Anaemia is a universal public health problem, affecting every country irrespective of whether it is a low, middle or high-income country. It has adverse health consequences, as well as adverse impacts on social and economic development [1–3]. While the most reliable indicator of anaemia at the population level is blood haemoglobin concentration, measurements of this concentration alone do not determine the cause of anaemia. Anaemia may result from a number of causes, while the most significant contributor is iron deficiency [1]. Previous reviews and reports estimate that a near 50% of anaemia case burden could be attributed to iron deficiency. The local conditions prevailing in different population groups and geographical areas can influence this proportion [1,4,5].
Apart from other micronutrient deficiencies like Folate, Riboflavin, Vitamins A and B12, other causes of anaemia include acute and chronic infections like malaria, tuberculosis, HIV and cancer. Inherited or acquired disorders that affect haemoglobin synthesis, red blood cell production or red blood cell survival (e.g. Haemoglobinopathies) are the other causes of anaemia. Raised risk of maternal and perinatal mortality and low birth weight are known consequences of anaemia during pregnancy [6,7]. Iron deficiency anaemia can down the productivity and induce fatigue by its untoward affect on cognitive and motor development [8,9]. Maternal and neonatal mortality were responsible for 3.0 million deaths in 2013 in developing regions and significant contributors to overall global mortality [10,11]. Nearly 90000 deaths were estimated to be due to iron deficiency alone irrespective of age and sex [12]. The National programs should take into account the common aetiologies affecting the anaemia prevalence in different population groups and base their strategies accordingly.
Surveillance of iron deficiency involves an ongoing process of recording and assessing iron status in an individual or a community [4]. Worldwide, the most common method of screening individuals or populations for iron deficiency involves determining the prevalence of anaemia by measuring blood haemoglobin or haematocrit levels. World Health Organization (WHO) proposed a classification of public health significance of anaemia in populations on the basis of prevalence estimated from blood levels of haemoglobin or haematocrit [13]. The prevalence of Hb values below the population-specific Hb threshold is used to classify countries by the level of the public health problem by WHO into four categories. If the prevalence of anaemia is less than or equal to 4.9 percent the population group is classified as ’No Public Health Problem’. Similarly, between 5.0 and 19.9 percent it is ’Mild Public Health Problem’. Between 20.0 and 39.9 percent it is ’Moderate Public Health Problem’. When prevalence is equal to or above 40.0 percent the population is classified under ’Severe Public Health Problem’-(SPHP).
The National Family Health Survey-3 (NFHS-3, 2005-06), a household survey aimed at having national and state representative data on population health and nutrition, estimated the prevalence of anaemia to be 70% in children aged 6–59 months and 55% in females aged 15–49 years. The prevalence of anaemia in children age 6-59 months was quoted to increase steadily with the mother’s level of anaemia, reaching 82 percent for children of mothers who are severely anaemic [14].
Based on the data from National Family Health Survey-3 (NFHS-3, 2005-06), India falls under “Severe public health problem” category in WHO Classification as almost all population groups have prevalence of anaemia levels which are above 40 percent. In countries where the anaemia control programs have already been successful to curtail the prevalence to below 40 percent, this classification can be used to prioritise geographic areas and population groups for directing the programatic steps [14], whereas the above classification cannot serve the requirement of a programmatic indicator at this stage of anaemia control for India. A need was felt for such an indicator that helps to prioritise the states and districts for targeted approach by the program managers. Hence an attempt was made to categorise “Severe Public Health Problem” into grades of severity that will help in prioritising the states and districts for action.
The primary objective of this study was to adapt the WHO Classification of “Anaemia as a Problem of Public Health Significance” to India and such other countries which fall under “Category of Severe Public Health Significance”. The adapted classification will be used to identify the high risk population groups based on age, gender and pregnancy status for anaemia. and finally to map the states and districts of southern India based on anaemia prevalence.
