Prescription order is an important therapeutic transaction between physician and patient, as it brings into focus the diagnostic acumen and therapeutic proficiency of physician with instructions for restoration of patient’s health. The most carefully conceived prescription orders may become therapeutically useless, however, unless it communicates clearly with pharmacist and adequately instructs patient on how to take prescribed medication [1]. Prescriptions are medico-legal documents which need to be written legibly, accurately and completely [2]. Moreover a good quality prescription is an extremely important factor for minimizing errors in dispensing medication and it should be adherent to guidelines for prescription writing for benefit of the patient [3].
On the other hand prescription errors may lead to adverse events which may be largely preventable [4]. Thus “A clinically meaningful prescribing error occurs when, as a result of a prescribing decision or prescription writing process, there is an unintentional significant (1) reduction in probability of treatment being timely and effective or (2) increase in the risk of harm when compared with generally accepted practice” [5]. Although it is difficult to quantify precisely the extent of prescription errors, they are frequent and often avoidable representing a major threat to patient safety. While in India prescription errors rates reported in a range between 17.6% to 44.18% [6], which depend largely on, types of different study methods used.
Since prescribing is one of the common tasks in daily general practice, there seems abundant evidence of continuous poor prescribing worldwide [7,8]. Prescription errors account for 70% of medication errors that could potentially result in adverse effects [9].
In India, conventional or traditional prescribing methods i.e. hand written on a prescription blank are still prevalent. Development of ability to write and dispense a complete and unambiguous prescription(s) consistently is an essential part of medical care training process, yet often neglected. Errors will always occur in any system, but it is essential to identify causes and attempts to minimize risk. This study is an effort directed to find out errors in prescription writing and interventions to improve upon such error prone practices of prescription writing.
The objective of this study was to evaluate the frequency and types of prescription errors in outpatient prescriptions and to find whether prescription writing abides with WHO standards of prescription writing.
Materials and Methods
This was a cross-sectional, observational study. Prior ethical permission was taken. Clinicians participating in study were informed about objectives of study and their written informed consent was taken. Prescriptions were collected from three local pharmacy stores of Anand city over a period of May 2008 to January 2010*. Collection of prescriptions was started a month after the consent to minimize bias in prescription writing.
The prescriptions were collected in two forms – Handwritten and Computerised. Available prescriptions were either photocopies or scans of original document presented by the patients at local pharmacy stores or in some cases as duplicate printouts of computer generated prescriptions. Allopathic private practitioners practising at Anand city of different specialities were included in study e.g. Physicians, Surgeons, Paediatricians, Otolaryngologists, Opthalmologists, Orthopaedic surgeons, Chest Physicians, Dermatologists, Psychiatrists and General Practitioners while institutional prescriptions and corporate hospital prescriptions were excluded from study.
The prescription copies so obtained were analysed as per WHO guidelines for “Prescription Writing Errors” [2]. A checklist was prepared and each prescription was analysed on various parameters given below:
Patient details: Name, age, sex, weight, address and date of prescription.
Clinician details: Qualification, address, registration number and signature.
Drug details: Mention of generic or brand name, dosage form, route, dose, unit, frequency, duration of treatment, quantity, signa.
Other information: Mention of allergy status, specific drug communication, mention of abnormality in liver/kidney/cardiac condition, refill mentioned or not, dispense as written, follow up, history of intake of other medicines and legibility status of the prescription.
Statistical Analysis
Descriptive statistics was performed to estimate the errors in handwritten and computer generated prescriptions. The data were expressed as numbers and percentages.
Results
Total number of prescriptions collected was 749. Of these, 549 were handwritten (73.29%) and 200 were computer generated (26.70%).
