Periodontitis is a complex, multifactorial disease characterized by the loss of connective tissue attachment with destruction of periodontium. The primary goal in periodontal therapy includes removal of the etiological factors by mechanical periodontal treatment, which sometimes fails to eliminate the anaerobic infection at the base of the pocket, within the gingival tissue or in furcation defect [1–3]. This can act as a bacterial reservoir from which recolonization of the tooth surface can occur after instrumentation [4]. The use of antimicrobial agents as an adjunct to mechanical therapy has proven to be effective in the treatment of periodontitis.
As a local drug delivery system, tetracycline is used widely in periodontal treatment as it is active against periodonto-pathogenic microorganism [5,6]. It possesses widespread bacteriostatic properties and acts slowly by binding to the tooth surface, inhibiting the activity of collagenase at low concentrations and thus preventing periodontal tissue destruction [7,8]. The high substantivity is one of the most important characteristics of the drug.
Minocycline is a broad spectrum tetracycline antibiotic compared to the other members of the group. It is one of the most active antibiotics against most of the microorganisms associated with periodontal disease. It has the most marked substantivity and shows greater solubility in lipids. It is classified as long acting drug and is commercially available as “Periofeel” which is a bio-absorbable sustained local drug delivery system consisting of 2% minocycline hydrochloride in a matrix of hydroxyethyl-cellulose, aminoalkyl-methacrylate, triacetine and glycerine. Periofeel contains 10mg of minocycline in 0.5gm of ointment in a disposable polypropylene applicator (2% minocycline HCl). One of the advantages of local drug delivery system is that the drug can be placed at a higher concentration, sub-gingivally, for 24hrs with sustained release. The drug concentration decreases exponentially following a first order kinetics [9,10].
Research has yielded promising results with the local application of minocycline in the treatment of periodontal disease, compared with other non-surgical therapies [11–15]. Van Steenberghe D et al., and Cortelli JR et al., have shown that the application of minocycline resulted in effective improvement in the post-operative maintenance period [16–18]. The clinical data using 2% Minocycline ointment as local drug delivery as an adjunct to periodontal surgery is limited. Hence we aimed to evaluate the effectiveness of 2% minocycline ointment as an adjunct to periodontal surgical therapy and post-operatively on 3rd and 6th month for the treatment of generalized chronic periodontitis.
Materials and Methods
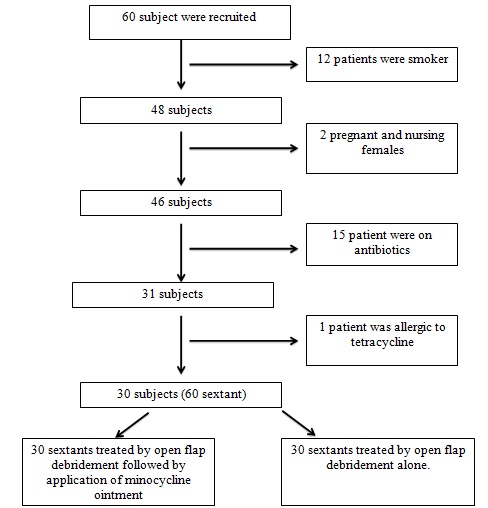
In the present clinical study 60 subjects were recruited from the Department of Periodontology, Meenakshi Ammal Dental College, Chennai between the period of February 2014 – February 2015. Out of 60 subjects 12 subjects were smokers, two pregnant and lactating females, 15 subjects were on antibiotics and one subject was allergic to tetracycline. Hence, they were excluded from the present investigation. Finally 30 subjects were selected with 60 posterior sextants in a split mouth design and were divided into two groups based on random allocation through coin toss (Group A - Experimental Group and Group B - Control Group) based on the inclusion and exclusion criteria [Table/Fig-1]. The inclusion criteria comprised of systemically healthy patients with age range between 30–50years, diagnosed with untreated generalized chronic periodontitis with a pocket depth ≥6mm around two or more teeth, in two or more sextants were included in the study. The patients taking antibiotics or anti-inflammatory drugs, allergic to tetracycline, pregnant or nursing females, smokers, those using chlorhexidine or any other mouth rinse were excluded from the present investigation. The ethical approval was obtained from the Institutional Review Board, Committee, MAHER University, Chennai (IRB number: 2014/012). A written informed consent was obtained from all the participants who were enrolled after full explanation of the present investigation. Group A (Experimental Group)–30 sextants were treated with periodontal flap surgery followed by application of minocycline ointment. Group B (Control Group)–30 sextants were treated with periodontal flap surgery alone.