Materials and Methods
Secondary data published in the District Level Household and Facility Survey-4 was analysed [15–20]. District Level Household and Facility Survey (DLHS) have been undertaken by the Ministry of Health and Family Welfare, Government of India with the main objective to provide reproductive and child health related database at district level in India. The data from these surveys have been useful in setting the benchmarks and examining the progress the country has made after the implementation of RCH programme. In addition, the evidence generated by these surveys has also been useful for the monitoring and evaluation of ongoing programmes and planning of suitable strategies by the central and state governments. The Ministry of Health and Family Welfare, Government of India, initiated the process of conducting DLHS-4 during 2012-2013 and has designated the International Institute for Population Sciences (IIPS) as the nodal agency to carry out the survey. Fieldwork in Andhra Pradesh was conducted during August 2013 to January 2014, gathering information from 20,490 households, 16,498 ever married women and also from 1,040 health facilities [15]. Fieldwork in Karnataka was conducted during December 2012 to October 2013, gathering information from 47,200 households, 44,028 ever married women and also from 2,155 health facilities [16]. Fieldwork in Kerala was conducted during April 2013 to February 2014, gathering information from 20,089 households, 13,780 ever married women and also from 539 health facilities [17]. Fieldwork in Puducherry was conducted during September 2013 to March 2014, gathering information from 5,210 households, 4,549 ever married women and also from 78 health facilities [18]. Fieldwork in Tamil Nadu was conducted during March 2013 to February 2014, gathering information from 46,084 households, 38,693 ever married women and also from 2,108 health facilities [19]. Fieldwork in Telangana was conducted during June 2013 to February 2014, gathering information from 13,927 households, 12,432 ever married women and also from 587 health facilities [20]. Anaemia prevalence was assessed in 11 population groups including Children (6-59 months); Children (6-9 Years) Male; Children (6-9 Years) Female; Children (6-14 years) Male; Children (6-14 years) Female; Children (10-19 Years) Male; Children (10-19 Years) Female; Adolescents (15-19 years); pregnant women (15-49 aged); Women (15-49 aged) and Persons (20 years and above). Anaemia was defined as haemoglobin levels below 11g/dl. Severe anaemia was defined as haemoglobin levels below 7g/dl.
“Severe Public Health Problem” category in the WHO classification [13] has been adapted to Grade Anaemia as a severe public Health problem into three grades [Table/Fig-1].
Gradation of severe public health problem (SPHP).
| Prevalence of anaemia (%) | Graded Category of public health significance |
|---|
| 40.0-59.9 | Grade 1 SPHP |
| 60.0-79.9 | Grade 2 SPHP |
| ≥ 80.0 | Grade 3 SPHP |
The Five states and One Union Territory (six territories) in the southern part India were included in the analysis (Andhra Pradesh, Karnataka, Kerala, Tamil Nadu, Telangana States and Puducherry UT) based on the data that is published by the Ministry of Health and Family Welfare, Government of India [21]. Data on individual states was pooled and the overall anaemia prevalence in the six territories is used to rank the priority population groups. Mapping of high risk states and districts was done for children 6 months to 59 months age group as it is the group with highest prevalence of anaemia. Statistical analysis was done using Microsoft Office Excel 2007. Proportions are used to depict prevalence. Choropleth Mapping was done to visually depict the intensity of anaemia problem across the geographic territories like districts and states [22].
Results
High risk population groups based on age, gender and pregnancy status for anaemia [
Table/Fig-2]
Ranking the high risk population groups based on prevalence of anaemia.