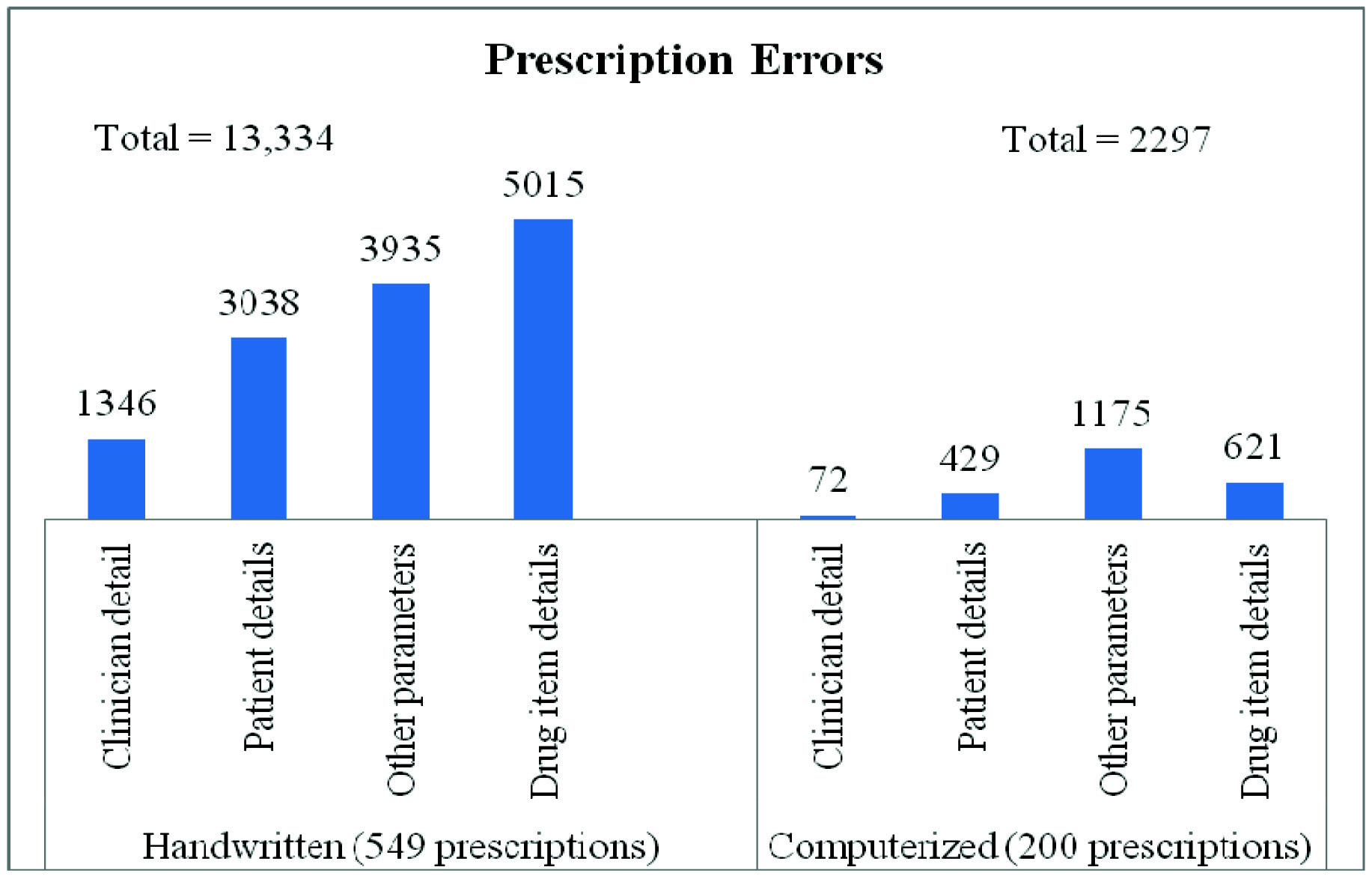
Out of 549 handwritten prescriptions, total of 13,334 errors were found in various parameters regarding clinicians detail, patient details, drug item details and others. While there were total 2297 errors found in similar context out of 200 computerized prescriptions [Table/Fig-1,2].
Frequency of overall prescription errors in different parameters in handwritten and computerized prescriptions
Number and frequency of prescription errors in clinicians’ and patient’s details in handwritten and computer generated prescriptions.
| Sr. No. | | Handwrittenn= 549 (%) | Computerizedn= 200 (%) |
|---|
| A | Clinician detail | Mentioned | Errors(Not mentioned) | Mentioned | Errors(Not mentioned) |
|---|
| 1 | Name | 549 (100) | 0 | 200 (100) | 0 |
| 2 | Qualification | 525(95.63) | 24 (4.37) | 200 (100) | 0 |
| 3 | Contact No. | 0 | 549 (100) | 164 (82) | 36(18) |
| 4 | Address | 544 (99.09) | 5 (0.91) | 200 (100) | 0 |
| 5 | Registration No. | 94 (17.12) | 455(82.88) | 200 (100) | 0 |
| 6 | Esoteric symbol | 423 (77.05) | 126 (22.95) | 200 (100) | 0 |
| 7 | Signature | 361 (65.76) | 188 (34.24) | 164 (82) | 36(18) |
| Total | | 1347 | | 72 |
| B | Patient details | Mentioned | Errors(Not mentioned) | Mentioned | Errors(Not mentioned) |
| 1 | OPD No. | 34 (6.19) | 515(93.81) | 200 (100) | 0 (0) |
| 2 | Name | 477 (86.89) | 72(13.11) | 200 (100) | 0 (0) |
| 3 | Age | 140 (25.50) | 409(74.50) | 200 (100) | 0 (0) |
| 4 | Sex | 95 (17.30) | 454(82.70) | 200 (100) | 0 (0) |
| 5 | Weight | 62 (11.29) | 487(88.71) | 171 (85.5) | 29 (14.5) |
| 6 | Address | 51 (9.29) | 498(90.71) | 0 (0) | 200 (100) |
| 7 | Contact No. | 0 (0) | 549(100) | 0 (0) | 200 (100) |
| 8 | Date of prescription | 495 (90.16) | 54(9.84) | 200 (100) | 0 (0) |
| Total | | 3038 | | 429 |
Total number of drugs prescribed by generic name are 55 (2.97%) in handwritten while 03 (0.50%) in computerized prescriptions. Rest 1799 (97.03%) and 592 (99.50%) drugs were prescribed by brand name in hand written and computerized prescriptions respectively [Table/Fig-3,4].
