Superior Mesentric Artery Syndrome in a Patient with Subacute Intestinal Obstruction: A Case Report
Amarjit Kaur1, Naveen Chandrashekhar Pawar2, Sonam Singla3, Jaswinder Kaur Mohi4, Shivani Sharma5
1 Professor, Department of Radiodiagnosis, GMCPatiala, Punjab, India.
2 Junior Resident, Department of Radiodiagnosis, GMCPatiala, Punjab, India.
3 Junior Resident, Department of Radiodiagnosis, GMC, Patiala, Punjab, India.
4 Associate Professor, Department of Radiodiagnosis, GMCPatiala, Punjab, India.
5 Junior Resident, Department of Radiodiagnosis, GMCPatiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Naveen Chandrashekhar Pawar, Junior Resident, Department of Radiodiagnosis/X Ray Department, Rajindra Hospital, Patiala, Punjab-147001, India.
E-mail: naveencp27@gmail.com
Superior Mesenteric Artery (SMA) syndrome is one of the rare cause of proximal small bowel obstruction wherein, the third part of the duodenum is compressed between the SMA at its origin and abdominal aorta due to decreased angulations in these two vessels. This decreased angulation exerts a compression effect on third part of the duodenum, resulting in duodenal obstruction which may be complete or partial. There are number of causes which can lead to this entity and will be discussed briefly. Here we report imaging findings of such a rare cause of proximal small bowel obstruction in a young male patient who presented to the emergency surgical department with non specific symptoms of pain abdomen and abdominal fullness. Patient was evaluated under the standard protocol in management of abdominal pain. General physical examination, erect and supine radiograph were taken. On barium meal follow-through examination, there was paucity of contrast agent distal to the second part of duodenum with proximal dilation of stomach, first and second part of duodenum which raised us the possibility of SMA syndrome. Reconstructed CECT abdomen confirmed the decreased angulation between SMA and abdominal aorta and diagnosed it as SMA syndrome. Findings were correlated on duodenojejunostomy anastomotic surgical procedure. Diagnosing and reporting such a case of SMA syndrome is of utmost importance because the clinical presentation being non-specific pertaining to small bowel obstruction which may pose a diagnostic difficulty to the surgeon and with the further delay in diagnosis, patients may end up with chronic symptoms and complications of the disease, repeated hospital visits and electrolyte abnormalities.
Barium studies, Decreased aortomesenteric angle, Wilkie’s syndrome
Case Report
A 28-year-old male patient presented to the Surgical Emergency for repeated chronic abdominal complaints. He gave history of intermittent colicky, non-radiating postprandial epigastric pain accompanied by feeling of fullness and vomiting for the last 2 years. He also had complaints of constipation for which he was on medications for symptomatic relief. Patient had significantly reduced his diet intake during this period and also had history of gradual weight loss. He had no significant past history of any infective diseases like tuberculosis, brucellosis, etc. He gave no history of previous abdominal surgeries and no history of diabetes or other chronic illness. On general physical examination the patient was thin built, around 165 cm in height, co-operative and well oriented. His vital signs were within normal limits. Systemic examination (CVS, RS, CNS) were unremarkable. Abdominal examination revealed epigastric fullness, hyper peristaltic bowel sounds and distended tender abdomen. Based on the history and clinical examination, provisional diagnosis of sub acute intestinal obstruction was made and sent for investigations. On first visit of the patient to the Radiology Department, plain X-ray abdomen (erect) was taken and reported as dilated stomach with reduced distribution of the gas in the distal bowel and no free air under both the domes of diaphragm. The patient at this point was managed conservatively with Ryle’s tube decompression and intravenous fluids. Baseline haematologic investigations were carried out, which turned out to be normal. Following this patient was ordered for upper GI barium study. And on suspicious findings of Superior mesenteric artery (SMA) syndrome on barium studies (mentioned later), patient was sent for contrast enhanced CT-scan of the abdomen. These imaging findings were correlated and a final diagnosis of “SMA syndrome” was made. Patient was not given any conservative management at this point because he had chronic symptoms and medical management of obstruction was unsuccessful with persistence of symptoms. Patient was taken up for elective surgery and the imaging findings were confirmed on surgery. Patient was absolutely symptom free in postoperative period.
