The aim of this study was to compare gonioscopy and various parameters available on SD-OCT in individuals with shallow anterior chamber and to determine the most reliable parameters.
Materials and Methods
This comparative observational study was done in a rural tertiary multi-speciality teaching hospital from April 2014 to September 2015 after getting approval from the institutional human ethics committee. Patients reporting to the outpatient department above the age of 40 with no history of intra-ocular surgery/ procedure, with healthy cornea and no anterior segment inflammation with peripheral Anterior Chamber Depth (ACD) of grade 2 or less by Van Herick’s technique were included in this study. For each study subject, slit lamp biomicroscopy, gonioscopy, SD-OCT imaging and a scan were performed on the same day.
1 drop of proparacaine (0.5%) eye drops was applied topically to both eyes prior to gonioscopy. Before placement, a drop of 1% hydroxymethyl cellulose was placed on the corneal curve of the lens. Gonioscopy was performed in the dark using Goldman 3 mirror lens at high magnification (X16). Examined eyes were in primary position of gaze. A narrow slit of 1mm, was cast during gonioscopy avoiding direct illumination over the pupil. The angle in each quadrant was graded with the shaffer grading system (grade 0: 0°, no structures seen, grade 1: ≤10°, schwalbe’s line visible, grade 2:10°–20°, posterior pigmented trabecular meshwork visible, grade 3:20°-35°, scleral spur visible, grade 4:35°-45°, visible ciliary body band) [4]. Manipulation of the angle was done in order to differentiate between appositional closure and peripheral anterior synechiae in quadrants where no angle structures were made out. But grading of all quadrants was done with eyes in primary position. The gonioscopic criteria for an occludable angle included angular width ≤ 2 by Shaffer grading.
Anterior segment imaging was performed with an anterior segment module lens, mounted over commercially available Spectral domain optical coherence tomography (Optos SLO OCT) imaging aperture.
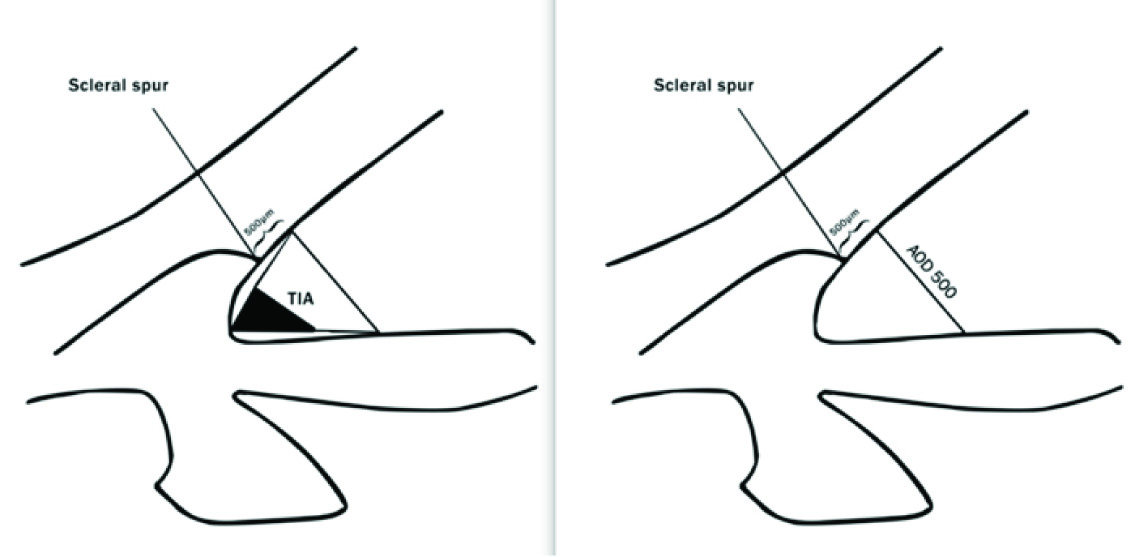
Imaging was performed in dark room conditions with the angle imaging software application. Images were taken by asking the patients to look straight ahead with the help of external fixation lights. Imaging of both meridional sections at 3 and 9 o’clock and at 1 and 7 o’clock was performed. The upper lid was elevated gently to avoid inadvertent pressure on the globe to image the superior angle. The image files were exported to a personal computer and were evaluated for the presence of a closed or open ACA by measuring the Trabecular Iris Angle (TIA) and Angle Opening Distance (AOD) [5] [Table/Fig-1]. Central ACD was measured by a scan biometry.