Number and frequency of prescription errors in drug item details of all drugs prescribed on Handwritten and computerized prescription.
| Sr. No. | Drug item details | Handwrittenn= 1854 (%) | Computerizedn= 595 (%) |
|---|
| Mentioned | Errors(Not mentioned) | Mentioned | Errors(Not mentioned) |
|---|
| 1 | Route | 1449(78.15) | 405(21.84) | 435(73.10) | 160(26.89) |
| 2 | Dosage form | 1434(77.34) | 420(20.65) | 435(73.10) | 160(26.89) |
| 3 | Dose | 876(47.24) | 978 (52.75) | 519(87.22) | 76(12.77) |
| 4 | Unit | 258(13.92) | 1596(86.08) | 434(72.94) | 161(27.05) |
| 5 | Frequency of administration | 1438(77.56) | 416(22.44) | 567(95.29) | 28(4.70) |
| 6 | Duration of treatment | 1352(72.92) | 502(27.08) | 567(95.29) | 28(4.70) |
| 7 | Signa | 1156(62.35) | 698(37.65) | 567(95.29) | 28(4.70) |
| Total | | 5015 | | 621 |
Number and frequency of prescription errors in other parameters in handwritten and computer generated prescriptions.
| Sr. No. | Other parameters | Handwrittenn= 549 (%) | Computerizedn= 200 (%) |
|---|
| Mentioned | Errors(Not mentioned) | Mentioned | Errors(Not mentioned) |
|---|
| 1 | Allergy | 0 (0) | 549 (100) | 0 (0) | 200 (100) |
| 2 | Specific drug communication | 0 (0) | 549 (100) | 6 (3.00) | 194 (97.00) |
| 3 | Status: CVS/RS/L/K* | 0 (0) | 549 (100) | 0(0) | 200 (100) |
| 4 | Dispense as written | 0 (0) | 549 (100) | 33 (16.50) | 167 (83.5) |
| 5 | Follow-up | 42 (7.65) | 507 (92.35) | 186 (93.00) | 14 (7) |
| 6 | H/O intake of other medicine | 0 (0) | 549 (100) | 0(0) | 200 (100) |
| 7 | Legible handwriting | 415 (75.59) | 134 (24.41) | 200 (100) | 0 (0) |
| 8 | Refill mentioned | 0 (0) | 549 (100) | 0 (0) | 200 (100) |
| Total | | 3935 | | 1175 |
*CVS/RS/L/K- Cardiovascular, Respiratory, Lung, Kidney condition of patient.
Discussion
In this study total 749 prescriptions were collected. All prescriptions were screened for the essential elements of prescription writing [2]. Name of doctor was mentioned in all handwritten prescriptions in the given study i.e. 100% while their qualifications mentioned in 95.60%, findings were similar to study by Di Paolo ER et al., which stated that prescriber’s name and qualifications were mentioned in 99.5% of the prescriptions [10]. While in a study conducted by Irshaid et al., in hospitals of Saudi Arabia it was found that 17% prescriptions did not bear the name of the prescriber [11]. In light of this finding, prescriptions can be rendered illegal, if they don’t bear the doctor’s name. Such type of deficiencies can pose a major difficulty for dispensing pharmacist to contact the prescriber in case he/she needs any clarification from prescriber in regards to details of drug prescribed etc.
In this study, doctor’s contact address was mentioned in 99.27% of handwritten prescriptions while none of the prescriptions mentioned any hospital contact numbers. On the other hand, Irshaid et al., study revealed that only 9.6% prescriptions had doctors address while none had hospital contact numbers [11]. Missing out such information needs to be taken care, as any error of omission or commission if detected by a pharmacist can be avoided or an instruction not clearly understood by patient can be clarified if the prescriber is just phone call away.