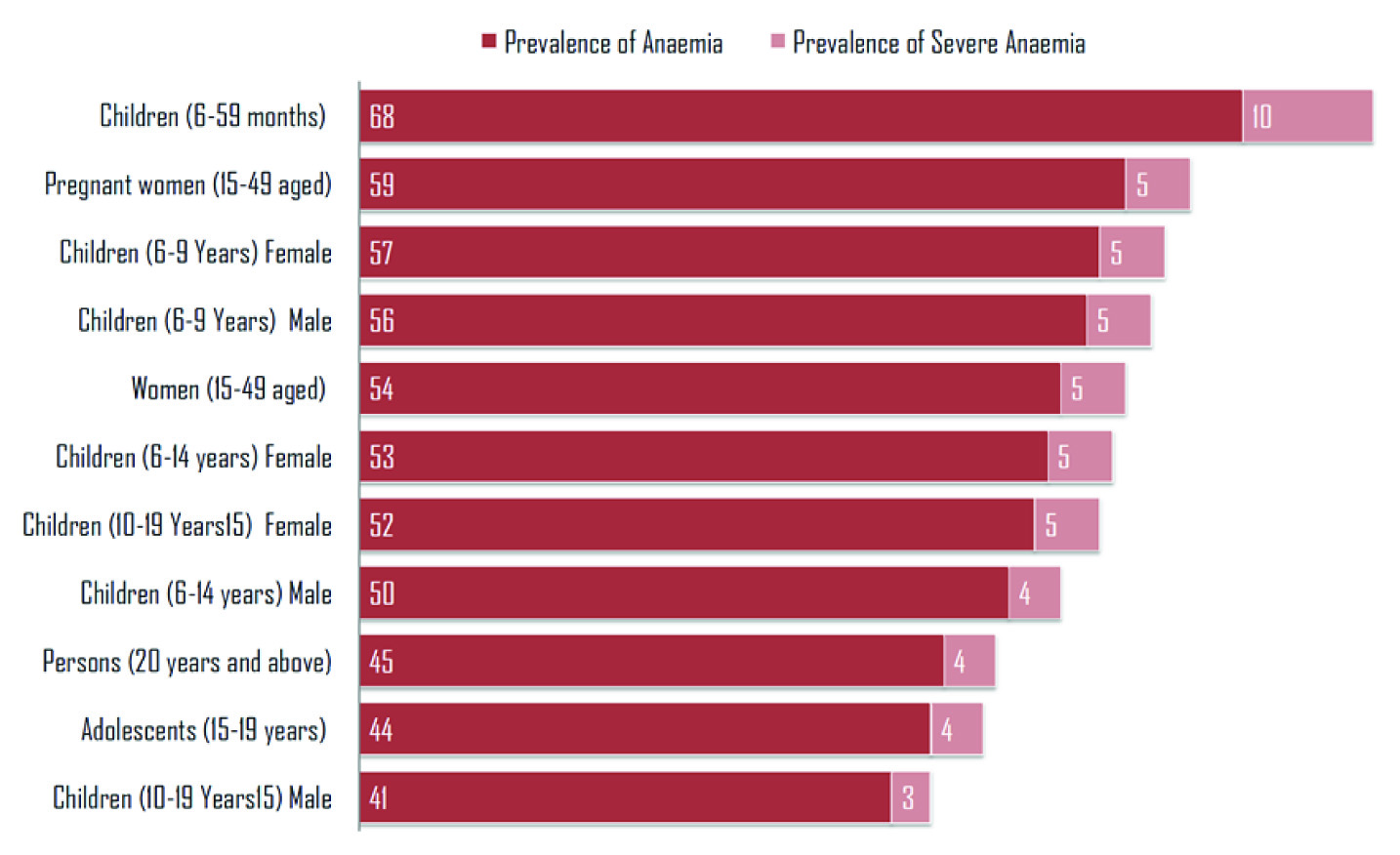
Among the various population groups the most vulnerable were the children 6 months to 59 months having highest prevalence of both, anaemia (68%) and severe anaemia (10%). This was followed by Pregnant Women aged 15 to 49 years (59%), Girl Child 6 to 9 years (57%), Boys 6 to 9 years (56%), women aged 15 to 49 years (54%), Girls 6 to 14-year-old (53%) and Girls 10 to 19 years (52%). Boys in the age group of 10-19 years have lowest prevalence of anaemia of 41 percent.