Imaging Findings
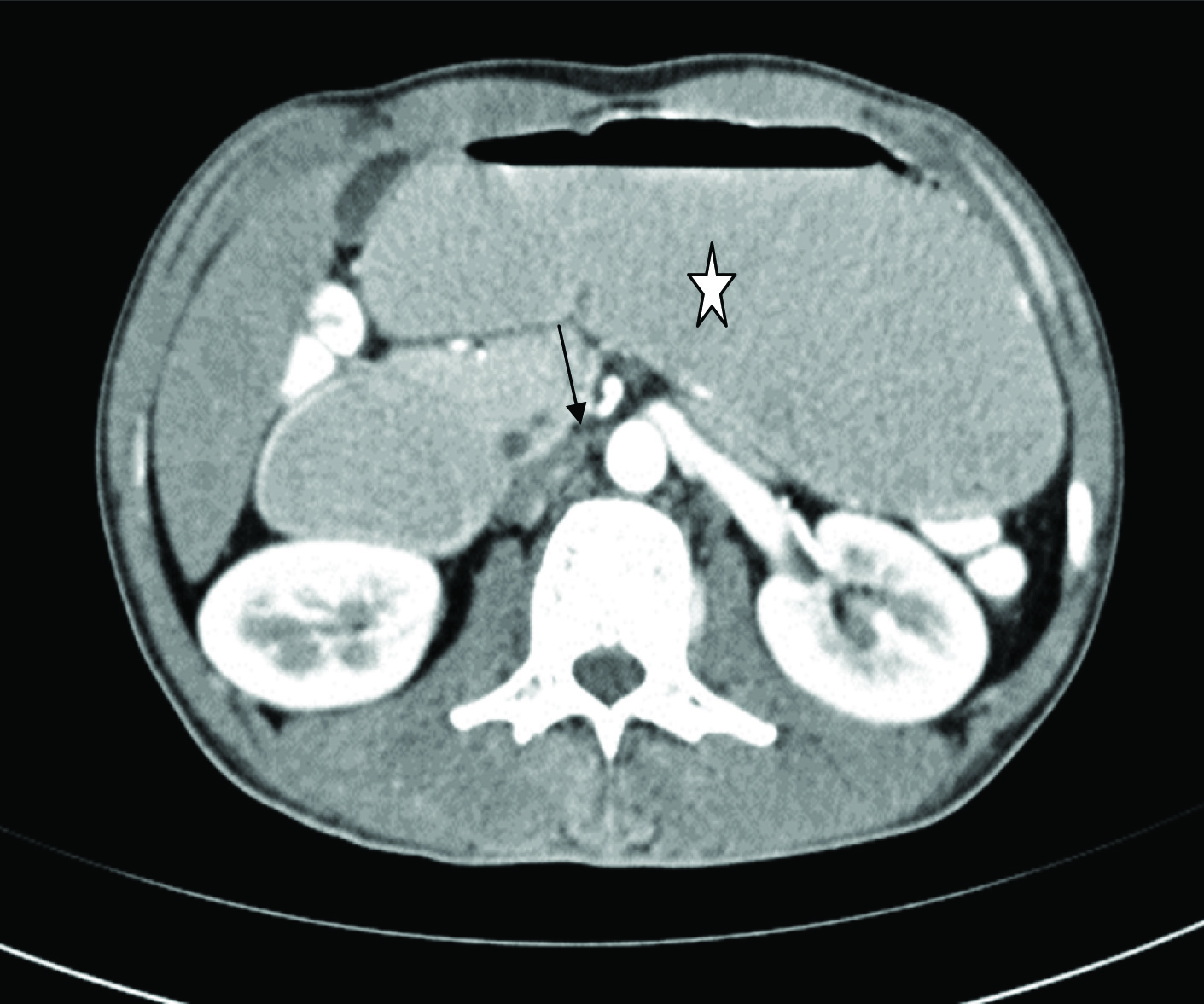
Erect abdominal radiograph revealed dilated stomach with reduced distribution of gas in the distal bowel loops. On barium meal follow through the findings were, dilated first and second portion of the duodenum (MEGADUODENUM) with abrupt linear vertically oriented cut-off of contrast at the junction of the second and third part of the duodenum [Table/Fig-1]. Upon repositioning the patient to lateral and prone position, there was subsequent contrast transit to the small-caliber third and fourth portions of the duodenum making the likely diagnosis of SMA Syndrome [Table/Fig-2]. CT of the abdomen and pelvis with oral and intravenous contrast demonstrated dilatation of the first and second parts of the duodenum with narrowing and small caliber of the third part as it crosses the midline posterior to the SMA and decreased aortomesenteric angle [Table/Fig-3].