In present study, doctor’s registration number was mentioned in only 17.12% of handwritten prescriptions. On the contrary it was mentioned in 99.06% prescriptions in a study done by Ansari et al., [12]. According to information regarding medical council registration number, doctors are required to quote their registration number on all medical prescriptions, reports, documentation and records; whether in paper or electronic format relating to their medical practice. Thus doctor should put his rubber stamp bearing his full name, qualification and registration number. This requirement arises from section number 43 [8] of the Medical Practitioner Act 2007 and comes in with the annual certificate of registration by the Medical Council of India [13].
Doctor’s signature was present in 65.75% of handwritten prescriptions in this study, as compared to study by Wilson et al., were in 96% prescriptions bore doctors signature [14]. On the contrary, study by Ansari et al., had doctor’s signature in only 15.7% prescriptions [12]. If prescriptions do not carry doctor’s sign then the validity and authenticity of prescriptions can be questioned by pharmacist and other doctors to whom prescriptions are referred, thereby raising major legal issues.
The date of issue of prescription to the patient was not mentioned in 9.83% of handwritten prescriptions in present study, whereas study conducted by Siddarth et al., reported the absence of date in 0.7% [15]. The mention of date signifies the fact that a medical consultation was sought and action was taken by clinician for ailment. Since treatment protocols follow a certain set of algorithms, the mention of date is essential to access the prognosis as well it is important for legal matters in case of mortality. This can have serious implications in medico-legal cases since the prescription is a legal document and not mentioning date can be taken as negligence even in non-medico-legal cases.
OPD number was mentioned in only 31.24% of handwritten prescriptions, clearly illustrating a lack of serial case recording for future easy access to old case records if required.
Patient’s name was not mentioned in 13.11% of handwritten prescriptions (only 34.01% had the full name, while partial name in 56.38%). Study conducted in India, by Siddarth et al., reported that patient’s name was absent in 0.7% prescriptions [15]. It is imperative to mention full name of the patients as it restores the correct identity of the recipients and helps in reducing medication error because there can be more than one person with same name.
Also patient’s age was not mentioned in 74.5% of handwritten prescriptions. Patient’s weight was mentioned only in 11.29% of handwritten prescriptions which is an important part of superscription. According to WHO the inclusion of weight is recommended and should be included in prescription especially at the extremes of ages [2,16]. Weight is an important piece of information since it has implications on pharmacokinetics and pharmacodynamics. Lack of information on weight of child in prescriptions could lead to dispensing errors.
Address of patient is another important element that should be added in prescription according to WHO guidelines for better prescribing [2]. Herein patient’s address was mentioned in only 9.29% of prescriptions while patient’s contact number was not mentioned in any of handwritten the prescriptions. Also, there was lacunae in mention of address in a study conducted by Wilson et al., wherein patients address was mentioned in only 1.8% of prescriptions [14]. The name and contact number of patient can help in reminding follow-up and at times even to make corrections if errors of omission or commission are noticed by the clinicians before an unwanted event occurs.
In handwritten prescriptions of this study, just 2.97% drugs were prescribed by generic names while 97.63% were prescribed by brand names. This perhaps shows that clinicians have either more faith in a particular brand or they do not wish the pharmacist to have liberty to decide the brand. Besides, a majority of patients who were on chronic lifestyle disease management, like to remember their drugs by brand names which are much easy to recall as opposed to generic names. This finding is similar to study conducted by Kumari et al., at the tertiary health care level in eastern part of India i.e. in Lucknow district, which also depicted a very low generic prescribing (1.1%) [17]. Various studies done in other parts of India i.e. Kothari N et al., Hazra et al., Phalke et al., in this regard also had similar findings [18–20]. On the contrary, Biswas et al., reported that in outpatient prescription, 35% drugs were prescribed by generic names [21].
In present study the dosage form was mentioned in 77.34% while dose was mentioned in 47.25% of handwritten prescriptions. While study conducted at Maharashtra [20] and Jammu [22] reported that dose was not properly written approximately 35% and 25% respectively. Keeping this in mind, it is important for clinicians to remember that mention of dose or dosage form of medicines in prescriptions, is very important and particularly needed when a pharmaceutical product exists in more than one strength/dosage form. In this study, unit was mentioned in only 13.91% of handwritten prescriptions. The frequency of administration was mentioned in 77.56% of prescriptions and duration of medication was mentioned in 72.93% of handwritten prescriptions. However as compared to these findings, Phalke et al., reported that the dose, frequency, and duration of medication were missing in more than 25% prescriptions [20].