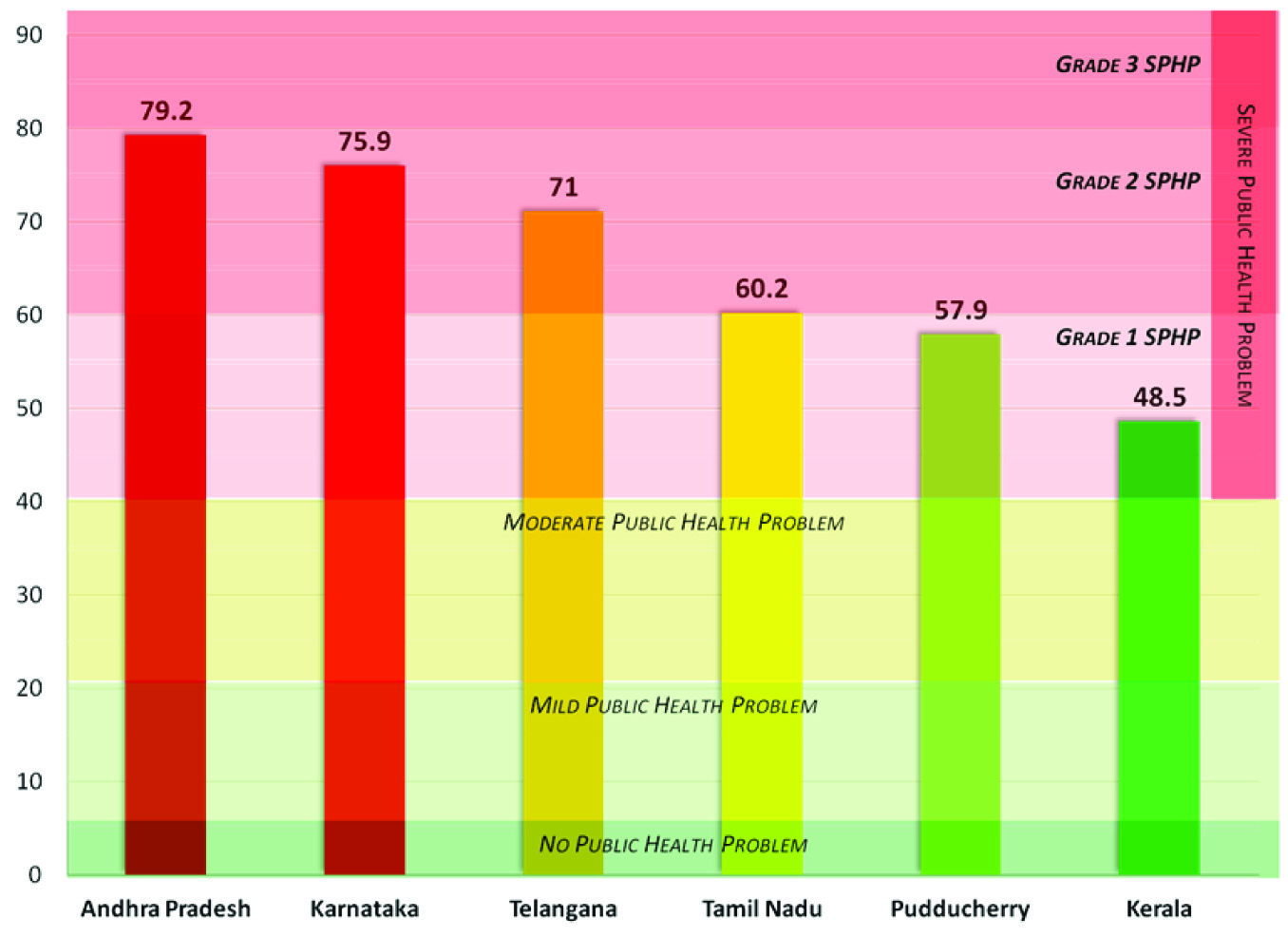
Mapping and grading the states and districts based on anaemia prevalence [
Table/Fig-3,
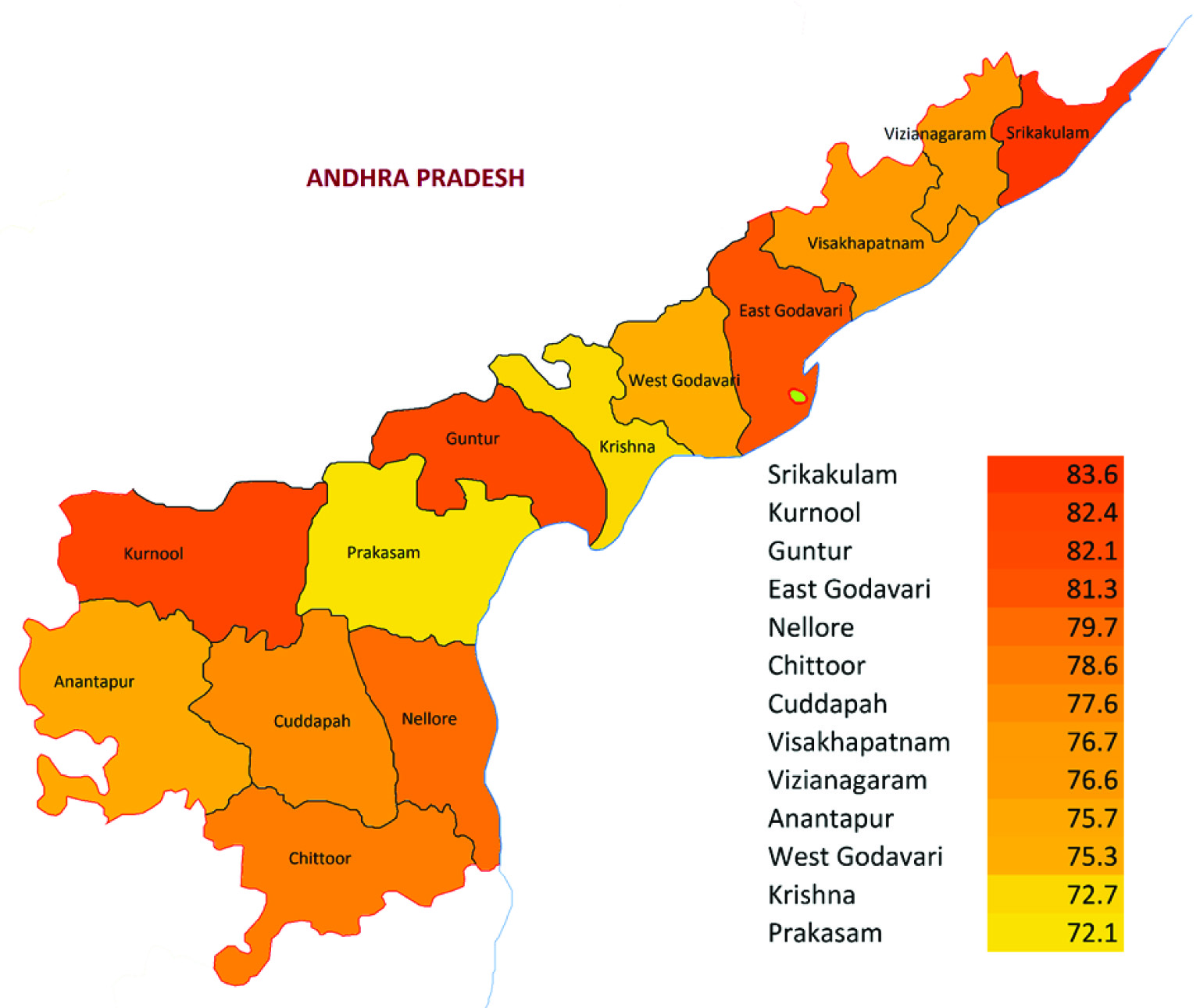
4,
5,
6,
7 and
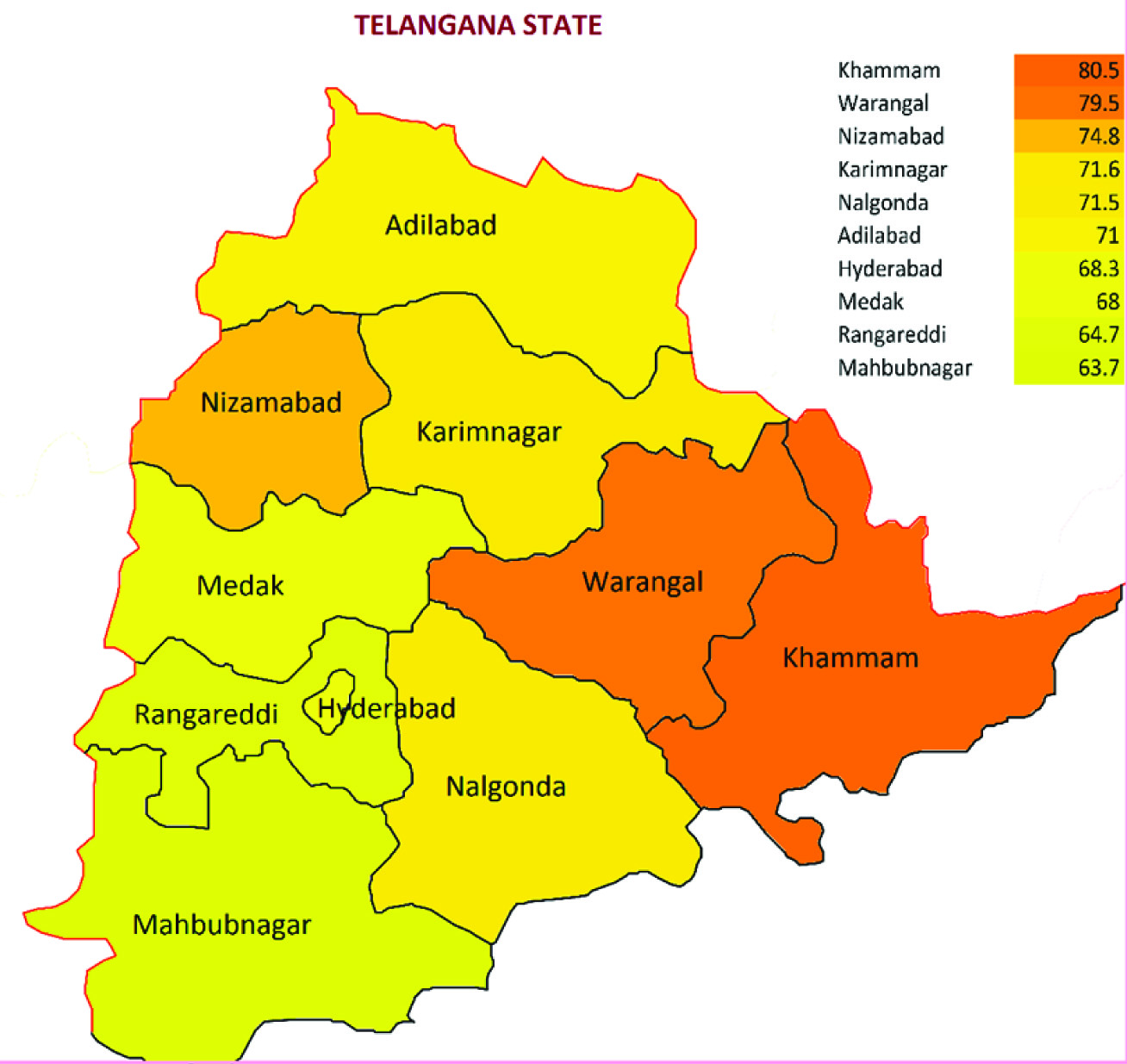
8]
Ranking & grading the south indian states based on prevalence of anaemia.
Choropleth mapping of districts of andhra pradesh state based on prevalence of anaemia in the 6-59 months age children.
Choropleth mapping of districts of karnataka state based on prevalence of anaemia in the 6-59 months age children.

Choropleth mapping of districts of kerala state based on prevalence of anaemia in the 6-59 months age children.

Choropleth mapping of districts of tamilnadu state based on prevalence of anaemia in the 6-59 months age children.

Choropleth mapping of districts of telangana state based on prevalence of anaemia in the 6-59 months age children.
Four of the Southern states of India fall in the Grade 2 SPHP, which include Andhra Pradesh, Karnataka, Tamil Nadu and Telangana. Pudducherry and Kerala fall in the Grade 1 SPHP [Table/Fig-3].