Barium study showing dilated proximal part (white star*) and narrowed third part (white circle 0) of duodenum with no passage of contrast seen distally. Black arrow;stomach.
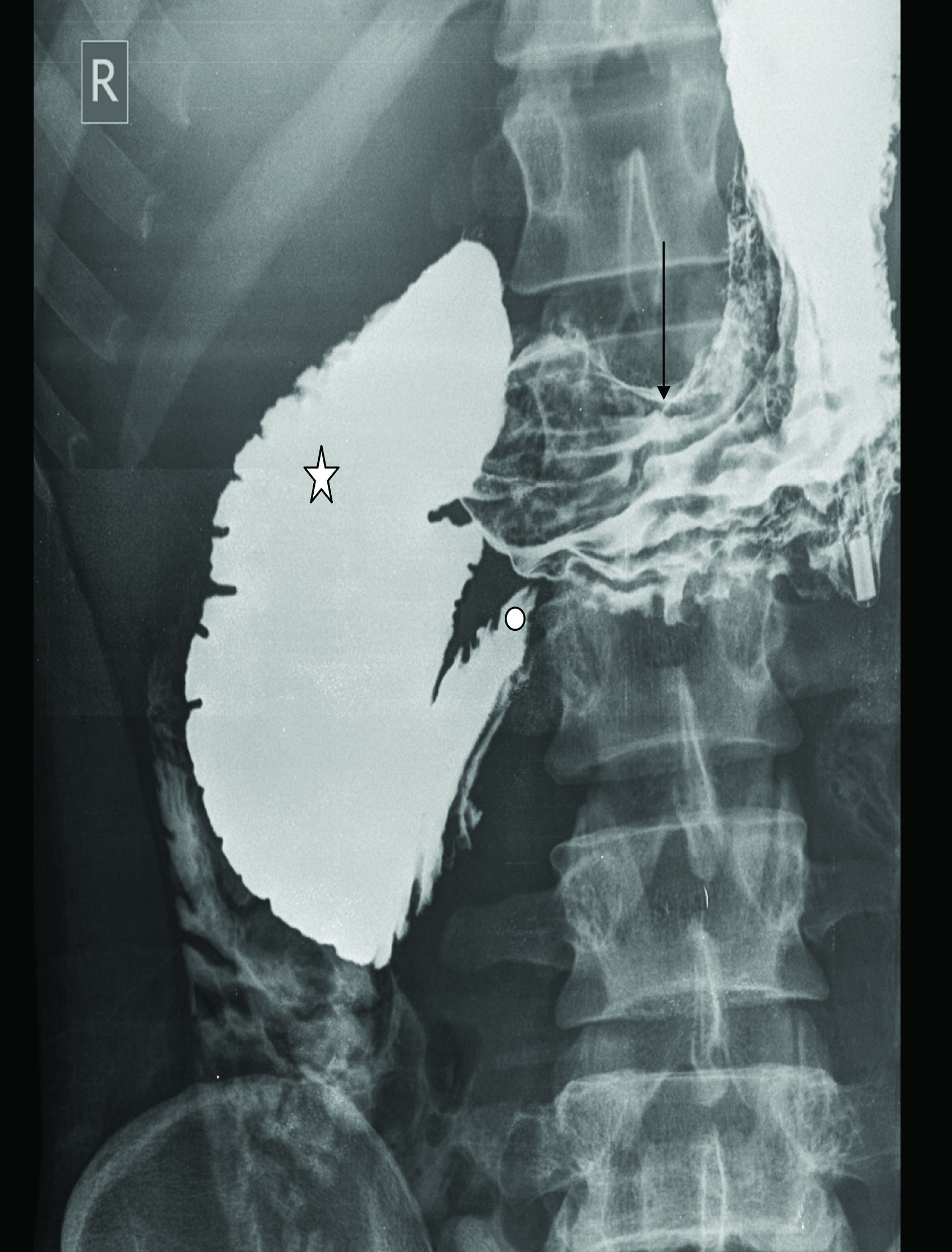
On repositioning the patient to prone, the contrast is seen passing into the third and fourth part (arrowheads) of duodenum. Black arrow; stomach.

