Multiple Myeloma: An Unusual Cause of Extensive Bone Marrow Necrosis
Rashi Sharma1, Smeeta Gajendra2, Swachi Jain3, Sunil Kumar Gupta4, Ritesh Sachdev5
1 Senior Resident, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Sector – 38, Gurgaon, Haryana, India.
2 Associate Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Sector – 38, Gurgaon, Haryana, India.
3 Junior Resident, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Sector – 38, Gurgaon, Haryana, India.
4 Consultant, Department of Hematology and Medical Oncology, Medanta-The Medicity, Sector – 38, Gurgaon, Haryana, India.
5 Senior Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Sector – 38, Gurgaon, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ritesh Sachdev, Senior Consultant, Department of Pathology and Laboratory Medicine, Medanta-The Medicity, Sector – 38, Gurgaon, Haryana-122 001, India.
E-mail: sachdev05@gmail.com
Bone marrow biopsies, Fatal complication, Hematological malignancy
Sir,
Bone Marrow Necrosis (BMN) is an unusual but fatal complication accounting less than 1% of bone marrow biopsies [1,2]. It is described morphologically as necrosis of marrow tissue along with medullary stroma and fat spaces with preservation of bone [3]. It usually presents as fever, bone pain, pancytopenia, leucoerythroblastic picture with elevated LDH and alkaline phosphatase [2–5]. BMN is either idiopathic or is associated with various diseases, commonly hematolymphoid malignancies like chronic myeloproliferative disorders, acute leukaemia, lymphoma and multiple myeloma. It is commonly seen in the setting of chemotherapy and during treatment with retinoic acid, fludarabine, interferon-α and granulocyte-colony-stimulating-factor. Other conditions associated with BMN are sickle cell anemia, solid tumours, metastatic carcinoma, parvovirus, Human immunodeficiency virus, antiphospholipid syndromes. Certain medications like paracetamol, sulfasalazine, interferon and imatinib can also induce marrow necrosis [4]. Herein we described a case of Multiple myeloma (MM) with extensive BMN at the time of initial presentation, which is very rare and only few cases have been described in the literature [2,4].
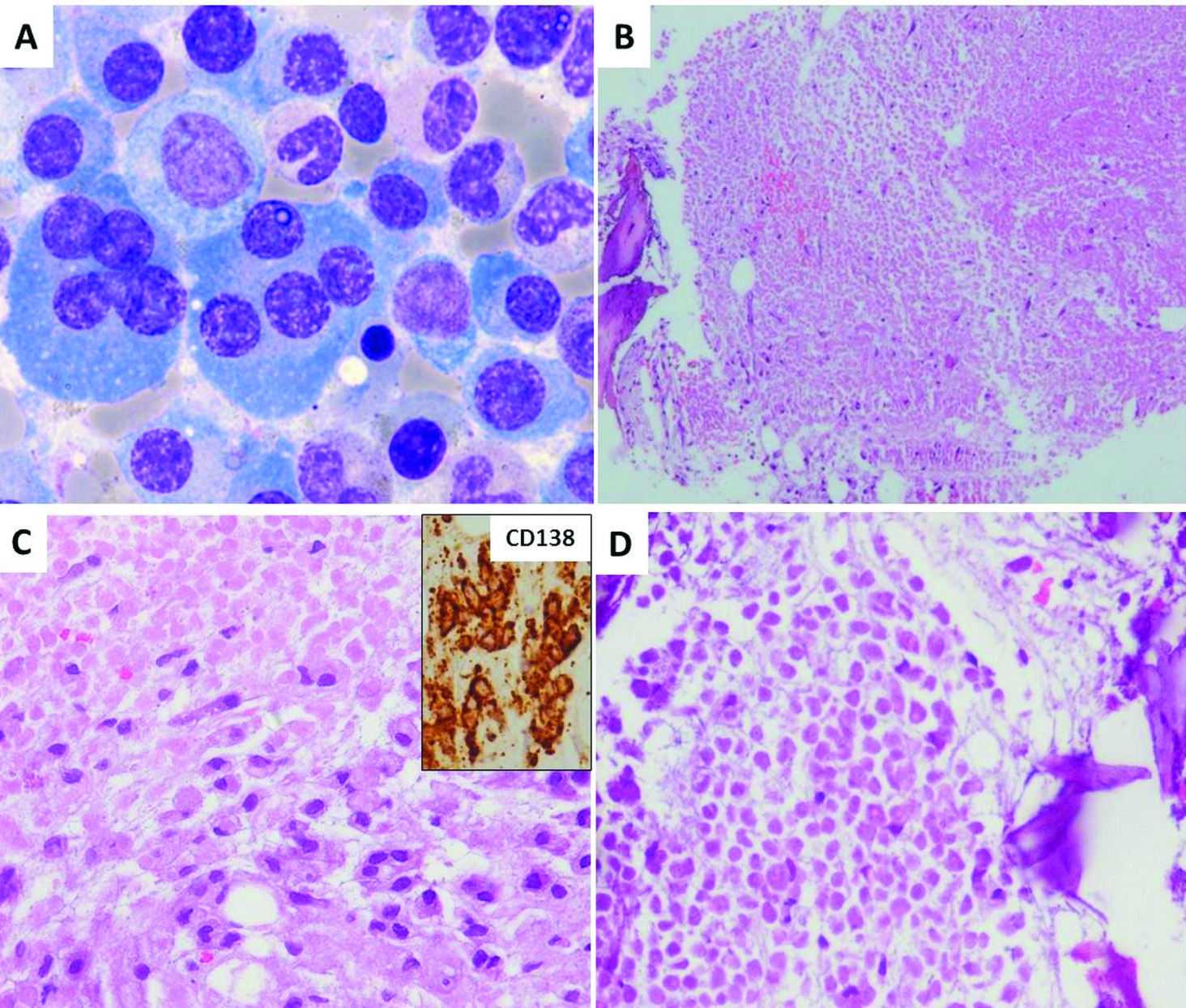
A 61-year-old male presented with back pain since 7 months. Peripheral blood smear revealed normocytic normochromic blood picture with mild leucopenia (total leucocyte count: 3.7x109/L). Bone marrow aspirate showed cellular marrow with infiltration by 64% plasma cells including abnormal forms [Table/Fig-1a]. Bone marrow biopsy exhibited sheets of plasma cells with extensive areas of coagulative necrosis; involving approximately 75 to 80% of the bone marrow [Table/Fig-1b-d]. CD-138 (Dako, MI 15) showed sheets of plasma cells with kappa (Biogenix, L1C1) light chain restriction. CK (Biogenix, AE1 and AE3) was negative. AFB stain was negative. The serum free light chain assay showed abnormally high levels of kappa light chain (>1650mg/L). Non-contrast Computed Tomography demonstrated diffuse osteopenia with multiple ill-defined lytic lesions in the dorso-lumbar vertebral body, posterior elements and pelvic bone. There was no evidence of other causes of BMN like infections, DIC or drug intake. Vertebroplasty was done and he was started on chemotherapy with bortezomib, cyclophosphamide and dexamethasone. After two cycles of chemotherapy, he was in stringent complete remission. The complete blood count, renal function test and liver function test were within normal range. The serum free light chain assay was normal with free Kappa 14.0 mg/L (normal range: 3.3-19.4), Lambda 14.6 mg/L (normal range: 5.71-26.30) and ratio of 0.959. The patient tolerated three cycles of chemotherapy well with acceptable blood indices. Thalidomide was added and the patient was counseled for further treatment including consolidation with auto Peripheral Blood Stem Cell Transplantation (PBSCT) followed by maintenance therapy.