Periodontal Examination
In both the groups, following clinical parameters were assessed pre-operatively such as plaque index, gingival bleeding index, probing pocket depth and clinical attachment level.
Plaque index measurements were carried out at four sites around each tooth (mesio-buccal, mid-buccal, disto-buccal and lingual). A mouth mirror and a dental explorer were used after air-drying the teeth to assess plaque. The plaque index score for the area was obtained by totaling the four plaque scores per tooth. The sum of the plaque index scores per tooth were divided by four to obtain the plaque index score for the tooth. For an individual, the plaque index score was calculated by adding the plaque index score per tooth and dividing by the number of teeth examined [19].
Similarly, for determining the gingival bleeding index, the gingival crevice was gently probed with the William’s periodontal probe. If the bleeding occurred within 10 seconds, it indicated a positive score and this was expressed as a percentage of the total number of gingival margins examined [20].
Probing pocket depth was measured clinically using William’s probe. The probe was inserted parallel to the vertical axis and pocket was measured to the nearest millimeter. The probing pocket depth was measured at six sites (mesio-buccal, mid-buccal, disto-buccal, mesio-lingual, disto-lingual and mid-lingual) of each tooth and the deepest/highest probing depth was recorded for each individual tooth [19].
Clinical attachment level score was obtained by measuring the distance between the base of the pocket and a fixed point on the crown, such as cemento-enamel junction in a sextant [19].
Pre-Surgical Procedure
After the clinical parameters were recorded, Phase I therapy (full mouth scaling, root planning and oral hygiene instructions) was performed. The patients were then put under observation to assess the oral hygiene practice and the response of the gingival tissue to Phase I therapy.
After two weeks, patients were recalled and based on further treatment protocol, periodontal flap surgery was planned. Group A (Experimental Group) underwent periodontal flap surgery followed by application of minocycline ointment. Group B (Control Group) underwent periodontal flap surgery alone.
Surgical Procedure
The operative sites were anaesthetized with 2% lignocaine hydrochloride with adrenaline (1:200000). Crevicular incisions were made using Bard Parker No.15 blade on the facial and lingual/palatal surface of each tooth segment or area involved. A full thickness mucoperiosteal flap was reflected using periosteal elevator taking care to preserve the maximum amount of gingival connective tissue in the flap. After exposure, the root surface was planed and the flap was trimmed to remove granulation tissue tags and to minimize bleeding. The flap was then sutured and hemostasis was achieved.
At the experimental site (Group A) after suturing, 10mg of 2% minocycline ointment with a disposable polypropylene applicator was placed around adjacent teeth that exhibited a baseline pocket depth ≥6mm. The applicator tip was inserted into the pocket until resistance was felt, and then slowly pulled out, while injecting about 1mg of minocycline (Periofeel Dental Ointment 2%, Showa Yakuhin Kako Co., Tokyo, Japan) in a zig-zag motion. To prevent uncontrolled spillover effects of the ointment, mild pressure was applied over the flap with the wet gauze and excess ointment was removed and Coe Pak was placed. The use of antibiotic was avoided but analgesic (Dolo 650mg) was prescribed twice a day for three days.
Post–Operative Care
Following surgery the patients were instructed to avoid chewing on the surgical area during the first post-operative day. The use of antibiotics and mouthwash was avoided during the observation period, but patients were instructed to continue mechanical plaque control measures.
All patients were placed on a strict maintenance schedule following surgery. The sutures were removed in all sextants one week later. Recall appointment were scheduled once in 10 days for the 1st months. At every recall appointment, oral hygiene was checked. At 3rd month, the clinical parameters were recorded in both the groups followed by the application of minocycline ointment in all the selected pockets in the Group A. The clinical parameters were again recorded in both the groups at 6th month. The difference between pre and post–operative values was assessed and then statistically analyzed.
Statistical Analysis
Using the SPSS version 22.0 software, the mean and standard deviation of the clinical parameters at various time points were estimated for each study group. To compare mean value between two groups independent sample t-test was applied. Paired t-test was applied to compare the mean values between two time points. In the present study, p<0.05 was considered as the level of significance.