In the state of Andhra Pradesh 4 districts, Srikakulam, Kurnool, Guntur and East Godavari are Grade 3 SPHP while rest of 9 districts fall under Grade 2 SPHP [Table/Fig-4].
In the state of Karnataka, 11 out of 30 districts fall under Grade 3 SPHP Category including Ramanagara, Banglore Rural, Chikkaballarpura, Mandya, Yadgir, Banglore, Kolar, Mysore, Chamaranjangar, Chickmanglur and Bellary. Eighteen Districts fall under Grade 2 and 1 district, Dharwad falls under WHO mild public health problem [Table/Fig-5].
In the state of Kerala, out of the 14 districts, 8 districts have no data. Of the remaining 6 districts, 1 district (Kollam) falls in Grade 2 SPHP, 4 districts Kozhikode, Alappuzha, Thiruvananthapuram and Ernakulam fall in Grade 1 SPHP and Thrissur falls in WHO moderate public health problem category [Table/Fig-6].
Out of the 4 districts of Pudducherry State, Mahe and Pondicherry fall under Grade 2 SPHP. Karaikal and Yanam Grade 1 SPHP.
In the state of Tamilnadu, out of the 32 districts, 17 districts Ariyalur, Karur, Dindigul, Khancheepuram and others fall under Grade 2 SPHP and the remaining 15 districts fall under Grade 1 SPHP [Table/Fig-7].
In the New state of Telangana, Khammam is the only Grade 3 district, while rest of the 9 districts including the capital Hyderabad fall under Grade 2 SPHP [Table/Fig-8].
Discussion
Overall, the three population groups most vulnerable to anaemia include preschool-age children (6–59 months), pregnant women (15–49 years of age) and girls and boys in the 6-9 years age followed by non-pregnant women (15–49 years of age).
For the year 2011, WHO has estimated that roughly 43% of children, 38% of pregnant women, and 29% of non-pregnant women and 29% of all women of reproductive age have anaemia globally, corresponding to 273 million children, 496 million non-pregnant women and 32 million pregnant women [23].
As per DLHS 4 the prevalence in Southern States of India is much higher. The prevalence is 68% in pre-school children, 59% pregnant women, 58% 6 to 9 years age group children and 56 percent in 15 to 49 years women. If the adapted Grading method may be applied, Pre-school children may be graded as Grade 2 Severe Public Health Problem and others Grade 1 Severe Public Health problem.
The state of Andhra Pradesh and Karnataka require immediate programmatic interventions. The state of Andhra Pradesh (79.2 percent anaemia) can slip to Grade 3 Severe Public Health Problem if no appropriate intervention is taken. The state of Karnataka with 11 of its districts in Grade 3 Severe Public Health Problem has a huge burden of anaemia. The diverse reasons to address local issues need to be addressed.
Correcting anaemia calls for an integrated approach which should be based on identification of the contributing factors and addressing them. Factors beyond Iron deficiency like low blood haemoglobin concentrations may be caused by inadequate bioavailability of dietary iron, folic acid and/or vitamin B12. Genetic traits like sickle cell anaemia thalassaemias and infections like malaria, schistosomiasis, hookworm, or Human Immunodeficiency Virus (HIV) infections; and some non-communicable diseases need to be explored especially in high risk states and districts [5,24,25]. In territories and populations where a higher proportion of anaemia and severe anaemia is caused by non-iron causes (like Europe and the Americas), it was found that the proportion of anaemia amenable to iron as 42% and 50% in children and women respectively. Perversely, the proportion of anaemia amenable to iron was lower in populations where other factors contribute to anaemia (SEARO and African regions of WHO) [23]. Harrison’s principles of Internal Medicine enumerate three major causes of iron deficiency which include decrease in iron intake or absorption, increase iron loss and increase demand for iron. Decreased iron absorption is seen in inadequate diet; malabsorption from disease (sprue, Crohn’s disease); malabsorption from surgery (post-gastrectomy) and acute or chronic inflammation. Increased iron loss is seen in chronic blood loss; menses; acute blood loss; blood donation and phlebotomy. Increased demand for iron and/or haematopoiesis is seen in rapid growth; in infancy or adolescence; pregnancy and erythropoietin therapy [26].
