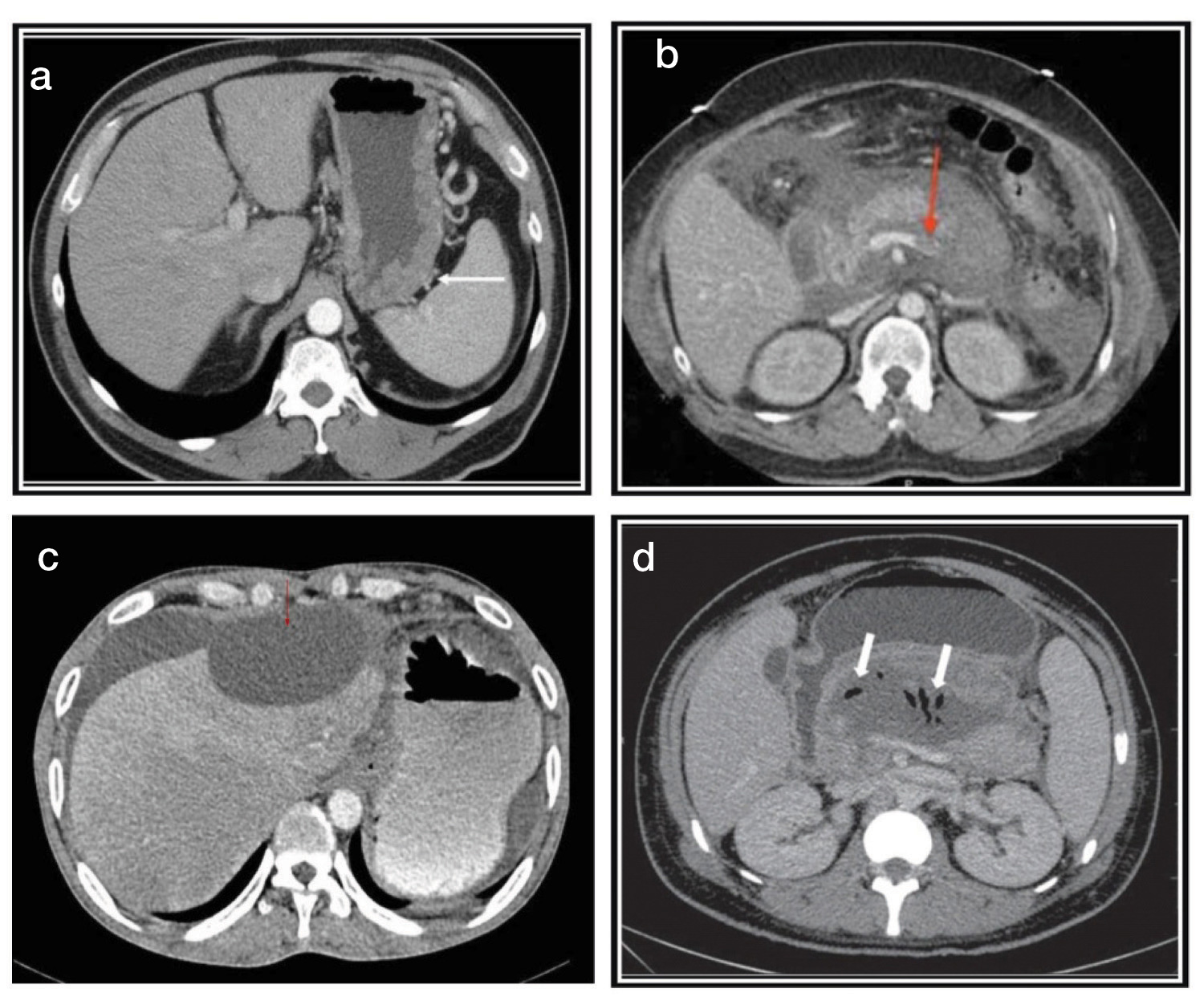
(a) Acute pancreatitis associated with thickened stomach wall. (b) Acute necrotizing pancreatitis complicated by splenic vein thrombosis. (c) Acute pancreatitis complicated by subcapsular collection. (d) Acute gangrenous pancretitis.
Discussion
The present study was undertaken to evaluate the acute pancreatitis on CT and the patient was prognostically correlated on the basis of CTSI (including Balthazar’s Computed Tomography Severity Index and the Modified Computed Tomography Severity Index). The study group consisted of 35 male and 15 female patients with a male: female sex ratio of 2:1 In a prospective study by Block et al., consisted of 61 (65.6%) males and 32 (34.4%) females with a male to female ratio of 2:1 [9]. Silverstein et al., in his prospective study of 102 patients, also had a male to female ratio of 2:1 [10].
In our study, most common aetiological factors were cholelithiasis (42%) and alcoholism (38%) followed by idiopathic (24%), trauma (2%) and drug induced (2%). Casas et al., in their study of 148 patients, found the cause of acute pancreatitis as gall stones in 57%, alcohol over indulgence in 21% and to both in 5% which is in concordance with the present study [11]. According to Steinberg et al., biliary calculi and alcohol together constituted about 80-90% of causes of acute pancreatitis, the frequency varied in different populations. Peripancreatic inflammatory changes were the most common CT findings seen in 88% of the cases of acute pancreatitis. Mendez et al., found that out of 32 patients, 28 (87.5%) exhibited extrapancreatic spread of the inflammatory process In the present study, the pancreatic gland was enlarged in 60% cases [12]. Silverstein et al., found enlargement of the pancreas in 68% of the cases as in this study [10]. And also, similar findings concluded in a study by Irshad Ahmad Banday et al., [13]. Infected necrosis occurred in 4 cases (8%) in this study Silverstein et al., and Mendez et al., have also reported an incidence of infected necrosis in 10.5% and 3% respectively [5,9]. Twenty-five patients (50%) had necrosis of the pancreas. Six (24%) patients had less than 30%, 5 (20%) patients had 30-50% necrosis and majority 14 (56%) of them had more than 50% pancreatic gland necrosis. Consequently 76% of the cases had more than 30% pancreatic necrosis.