Bone marrow aspirate smear showing infiltration by abnormal plasma cells (a). Bone marrow biopsy showing sheets of plasma cells with extensive areas of coagulative necrosis; involving approximately 75 to 80% of the bone marrow (b-d) with plasma cells showing CD 138 (Dako, MI 15) positivity (C, inset).
BMN is usually an unrecognized finding in routine bone marrow biopsy. According to the extent of involvement, BMN is classified into minor (grade I) involving <20% of BM, intermediate (grade II) involving 20-50% of the BM and severe (grade III) >50% of the BM. The pathogenesis is not clear. The common hypothesis involves the role of bone marrow microenvironment with elevated TNF-alpha and interleukin 6-(IL-6) which leads to bone marrow endothelial cell injury with subsequent microvascular occlusion and necrosis [4]. BMN in multiple myeloma is very rare [4]. Both the MM cells and/or stromal cell secrete multiple cytokines including IL-6 and TNF-a. Only three cases have been described in the literature till date [2,4]. Zhu et al., described two cases of BMN in patients at the time of relapse with MM [4]. Their clinical presentations were typical of BMN as bone pain, increased alkaline phosphatase, and marked elevated LDH level associated with characteristic BM findings on biopsy. Prompt initiation of therapy in his patients resulted in complete restoration of haematopoiesis, relief of bone pain and normalization of LDH, and phosphate levels as seen in the present case. He suggested that the high tumour burden in these two patients in relapse was associated with high expression of TNF-a in the BM microenvironment, which subsequently led to the endothelial injury, resulting in the development of BMN. Eishi et al., described one case of grade II bone marrow necrosis in a case of MM at the time of initial presentation as in our case [2]. His patient underwent treatment for MM, but two months later he developed altered mental and succumbed due to anemia and organ failure. The importance of recognizing marrow necrosis in multiple myeloma lies in the fact that it can be reversible if immediate therapeutic intervention is initiated. BMN is a rare antemortem finding which may obscure the diagnosis and associated with poor prognosis, especially in haematologic malignancies [4,6]. Extensive BMN associated with haemotologic malignancies is almost invariably a fatal complication, however with prompt identification and treatment with chemotherapy and supportive care, the prognoses of these patients can be improved.
[1]. Wool GD, Deucher A, Bone marrow necrosis: ten-year retrospective review of bone marrow biopsy specimensAm J Clin Pathol 2015 143(2):201-13. [Google Scholar]
[2]. Eishi A, Ilkhanizade B, Rahimi E, Bone marrow necrosis: frequency and clinicopathological findings in marrow biopsiesIranian Journal of Pathology 2009 4(1):38-43. [Google Scholar]
[3]. Corti M, Soto I, Villafañe MF, Minué G, Campitelli A, Narbaitz M, Bone marrow necrosis as clinical presentation of plasmablastic lymphoma in an AIDS patient: First case reported and literature reviewJournal of Haematological Malignancies 2013 3(1):57-62. [Google Scholar]
[4]. Zhu AX, Niesvizky R, Hedrick E, Fata F, Filippa DA, Michaeli J, Extensive bone marrow necrosis associated with multiple myelomaLeukaemia 1999 13(12):2118-20. [Google Scholar]
[5]. Ozkan A, Ozkalemkas F, Ali R, Ozkocaman V, Ozcelik T, Severe bone marrow necrosis without suggestive featuresAm J Haematol 2006 81(5):386-87. [Google Scholar]
[6]. Badar T, Shetty A, Bueso-Ramos C, Cortes J, Konopleva M, Borthakur G, Bone marrow necrosis in acute leukaemia: Clinical characteristic and outcomeAm J Haematol 2015 90(9):769-73. [Google Scholar]