Signa/direction for drug use was mentioned in 62.35% of handwritten prescriptions. Study conducted by Irshaid et al., reported that prescriptions were seriously deficient in instructions for patient use and the majority of (90.7%) prescriptions contained only partial instructions while in only 2.3% of the prescriptions there were full instructions for patient use [11]. Numerous studies have demonstrated patient’s difficulty in recalling or understanding basic directions for taking the medicines. If the medication is to be taken at a specific time of the day, if a particular dosage interval is desired or if there are any additional directions for use, those should be noted on the prescription and precisely explained to the patient in simple terms. The presence of this information is of help to prevent dispensing errors.
Details like allergy, mention of medical condition like status of respiratory/hepatic/ renal/cardiac functioning as well as, history of intake of other medicines was not mentioned in any of the handwritten prescriptions. Clinicians should have the habit of mentioning all these important points in prescriptions. Mention of refill was not there in any of prescriptions. This is an interesting observation and perhaps partially explained by the fact that most clinicians are either uncomfortable with the patient taking medicines for long periods of time without regular follow-up checks as doses and drugs may need to be altered with changing patient physiology, prognosis and additional factors or perhaps have financial considerations not to mention refills. Follow-up was mentioned in 7.65% of prescriptions in this study. Specific drug communication or drug information was mentioned in barely 0.80% of handwritten prescriptions in this study, as compared to study done by Irshad et al., which reported that specific drug information was mentioned in 85% of prescriptions [11].
The computer generated prescriptions were less prone to errors than hand written ones. Almost all computer generated prescriptions contained 100% information on clinician details like name, qualification, address, registration number, esoteric symbol and the patient details like OPD number, name, age, sex of the patient. Similarly, in the drug item related prescriptions errors there was a marked reduction in the errors in areas like dose, unit, frequency of drug administration, duration of treatment, quantity, signa and legibility of prescriptions. On similar lines were the findings in a study done by Bates et al., which reports reduction in prescription errors in computer generated prescriptions [23]. In a study conducted by Bizovi et al., computer-assisted prescriptions at least three times less likely to contain errors and five times less likely to require pharmacist clarification than handwritten prescriptions [24].
On the other-hand 24.41% of the handwritten prescriptions had poor handwriting, while all computerized prescriptions were clear and legible. In the study by Irshaid et al., poor handwriting was recorded in large number of prescriptions (65.3%), while in study by Siddarth et al., and Phalke et al., illegible handwriting was seen in 6.3% and 17.6% respectively [11,15,20]. Poor handwriting is a serious problem and is a matter of concern for pharmacist esp. if he is unable to read the name of drugs prescribed.
The computerised prescriptions had some lacunae in a few areas like doctors signature was in 82% prescriptions, use of generic names only in 0.50% prescriptions, no mention of refill, and mention of dispense as written in only 16.50% of the prescriptions. On discussing with clinicians, they opined that the use of computer software for prescription writing was very tedious job. They felt that they needed separate skilled person for the same since they got dissociated from the patient while entering data themselves.
In present study, it is evident that out-patient prescription errors are abundant and often occult. Handwritten prescriptions were associated with relatively higher error rates associated with prescription writing in all areas like doctor’s details, patient details and drug details and even on other aspects like allergies, major illnesses and specific communication about drug. The computerized prescriptions on the contrary had lower frequency of prescription errors. Computer Physician order entry systems have advantages of clear legibility, accurate information on drugs, patient specific information such as warnings on overdoses, drug interactions and alerts on drug allergies, but they are expensive to introduce, measures must also be taken to encourage doctors to write prescriptions legibly.
Limitation
This study focused mainly on evaluation of prescriptions for omission errors i.e. errors in prescription writing rather than the commission errors i.e. errors in decision making which includes prescribing faults like irrational prescribing, overprescribing and under-prescribing. Also one cannot generalize the results of the study, as the data were collected solely from private practitioners of Anand city.
Conclusion
There seems to be an urgent need for education on appropriate prescription writing and furthermore re-inclusion of tutorials on prescription writing in final clinical year and internship of medical students. Administrative monitoring of prescription habits of clinicians is needed to improve health care process. By examining various aspects of prescription writing that can cause errors and by modifying prescribing habits, accordingly, clinician can improve the chance that the patient will receive correct prescription. Re-designing prescription forms, using computer generated prescriptions in day to day practice and sensitizing prescribers to improve prescription writing among clinicians will eventually help in reducing prescription errors.
*CVS/RS/L/K- Cardiovascular, Respiratory, Lung, Kidney condition of patient.