Balthazar et al., found that on the basis of initial assessment, pancreatic necrosis was detected in 22% of the patients of which 28% patients had less than 30% necrosis, 22% had 30-50% and 50% patients had more than 50% necrosis which is similar to the present study [14]. Extra-pancreatic and systemic complications occurred in 34(68%) of the patients in our study.
The most common complication was pleural effusion seen in 46% of the cases with left pleural effusion being commoner. Balthazar et al., also found left pleural effusion to be the most common abnormality (43% of the cases) which is similar to the present study [14]. Ascites was found to be present in 17 patients (34%) in our study. Venous thrombosis were seen in 4 patients (8%). Irshad Ahmad Banday et al., in their study found ascites to be the second most common complication and was seen in 18 patients (36%) [13]. Among vascular complications, venous thrombosis was the most common (3 in portal vein and 1 in splenic vein). A fairly common finding in the present study was inflammation of gastrointestinal tract seen in 12(24%). A recent study by Irshad Ahmad Banday et al., stated that GI involvement was found in 13 patients that is (26%) [13]. Balthazar et al., have also reported similar incidence [14]. There was a proportionally increasing trend of gland necrosis with increasing severity of Balthazar grade; 45% patients in grade C, 54% patients in grade D and 69% patients in grade E had gland necrosisade E pancreatitis (28%) as in our study with the most common type being grade C pancreatitis.
Balthazar et al., found that necrosis was present in 7% patients with grade B, 1% with grade C, 17% with grade D and 52% with grade E pancreatitis [14]. Their findings were on the lower side as compared to this study. The possible explanation for this is the large number of patients having mild pancreatitis in their study group. Using the currently accepted Balthazar CTSI, the severity of acute pancreatitis was graded as mild (score of 0-3) in 21 (42%) cases, moderate (score of 4-6) in 12 (24%) and severe (score of 7-10) in 17 (34%) patients. Using the modified CTSI scoring, maximum number 22 (44%) of the patients had severe (score of 8-10) pancreatitis. Mild (score of 0-2) and moderate (score of 4-6) pancreatitis were categorized in 9(18%) and 19 (38%) patients respectively. This was fairly similar to the study conducted by Irshad Ahmad Banday et al., where in when Balthazar CT Severity Index was employed, acute pancreatitis was graded as mild in 22/50 (44%), moderate in 11/50 (22%) and severe in 17/50 (34%) patients [13]. In contrast, when using the Modified CT Severity Index, a much larger number, viz. 22/50 (44%) patients were placed in the severe pancreatitis group and 9/50 (18%), 19/50 (38%) patients as mild and moderate pancreatitis.
According to Balthazar CT severity index, amongst the patients with mild pancreatitis (n=2l), average duration of hospital stay was 17 days). In the moderate group pancreatitis group (n=12), average duration of hospital stay was 25 days. In the severe group (n=17), average duration of hospital stay was 23 days.
Modified CT scoring system correctly predicted the outcome in all the patients who had a shift in their severity grades than Balthazar CTSI. The change in severity scoring was seen mainly due to the presence of extrapancreatic complication.
The strong relationship between the Modified CT severity index and the patient outcome in this study corroborates with the findings of Mortele et al., [7]. Similar trends in duration of hospital stay, intervention or surgery, evidence of infection, organ failure, and mortality in patients with variable grades of severity of pancreatitis were observed in our study as that seen by Mortele in their study. This also correlated with the study by Irshad Ahmad Banday et al., which concluded that Modified CT Severity Index is a simpler scoring tool and more accurate than the Balthazar CT Severity Index [13].
Results of our study were also found similar to a study conducted by Shivanand Melkundi et al., which showed a significant correlation of grades of severity of acute pancreatitis based on MCTSI with patient outcome parameters than grades of severity of acute pancreatitis based on CTSI [15].
Patient outcome using currently accepted Baltazar CTSI (N=50) showed intervention and length of stay was more significantly (p-value=0.02 and 0.01 respectively) associated with moderate grade. Infection, organ system failure and death were significantly associated with severe grade. Whereas with Modified Mortele CTSI (N=50) the average duration of hospital stay was significant more (p-value=0.02) with severe grade.
Patient outcome in terms of organ failure and death is more accurately assessed by revised Atlanta classification in comparison with Balthazar and modified ct severity index. The revised classification seems to be a good predictor for clinical outcome of AP Shyu JY et al., [16].
Limitations
In patients of derange renal function and pregnant patients contrast CT is contraindicated. Repeated follow-up study was not possible due to cost and radiation exposure. Different treatments were given to patients which changed the patient outcome. Sample size was small which may have affected the result. As per the revised Atlanta classification, CECT is useful after first week. However, in first week only clinical parameters are useful.
Conclusion
Contrast enhanced Computed Tomography is excellent diagnostic modality to stage the severity of inflammatory process, detect the pancreatic necrosis and depict local complications and grading of severity of acute pancreatitis. The scores obtained with the modified Mortele index, showed a stronger correlation for all outcome parameters in all the patients better than the Balthazar index. Revised Atlanta classification is more accurate than modified Mortele index and Balthazar severity index for assessing patient mortality and organ failure.