CECT showing dilated stomach (white star) and duodenum up to the level of superior mesenteric artery (black arrow).
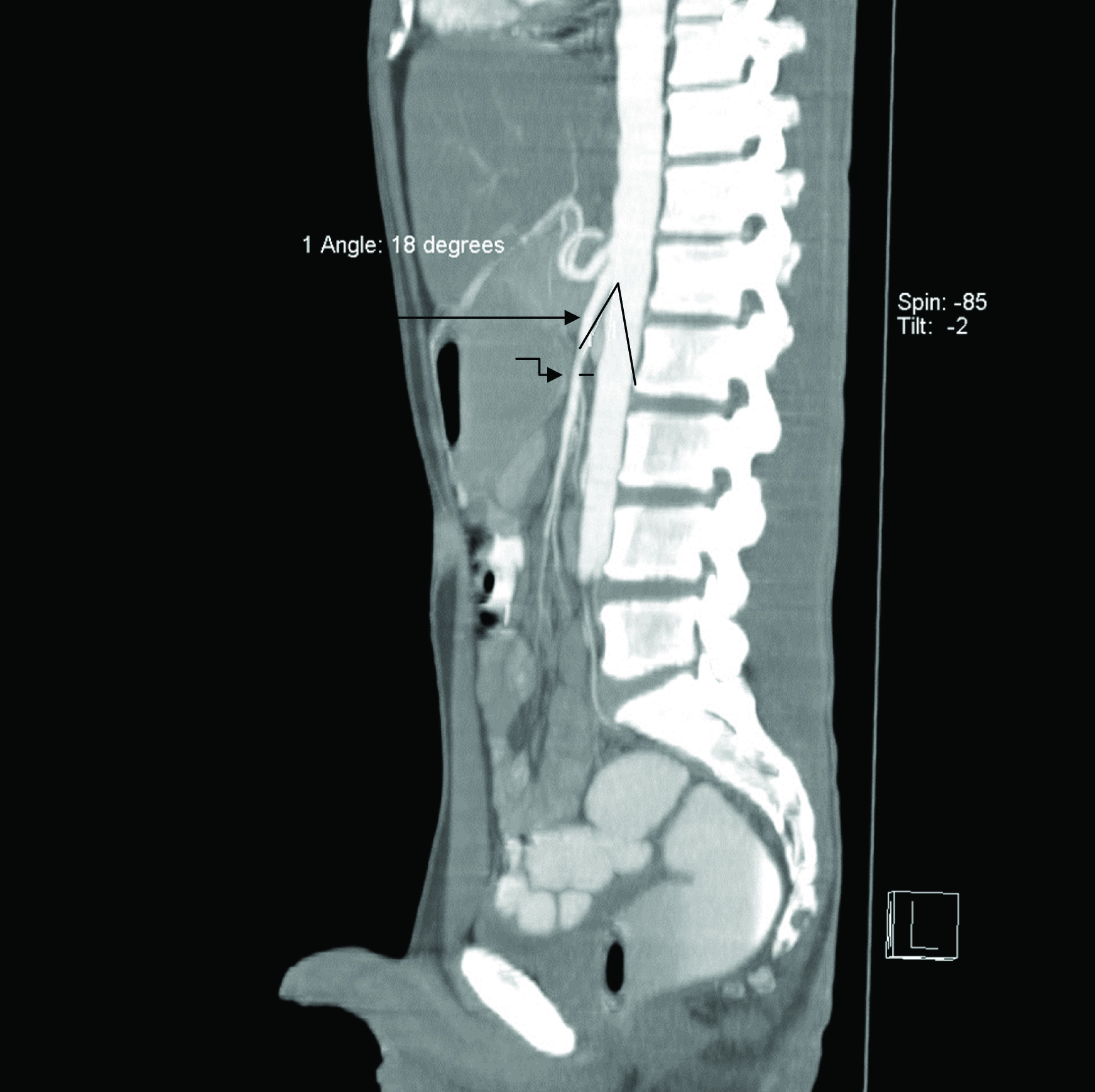
Reconstructed sagittal CT section of the abdomen – pelvis enabled us in the Direct visualization of vascular compression of the duodenum and measurement of aortomesenteric distance precisely.