Measurement of Trabecular Iris Angle (TIA) and Angle Opening Distance (AOD).
*TIA 500 is defined as an angle measured with the apex in the iris recess and the arms of the angle passing through a point on the trabecular meshwork 500 μm from the scleral spur and the point on the iris perpendicularly.
*AOD 500 is defined as the distance from the corneal endothelium to the anterior iris surface perpendicular to a line drawn along the trabecular meshwork at 500 μm from the scleral spur.
Statistical Analysis
Statistical analysis used was Chi-square test, sensitivity, specificity, positive and negative predictive value in order to find correlation between OCT parameters and gonioscopy grading.
Results
A total of 101 eyes of 54 patients with peripheral shallow anterior chamber (50 right and 51 left eyes) were studied. Forty (72.7%) were females and 14 (27.3 %) were males. All patients were South Indians (Asians). The mean age was 53.9 ± 8.24 years (range, 40 - 75 years). The mean ACD was 2.47 mm ± 0.152 mm.
On gonioscopy, narrow angles (Shaffer grade ≤ 2) were identified in 95 (94%) superior, 42 (41.5%) inferior, 65 (64.3%) nasal and 57 (56.4%) temporal quadrants [Table/Fig-2]. Majority of the narrow (Shaffer grade ≤2) angles were found in superior quadrants. Open angles (Shaffer grade >2) were noted in 59 (58.4%) inferior quadrants.
Shaffer Grading of Angle Width in Different Quadrants of the Eye.
| Gonioscopic Grade | Superior Quadrant | Inferior Quadrant | Nasal Quadrant | Temporal Quadrant |
|---|
| 0 | 63 | 9 | 23 | 25 |
| 1 | 24 | 7 | 13 | 9 |
| 2 | 8 | 26 | 29 | 23 |
| 3 | 4 | 19 | 9 | 22 |
| 4 | 2 | 40 | 27 | 22 |
* Shaffer grade ≤ 2 were identified in 95 (94%) superior, 42 (41.5%) inferior, 65 (64.3%) nasal and 57 (56.4%) temporal quadrants, respectively.
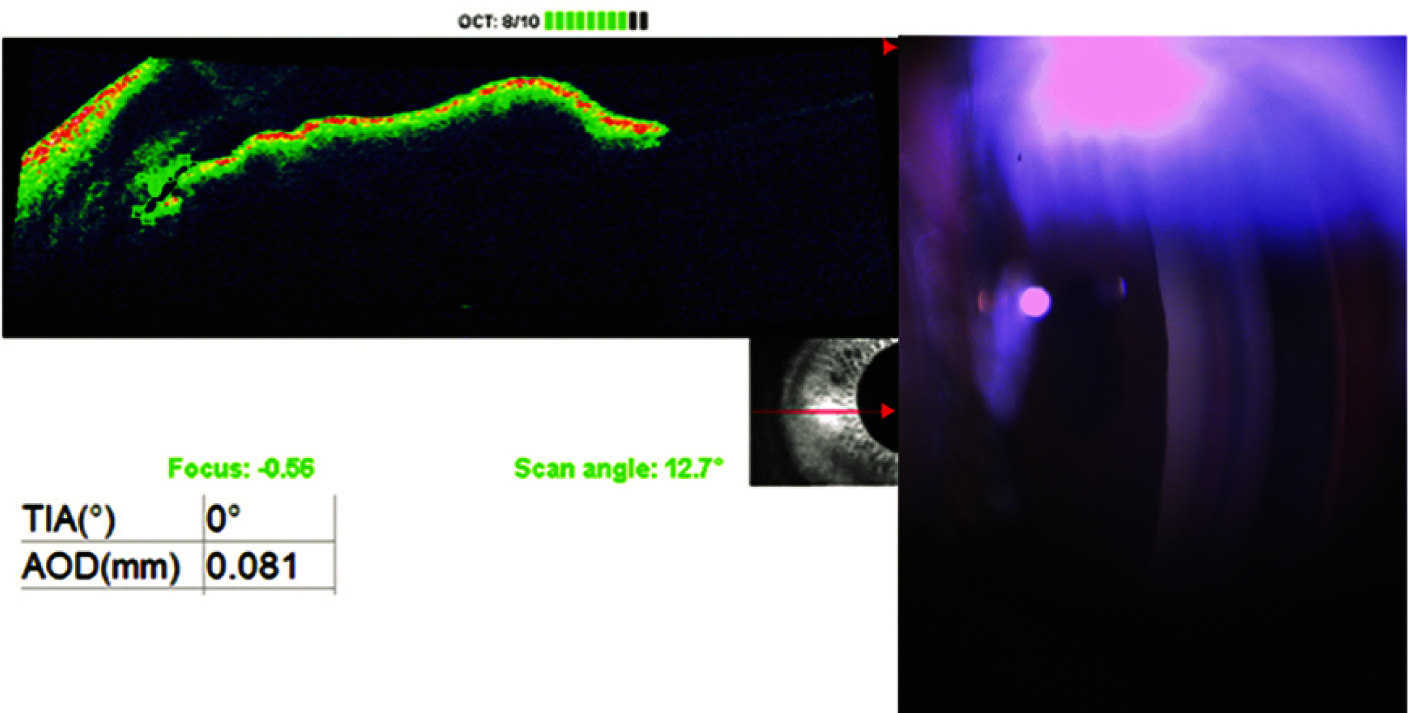
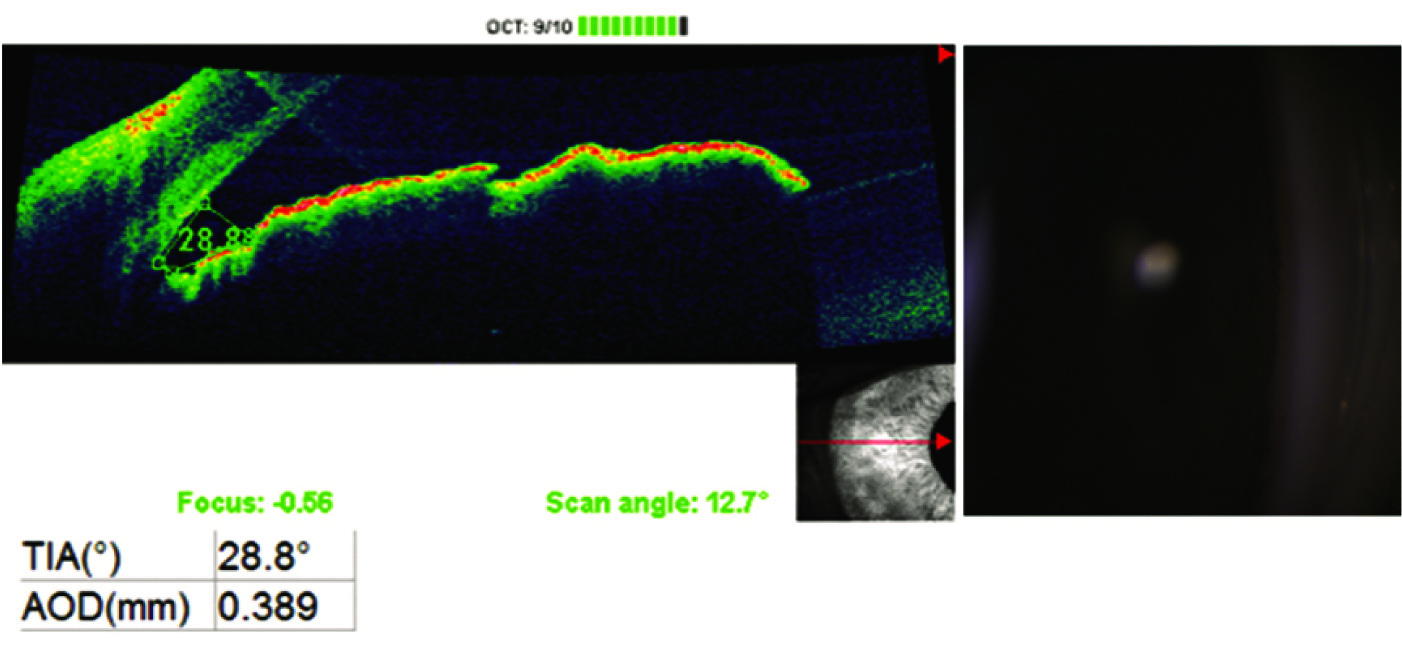
Anterior segment imaging of all the 4 quadrants were obtained [Table/Fig-3,4]. Scleral spur (landmark required for calculation of TIA and AOD) was not clear in the superior and inferior OCT images. Therefore, the nasal and temporal gonioscopy grading have been compared with values from corresponding OCT images. Scleral spur was not identifiable in 6 nasal and 1 temporal OCT images and they were excluded from analysis.