Results
On comparing the mean change in plaque index score at different time points between the groups, it was found that the mean plaque index score was significantly reduced at 6th month (0.91±0.28) in Group A compared to Group B. Similarly, there was reduction in the mean change from 0 day to 3rd month, 0 day to 6th month and 3rd month to 6th month in Group A compared to Group B. However it was not statistically significant [Table/Fig-2].
Comparison of mean, standard deviation, mean change and test of significance for plaque index score at different time points within the groups and between the groups.
| Time Point | Group A(Mean ± SD) | Group B(Mean ± SD) | p-value(Intergroup) |
|---|
| 0 day(Baseline) | 1.84 ± 0.36 | 1.90 ± 0.37 | 0.560(NS) |
| 3rd Month | 1.20 ± 0.41 | 1.41 ± 0.42 | 0.051(NS) |
| 6th Month | 0.91 ± 0.28 | 1.08 ± 0.29 | 0.034*(S) |
| Mean change(0 day- 3 months) | 0.64 ± 0.52 | 0.48 ± 0.46 | 0.217(NS) |
| Mean change(0 day - 6 months) | 0.92 ± 0.44 | 0.81 ± 0.41 | 0.330(NS) |
| Mean change(3months-6months) | 0.28 ± 0.18 | 0.33 ± 0.19 | 0.305(NS) |
Independent t- test
S – Significant*
NS – Non significant
When the mean gingival bleeding index was compared between the Group A and Group B, it was found that there was significant reduction at 3rd month and 6th month. Similarly, there was significant reduction in the mean change from 0 day to 3rd month, 0 day to 6th month and 3rd month to 6th month in Group A compared to Group B and the difference was statistically significant [Table/Fig-3].
Comparison of mean, standard deviation, mean change and test of significance for gingival bleeding index score (in%) at different time points within the groups and between the groups.
| Time Point | Group A(Mean ± SD) | Group B(Mean ± SD) | p-value(Intergroup) |
|---|
| 0 day(Baseline) | 92.19 ± 10.52 | 94.37 ± 8.98 | 0.39(NS) |
| 3rd Month | 57.78 ± 10.95 | 72.33 ± 11.80 | <0.001*(S) |
| 6th Month | 26.42 ± 9.27 | 55.11 ± 10.27 | <0.001*(S) |
| Mean change(0 day- 3 months) | 34.41 ± 11.94 | 22.04 ±8.23 | <0.001*(S) |
| Mean change(0 day - 6 months) | 65.76 ± 11.55 | 39.25 ± 10.13 | <0.001*(S) |
| Mean change(3months-6months) | 31.35 ± 9.79 | 17.21 ± 9.99 | <0.001*(S) |
Independent t- test
S – Significant*
NS – Non significant
When the mean probing pocket depth was compared between the Group A and Group B, it was found that there was significant reduction at 3rd month and 6th month. Similarly, there was significant reduction in the mean change from 0 day to 3rd month and 0 day to 6th month for Group A compared to Group B and the difference was statistically significant. The mean probing pocket depth from 3rd month to 6th month was more for Group A compared to Group B, but the difference was not statistically significant (p=0.285) [Table/Fig-4].
Comparison of mean, standard deviation, mean change and test of significance for probing pocket depth (in mm) around teeth with a baseline probing pocket depth≥6mm score at different time points within the groups and between the groups.
| Time Point | Group A(Mean ± SD) | Group B(Mean ± SD) | p-value(Intergroup) |
|---|
| 0day(Baseline) | 6.73 ± 0.64 | 6.45 ± 1.37 | 0.31(NS) |
| 3rd Month | 4.22 ± 0.65 | 5.04± 1.10 | <0.001*(S) |
| 6th Month | 3.04 ± 0.52 | 3.99 ± 0.96 | <0.001*(S) |
| Mean change(0 day- 3 months) | 2.51 ± 0.84 | 1.41 ± 0.58 | <0.001*(S) |
| Mean change(0 day - 6 months) | 3.68 ± 0.77 | 2.45 ± 0.78 | <0.001*(S) |
| Mean change(3months-6months) | 1.17 ± 0.48 | 1.04 ± 0.42 | 0.285(NS) |
Independent t- test
S – Significant*
NS – Non significant
We also found a significant gain in clinical attachment level (CAL) at 3rd month and 6th month. Similarly, there was significant gain in the mean CAL from 0 day to 3rd month and 0 day to 6th month for Group A compared to Group B and the difference was statistically significant. The mean CAL from 3rd month to 6th month was more for Group A compared to Group B, however the difference was not found to be statistically significant (p=0.249) [Table/Fig-5].