Normally, the aortomesenteric angle and aortomesenteric distance is 25° to 60° and 10 to 28 mm, respectively
In our case, both parameters were reduced, with values of 18° and 7mm on reconstructed sagittal CT images. [Table/Fig-4].
Reconstructed CECT image shows reduced angle distance between SMA and abdominal aorta. ANGLE was reduced to 18 degrees and distance was approx 7mm (curved arrow)diagnostic of SMA syndrome. Note the thin built of patient in this sagittal reconstructed CT image with significantly less retroperitoneal fat.
SURGICAL NOTES; Exploratory laparotomy was done through a midline incision under all aseptic precautions. Surgeons confirmed the extrinsic compression of the third part of the duodenum with proximal dilation of stomach, first and second part of duodenum. Minimal peritoneal adhesions and small insignificant mesenteric lymph nodes were also present. Duodenojejunostomy, side to side anastomosis was done. Postoperative period was uneventful. Patient was symptom free and switched on to routine diet and gained some weight in his follow-up.
Discussion
Superior mesenteric artery (SMA) syndrome also called as Wilkie’s syndrome is a rare cause of high intestinal obstruction [1]. This entity was first described by Austrian professor Carl Von Rokitansky in 1861 [2]. Later in 1927, Wilkie came up with a detailed description of its pathophysiological association with the reduced aortomesenteric angle and reduced aortomesenteric distance [3].
Some previous studies, report incidence of SMA syndrome to be 0.1-0.3% however, the true incidence of the disease is unknown [4]. Few cases have been reported previously with the aetiology of tuberculosis, anorexia nervosa, cardiac cachexia, diabetes mellitus and spinal surgeries [5].
Normally the angle between abdominal aorta and SMA is 450 (range 38°-56°). Normal aortomesentric distance is in the range of 10-20mm. The third part or the transverse part of duodenum courses posteroinferiorly in relation to the origin of SMA [6]. Due to rapid loss of retroperitoneal fat the angle may reduce to 6°-25° giving rise to SMA syndrome [7]. This syndrome is known by a variety of names like aortomesenteric artery compression, arteriomesenteric duodenal compression, duodenal vascular compression [8].
Causes which predispose to this syndrome include prolonged bed rest, rapid weight loss, thin built patient, application of body cast in the correction of scoliotic spine trauma, cachexic states and other malabsorption states. Anatomical causes include short ligament of treitz, unusual low origin of SMA also predispose to SMA syndrome [9].
Patients may present with acute symptoms of intestinal obstruction or more commonly with chronic insidious symptomatolgy like postprandial fullness, early satiety, recurrent episodes of abdominal pain and cramping. Sometimes patient may typically complain of pain abdomen which is aggravated by lying supine and relieved on left lateral decubitus or even in knee chest position which increase the aortomesenteric angle, subsequently reducing small bowel mesentery tension [10].