Iron deficiency anaemia should ideally be addressed through dietary variegation and improved access to foods that have high levels of bio-available iron, including animal products. Daily or intermittent iron supplementation, alone or together with folic acid and other micronutrients, can be used for high-risk groups (children, pregnant women and women of reproductive age), to improve iron intakes [4,27–30]. However, supplementation programmes need to address challenges that have trammeled their effectiveness, such as poor attendance at antenatal clinics, insufficient doses for supplementation, or insufficient emphasis on behavioral aspects of using supplements on a regular basis [31]. Other food based approaches, such as fortification of staple foods and condiments can also be used to improve iron intake in the general population [32,33]. Fortification of wheat flour with iron and other vitamins and minerals is currently mandated in 80 countries but the extent of coverage varies [34]. As anaemia is a multi-thronged public health problem, the current control strategies in place need as well to be adapted and integrated to address the contributory factors in an integrated manner. For example, in territories where Malaria is an endemic disease, an integration of malaria case management and iron supplementation is required. It was demonstrated that malaria control programs in endemic zones has contributed to reduction in anaemia by 25 percent and severe anaemia by 60 percent. The haemoglobin concentrations have bettered in pregnant women and the children following preventive strategies like providing insecticide impregnated bed nets and intermittent preventive treatment [35]. There is also an increased need for improved water and sanitation and de-worming in populations affected by hookworms and schistosomiasis; these populations typically live in rural tropical regions with poor sanitation facilities, especially in Indian sub continent.
Limitation
As the study is based on secondary data, though it is very cost-effective, lack of control on data collection, compilation and collation can affect the validity and reliability of the findings in the study. However the chances for such a deviation are minimal as District Level Household and Facility Survey (DLHS) has been undertaken by the Ministry of Health and Family Welfare, Government of India in a controlled way.
Recommendations
The preschool children in the southern states of India have an unacceptably high prevalence of Anaemia. The Government of India has launched Rashtriya Bal Swasthya Karyakram (RBSK) in the National Health Mission. It is aimed at early identification of diseases and early intervention for children from birth to 18 years. RBSK has its focus on four issues including Defects at birth, Development delays (including disability), Deficiencies and Diseases [36]. The vulnerable population groups and territories require priority in the Government of India’s RBSK in the National Health Mission to address iron deficiency anaemia. Reducing anaemia among women is the second global nutrition target for 2025. The target is a 50% reduction of anaemia in women of reproductive age [37]. The problem needs to be addressed through dietary diversification and improved access to foods that have high levels of bioavailable iron, including animal products apart from Iron supplementation. All the 16 districts that fall under Grade 3 Severe Public Health Problem in the states of Andhra Pradesh, Karnataka and Telangana require special focus for identifying and addressing the determinants of such high prevalence of anaemia. A combination of key programmes that address the determinants of low blood haemoglobin concentrations will be required to make a significant impact. These strategies should be tailored to local conditions, based on specific aetiology and prevalence of anaemia in a given setting and population group. The interventions should be built into the primary health-care system and existing programmes to improve insure sustainability. In the year 2013, Ministry of Health and Family Welfare, GOI launched the National Iron Plus Initiative (NIPI) as a comprehensive strategy to combat the public health challenge of iron deficiency anaemia prevalent across the life cycle, There are age specific interventions with IFA supplementation and deworming for improving the haemoglobin levels and reducing the prevalence of anaemia for all age groups [38].
Conclusion
The vulnerable population groups for anaemia keyed out in this study are the Children 6 months to 59 months; Pregnant Women aged 15 to 49 years and Girl Child 6 to 9 years. Four of the Southern states of India including Andhra Pradesh, Karnataka, Telangana and Tamil Nadu fall in the Grade 2 SPHP (Severe Public Health Problem). Sixteen districts fall under Grade 3 Severe Public Health Problem in the states of Andhra Pradesh, Karnataka and Telangana. Choropleth Mapping is a vibrant way to display territories that require priority in anaemia control.