Comparison of mean, standard deviation, mean change and test of significance for clinical attachment level score (in mm) around teeth with a baseline probing depth≥6mm at different time points within the groups and between the groups.
| Time Point | Group A(Mean ± SD) | Group B(Mean ± SD) | p-value(Intergroup) |
|---|
| 0 day(Baseline) | 7.30 ± 0.64 | 6.97 ± 1.53 | 0.283(NS) |
| 3rd Month | 4.61 ± 0.93 | 5.51 ± 1.39 | 0.005*(S) |
| 6th Month | 3.41 ± 0.95 | 4.45 ± 1.39 | <0.001*(S) |
| Mean change(0 day- 3 months) | 2.69 ± 0.87 | 1.46 ± 0.58 | <0.001*(S) |
| Mean change(0 day - 6 months) | 3.89 ± 0.88 | 2.52 ± 0.83 | <0.001*(S) |
| Mean change(3months-6months) | 1.20 ± 0.53 | 1.06 ± 0.44 | 0.249(NS) |
Independent t- test
S – Significant*
NS – Non significant
Discussion
Periodontitis is an infectious disease that causes destruction of supporting connective tissue and bone and ultimately tooth loss. It occurs due to interaction between the colonizing bacteria in the periodontal pocket and host immune and inflammatory response. The sub-gingival pocket harbors a mixture of many pathogens rather than a single pathogenic species, and is resistant to many antibacterial therapies [21]. Putative pathogens associated with periodontal disease are susceptible to a variety of chemotherapeutic agents. These agents can be used systemically or topically as an adjunct to scaling and root planing in an attempt to further reduce the number of periodontal pathogens thereby improving the periodontal condition. In the past years, local delivery of antimicrobial agents has been extensively researched. The choice of antibacterial agents is based on the bacterial etiology of the infection. Minocycline ointment, a semi-synthetic derivative of tetracycline, has a wide spectrum of action against anaerobic as well as aerobic bacteria. Various clinical studies done by Kurimoto K and Colleagues in Japan lead to approval of minocycline hydrochloride formulation under the name Periocline (Sunstar) in August 1990 [22]. Maehara et al., also reported the inhibitory effect of minocycline against collagenase activity [23].
Our study evaluated the efficacy of a 2% minocycline ointment application as an adjunct to open flap debridement in the management of generalized chronic periodontitis in a split mouth design. The advantage of using split mouth design is that it allows the determination of superiority between the different treatment options.
In our study, periodontitis patients underwent periodontal flap surgery followed by the application of minocycline at 0 day. Patients were recalled after three months, the clinical parameters were recorded and minocycline was applied in Group A.
Studies state that, after sub-gingival debridement, bacterial recolonization of subgingival plaque occur within 120-240 days in deep pockets (Drisko CH) [24]. Haffajee AD et al., has also shown that levels of Tannerella forsythia, Fusobacterium nucleatum, Porphyromonas gingivalis, and Treponema denticola decreased significantly until three months, but increased gradually during 3rd month in pockets that were at least 6mm deep [25]. Moreover various studies state that the repeated application of minocycline to the periodontal tissue has been beneficial. Hence in our study the minocycline ointment was applied at 0 day and again at three months.
On comparing the mean changes in plaque index score between Group A and Group B the reduction in plaque index score was not statistically significant. This was in accordance with the studies done by Jones AA et al., Van Steenberghe D et al., Hellstrom MK et al., Jain R et al., Jung DY et al., [11,16,26–28].
Hence, we could not find any significant reduction in the plaque index score between Group A and Group B.