Diagnosing a case of SMA syndrome is based on interpreting clinical signs and symptoms with clinical suspicion combined with radiological investigations. Barium study findings though non-specific, include dilation of the first and second part of the duodenum with an abrupt narrowing at the third part. Turning the patient into prone/left lateral decubitus position relieves the obstruction and contrast material will be seen opacifying the small bowel distal to the SMA [11]. CECT demonstrates similar findings of bowel obstruction & reconstructed CT images provide an additional advantage of measuring the aortomesentric angle and distance, and thus have become an indispensable part of the diagnostic protocol [12].
The mainstay of management in most cases of SMA syndrome is conservative medical management which aims at resolution of underlying conditions and weight gain. It involves duodenal and gastric decompression, and making the patient to lie in prone or left lateral decubitus position in order to relieve the compression on third part of duodenum [13]. Fluid, electrolyte imbalance is corrected and nutritional support is provided for the restoration of retroperitoneal fat [2,9]. Surgical treatment is undertaken if the conservative management fails. Duodenojenunostomy procedure is the most common surgery undertaken in such cases [9].
Conclusion
Diagnosing SMA syndrome needs high degree of suspicion and correlation between clinical and radiological findings. Reporting such rare case and there imaging findings will also help in knowing the actual incidence of the disease entity. In our case, the patient clinical symptoms, history and radiological findings lead us towards the diagnosis of SMA syndrome. Important here is to think for the aetiology. As in this patient there was no history of trauma, burns, anorexia nervosa, previous abdominal surgeries, infective and inflammatory diseases. The only possible aetiology in this patient was thin built of the patient with decreased retroperitoneal fat which was evident on physical examination and on reconstructed CT. Chronic repeated symptoms, Clinical suspicion and imaging findings should alarm the treating Doctor to raise the possibility of SMA syndrome.
[1]. Chan DK, Mak KS, Cheah YL, Successful nutritional therapy for superior mesenteric artery syndromeSingapore Med J 2012 53(11):e233-36. [Google Scholar]
[2]. Ahmed AR, Taylor I, Superior mesenteric artery syndromePostgrad Med J 1997 73:776-78. [Google Scholar]
[3]. Wilkie D, Chronic duodenal ileusBr J Surg 1921 :204-14. [Google Scholar]
[4]. Shiu JR, Chao HC, Luo CC, Clinical and nutritional outcomes in children with idiopathic superior mesenteric artery syndromeJ Pediatr Gastroenterol Nutr 2010 51(2):177-82. [Google Scholar]
[5]. Ansari WA, Shaikh AS, Jamadar NM, Superior mesenteric artery (wilkie’s) syndromeBombay Hospital Journal 2009 51:503-07. [Google Scholar]
[6]. Gerasimidis T, George F, Superior mesenteric artery syndrome. Wilkie syndromeDig Surg 2009 26(3):213-14. [Google Scholar]
[7]. Welsch T, Buchler MW, Kienle P, Recalling superior mesenteric artery syndromeDig Surg 2007 24:149-56. [Google Scholar]
[8]. Townsend CM, Naoum JJ, Vascular compression of the duodenum. In: Fischer J. E., editorMastery of Surgery 2007 5thLippincott Williams & Wilkins:955-61. [Google Scholar]
[9]. Scovell S, Hamdan A, Superior mesenteric artery syndrome. Upto DateWaltham, MAUpto Date; September 19, 2015 [Google Scholar]
[10]. Cohen LB, Field SP, Sachar DB, The superior mesenteric artery syndrome. The disease that isn’t, or is itJ Clin Gastroenterol 1985 7:113-16. [Google Scholar]
[11]. Agrawal GA, Johnson PT, Fishman EK, Multidetector row CT of superior mesenteric artery syndromeJ Clin Gastroenterol 2007 41:62-65. [Google Scholar]
[12]. Unal B, Aktaş A, Kemal G, Bilgili Y, Güliter S, Daphan C, Superior mesenteric artery syndrome: CT and ultrasonography findingsDiagn Interv Radiol 2005 11:90-95. [Google Scholar]
[13]. Sapkas G, O’Brien JP, Vascular compression of the duodenum (cast syndrome) associated with the treatment of spinal deformities. A report of six casesArch Orthop Trauma Surg 1981 98:7-11. [Google Scholar]