OCT and gonioscopy image showing a closed angle.
* OCT image showing TIA of 0° and AOD of 81 μm of the same angle with shaffer grade 0.
OCT and Gonioscopy Image Showing an Open Angle.
* OCT image showing TIA of 28.8° and AOD of 389 μm of the same angle with shaffer grade 4.
Since, cut-off values for Indian eyes were not available, we have analysed our data based on the study conducted by Wirbelauer C et al., where the cut off values in detecting narrow angles were anterior chamber angle of ≤ 22° and AOD of ≤ 290 μm [6]. OCT detected angles ≤ 22° in 88 (92.6%) nasal and 87 (87%) temporal quadrants, whereas >22° was noted in 7 (7.3%) nasal and 13 (13%) temporal quadrants. AOD of ≤ 290 μm was found in 73 (76.8%) nasal and 83 (83%) temporal quadrants.
High sensitivity and low specificity of TIA and AOD on OCT was found compared to the gold standard in detecting narrow angles [Table/Fig-5,6]. Best agreement was observed between TIA and gonioscopy in nasal quadrants [Table/Fig-7].
Sensitivity and specificity of gonioscopy grading with TIA.
| ≤2 | >2 | TOTAL |
|---|
| ≤ 22° | 107(61.1%) | 68(38.9%) | 175(100.0%) |
| >22° | 11(55.0%) | 9(45.0%) | 20(100.0%) |
| TOTAL | 118(60.5%) | 77(39.5%) | 195(100.0%) |
Sensitivity: 90.7%, specificity: 11.7%, positive predictive value: 61%, negative predictive value: 45%, chi-sqaure : 0.283, df : 1, p: 0.381
High sensitivity and low specificity of TIA in detecting narrow angles.
Chi-square test found no association between TIA and Gonioscopy grade.
Sensitivity and specificity of gonioscopy grading with AOD
| ≤2 | >2 | TOTAL |
|---|
| ≤ 290 μm | 97(62.2%) | 59(37.8%) | 156(100.0%) |
| >290 μm | 21(53.8%) | 18(46.2%) | 39(100.0%) |
| TOTAL | 118(60.5%) | 77(39.5%) | 195(100.0%) |
sensitivity: 82.2%, specificity: 23.4%, positive predictive value: 62.2%, negative predictive value: 46.2%, chi-sqaure: 0.907, df: 1, p: 0.341
High sensitivity and low specificity of TIA in detecting narrow angles.
Chi-square test found no association between TIA and Gonioscopy grade.
Agreement between gonioscopy and OCT parameters of nasal and temporal angles in detecting narrow angles.
| Agreement | No Agreement | Total |
|---|
| ≤2 and ≤ 22° nasal | 59 (96.7%) | 2 (3.3%) | 61 (100%) |
| ≤2 and≤ 22° temporal | 48 (84.2%) | 9 (15.8%) | 57 (100%) |
| ≤2 and ≤ 290 μm nasal | 50 (82%) | 11 (18%) | 61 (100%) |
| ≤2 and ≤ 290 μm temporal | 47 (82.5%) | 10 (17.5%) | 57 (100%) |
* Narrow angles with gonioscopy ≤2 and TIA ≤ 22° was found more in nasal quadrants.