On comparing the mean reduction in gingival bleeding index score between the groups, the reduction was more in Group A compared to Group B at all time intervals and the difference was statistically significant. This is in accordance with the studies done by Williams RC et al., Van Steenberghe D et al., Jung DY et al., Atilla et al., McColl E et al., they also reported a significant reduction in the gingival bleeding index [14,17,28–30]. It has been demonstrated that bleeding on probing is associated with histopathologic and bacteriologic alteration with periodontal disease (Greenstein C et al.,) [31]. Bleeding on probing results due to increased vascularity, thinning and degeneration of epithelium and proximity of engorged vessels to inner surface. Surgical debridement itself leads to complete elimination of local factors and healing of the epithelial attachment. The addition of minocycline has an additional beneficial effect because it is an effective anti-inflammatory agent. It has shown that it specifically inhibits the collagenolytic enzyme activity produced by host tissues during inflammation by binding Ca++ and Zn++ [32]. Furthermore, Gabler and Creamer demonstrated that several neutrophil functions such as migration, O2-synthesis, and degranulation involved in inflammatory tissue destruction are suppressed with additional application of minocycline [33].
On comparing the mean reduction in probing pocket depth between Group A and Group B, the reduction was more in Group A than Group B and the reduction was statistically significant. This is in accordance with the studies done by Pandit N et al., [4], Williams RC et al., [14], Van Steenberghe D et al., [16], Van Steenberghe D et al., [17], Cortelli JR et al., [18], Jain R et al., [27], Atilla et al., [29], Meinberg TA et al., [34], Paquette DW et al., [35]. In both the groups surgical therapy was performed, which resulted in, reduction of probing pocket depth. Group A showed greater reduction compared to Group B. This was because it could be due to the reduction in the gingival inflammation by modulating the inflammatory response and by suppressing the periodontal pathogenic microbiota. During the healing period, minocycline absorbs onto the mineralized dentine and act as a transient reservoir of the antimicrobial activity. This leads to the reduced sub-gingival bacterial load and greater reduction in probing pocket depth.
However, the mean reduction in probing depth from 3rd – 6th month was more in Group A compared to Group B, but the difference was not statistically significant. This is accordance with the studies done by Jones AA et al., [11], Timmerman MF et al., [12], Radvar M et al., [36]. Mc Coll E et al., [30]. Cortelli JR et al., [18]. This could be due to the fully epithelized gingival crevice with a well-defined epithelial attachment, which is formed in one month following surgical debridement. So any further reduction in probing depth might not be statistically significant.
We also found a higher gain of clinical attachment level at 0 day - 6th month in Group A compared to Group B which was highly significant. This is in accordance with the studies done by Pandit N et al., [4], Van Steenberghe D et al., [17], Jung DY et al., [28] and Lu Chei et al., [37]. Similarly, the mean gain in clinical attachment level at 3rd – 6th month was more in Group A compared to Group B but the difference was not statistically significant. This is in accordance with the studies done by Bonito AJ et al., [10], Van Steenberghe D et al., [16], Jain R et al., [27], Radvar M et al., [36]. This could be due to greater shrinkage of gingival tissue as a result of the elimination of inflammation with the application of minocycline as an adjunct. The gain in clinical attachment level may reflect reduction in the degree of gingival inflammation rather than a true gain of connective tissue.
The clinical implication of Minocycline is that at the sites of infection the bacteria are exposed to higher doses of antibiotics, reducing the risk of resistant bacterial strains and it reaches a concentration above the minimum inhibitory concentration of putative pathogens. It also aids in reducing and eliminating the periodontal pathogens from the pockets and helps the clinician to achieve more favorable results.
Limitation
This study has certain limitations like microbial analysis would have provided a better picture about the changes in microbial colonies following minocycline application. GCF analysis to measure the levels of IL-1β and collagenase activity would have provided an insight about the anti-inflammatory property of minocycline.
Conclusion
The results demonstrate that the application of minocycline ointment, as an adjunct to open flap debridement in generalized chronic periodontitis is safe and may be used as an adjunct to the periodontal surgery. In future, a better picture can be provided with the identification of the microbial profile at the diseased site following minocycline application. Also, GCF analysis of the biomarker such as IL-1β and collagenase activity may provide an insight about the anti-inflammatory property of minocycline.
Independent t- test
S – Significant*
NS – Non significant
Independent t- test
S – Significant*
NS – Non significant
Independent t- test
S – Significant*
NS – Non significant
Independent t- test
S – Significant*
NS – Non significant