Discussion
Angle assessment is essential for determining type of glaucoma based on angles. Although gonioscopy has been considered as the gold standard for characterizing the ACA, it is subjective and requires the expertise. Placement of a contact lens on the eye and localized corneal compression can cause fluid displacement and widening of the angle. Light intensity can alter grading of the angle. Imaging with OCT defines ACA characteristics in an objective manner avoiding contact with the globe with contact lens. These images can be analysed qualitatively and quantitatively. As a result, it is a quick, easily tolerated procedure for the patient and there is also less distortion of angle morphology due to lack of globe manipulation [3].
This study also showed that with gonioscopy, angle width is narrowest in the superior quadrant similar to other studies [9,10].
Narrow angles were detected more in older population and in women compared to men in our study, consistent with other reports in multiple populations [11,12]. The most likely explanations for a higher prevalence of PACG among older persons are the increase in lens thickness that occurs with age. This leads to crowding of the anterior segment. In addition, it is postulated that the zonules becomes more lax with age, allowing the anterior movement of the lens-iris diaphragm.
OCT was able to detect more narrow angles compared to gonioscopy (nasal 92.6% and 64.3% and temporal 87% and 56.4%, respectively). Similar findings were noted in other studies [10,13]. This can be due to differences in lighting conditions. Complete darkness was possible for OCT examination because no visible light is required to obtain the image. Despite efforts to use as little light as possible, the anterior segment and pupil are exposed to light during gonioscopy. This may open up an angle that could have been closed in the dark. Also, angle opening could have been possible by displacement of anterior segment structures when Goldman lens was placed on the globe [13].
Various studies [Table/Fig-8] have defined occludable angles on OCT. But there is no consensus as of which of the parameters best describes the anterior chamber angle.
Parameters of Different Studies Defining Occludable Angles.
| Author Name | TIA (°) | AOD 500 (μm) | TISA (mm2) | ACA(°) | ARA 500(mm2) |
|---|
| Cheung CY et al., [5] | 14.5 | 178 | 0.060 | - | - |
| Wirbelauer C et al., [6] | - | 290 | - | 22 | - |
| Grewal DS et al., [7] | - | 330 | 0.230 | - | - |
| Radhakrishnan S et al., [8] | - | 191 | 0.11 | - | 0.120 |
* Studies indicating the cutoff values of different parameters (trabecular iris angle TIA, angle opening distance AOD, trabecular iris surface area TISA, Anterior Chamber Angle ACA, angle recess area ARA) Defining Occludable Angles on OCT.
Limitation
Small sample size remains the limitation of our study. With more number of patients, a normative value and cut off values for occludable angle can be found out. Also, the scleral spur of superior and inferior quadrants could not be identified in the model of the OCT used in the study.
Conclusion
SD-OCT is more sensitive than gonioscopy in identifying narrow angles. It has low specificity though. Similar study on a larger population shall provide definitive answer. Objective measurement by a non-contact technique remains the major merit of SD-OCT.
* Shaffer grade ≤ 2 were identified in 95 (94%) superior, 42 (41.5%) inferior, 65 (64.3%) nasal and 57 (56.4%) temporal quadrants, respectively.
Sensitivity: 90.7%, specificity: 11.7%, positive predictive value: 61%, negative predictive value: 45%, chi-sqaure : 0.283, df : 1, p: 0.381
High sensitivity and low specificity of TIA in detecting narrow angles.
Chi-square test found no association between TIA and Gonioscopy grade.
sensitivity: 82.2%, specificity: 23.4%, positive predictive value: 62.2%, negative predictive value: 46.2%, chi-sqaure: 0.907, df: 1, p: 0.341
High sensitivity and low specificity of TIA in detecting narrow angles.
Chi-square test found no association between TIA and Gonioscopy grade.
* Narrow angles with gonioscopy ≤2 and TIA ≤ 22° was found more in nasal quadrants.
* Studies indicating the cutoff values of different parameters (trabecular iris angle TIA, angle opening distance AOD, trabecular iris surface area TISA, Anterior Chamber Angle ACA, angle recess area ARA) Defining Occludable Angles on OCT.