Massive Intrabile Duct Invasion Caused by a Fatal Progression of Colonic Adenocarcinoma: Abdominal Computed Tomography Findings and Cholangiography Correlation
Jesus Rodriguez-Pascual1, Michael Tyler B Abbitt2, Marisol Fernádez3, Fernando Camuñez4, Francisco José Pérez-Rodríguez5
1 Attendig Oncologist, Clinical Oncology Department, Hospital Universitario Montepríncipe, Boadilla Del Monte, Madrid, Spain.
2 Resident, Department of Radiology, University of Illinois at Chicago Hospital, Chicago, Illinois, USA.
3 Attending Radiologist, Department of Radiology, Hospital Universitario Montepríncipe, Boadilla Del Monte, Madrid, Spain.
4 Attending Gastroenterologist, Department of Gastrointestinal, Hospital Universitario Montepríncipe, Boadilla Del Monte, Madrid, Spain.
5 Department of Pathology, Hospital Universitario Montepríncipe, Boadilla Del Monte, Madrid, Spain.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jesus Rodriguez Pascual, Hospital Universitario Madrid Montepríncipe, Avda Montepríncipe 25, 28660, Boadilla Del Monte, Madrid, Spain.
E-mail: jrodriguez@hmhospitales.com
In this report, we present an unusual case of jaundice in a patient with advanced colorectal cancer due to intraductal tumour invasion of the intra- and extrahepatic biliary tree. This complication proved to be fatal despite aggressive therapeutic management. A correct diagnosis of this type of involvement was achieved by a combination of diagnostic and therapeutic cholangiography. Despite adequate biliary decompression, the patient died from liver failure and biliary sepsis.
Contrast enhanced computed tomography, Colorectal cancer, Intrabiliary metastases
Case Report
A 62-year-old Caucasian male was referred to Medical Oncology Department with an 18 month history of colon cancer complicated by liver and lung metastasis at diagnosis, being treated in active second-line chemotherapy with FOLFIRI plus Bevacizumab. Ten days after his last chemotherapy administration, the patient complained of insidious and progressive abdominal pain localized in the right upper abdominal quadrant. He also noted dark urine and chalky stools. The patient had no chills or fever. He presented with mucocutaneous jaundice, consistent with elevated serum bilirubin levels (direct bilirubin 4.5 g/dL). Other laboratory tests were normal, including WBC.
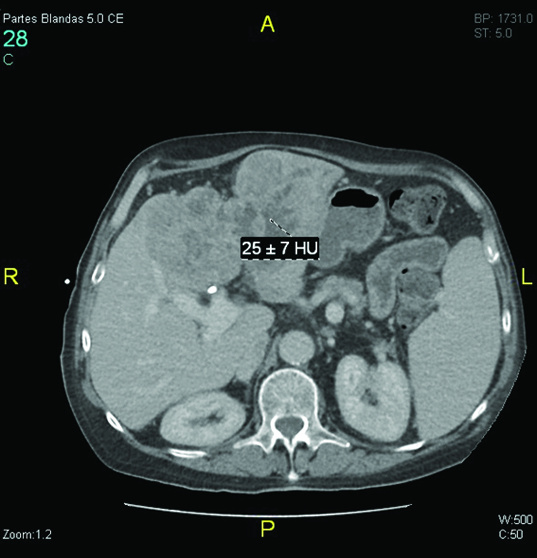
Abdominal CT scan demonstrated multiple hypodense hepatic lesions compatible with the diagnosis of liver metastasis but without increase in size or number when compared to the prior CT scan. However, we identified interval multifocal dilatation of intra- and extrahepatic bile ducts. At this time the differential diagnosis was established to include extrinsic obstruction due to hepatic tumour progression, solid endoluminal occupation by infection or biliary microlithiasis or haemobilia secondary to Bevacizumab.
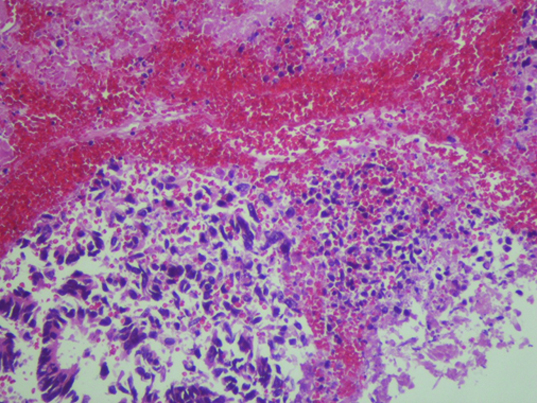
Percutaneous transhepatic cholangiography was then performed after ciprofloxacin prophylaxis. Internal-external drainage was placed during the intervention. During the procedure, solid material occupying the bile duct was unexpectedly identified [Table/Fig-1]. Pathological analysis demonstrated the presence of solid tumour fragments of adenocarcinoma [Table/Fig-2]. At this time, microbiological study of biliary fluid did not detect bacterial cholangitis. Given these findings, abdominal CT images were reviewed which revealed increased iodinated contrast uptake within the dilated bile duct, suggestive of bile duct tumour invasion [Table/Fig-3].
Cholangiography. Dilated biliary tract. Distal duct was not opacified due to solid material occupying the bile duct.

Histologic findings of the isolated biliary drainage solid fragments (HE stain). The histologic features were indicative of an adenocarcinoma. The liver and intrabile duct tumours resembled the colon carcinoma.
Abdominal computed tomography (CT). A contrast enhanced CT scan demonstrated dilatation of the intra- and extrahepatic bile duct and increased uptake of iodinated contrast within the dilated bile duct, suggestive of bile duct tumour invasion.
Despite an adequate biliary drainage, serum bilirubin levels were gradually increased. This was likely refractory to transhepatic drainage due to a mechanical limitation caused by the tumoural mold. Repeat cholangiography and new left biliary duct drain placement were achieved, but this measure failed to stabilize the situation. The patient subsequently developed a severe secondary biliary infection which evolved into septic shock. Despite antibiotic treatment, the patient died on the twentieth day of hospitalization.
Discussion
It is well known that intrabiliary invasion and growth is one of the developmental patterns of primary liver tumours. In Hepatocellular Carcinoma (HCC) this invasion potential is thought to be an indicator of a poor prognosis [1]. With respect to Intrahepatic Cholangiocarcinoma (ICC), bile duct invasion is a common characteristic [2]. Bile duct invasion by metastatic colorectal cancer has been previously reported in rare cases mimicking an intraductal papillary neoplasm of the extrahepatic bile duct [3], presenting intrapancreatic duct metastastases [4] or specifically in pathological examination after surgical treatment of isolated liver metastasis [5–7,11]. In a study by Kubo et al., microscopic bile duct invasion was found in 89 of 217 cases (41%), and 23 of 217 cases of macroscopic intrabiliary extension (10.5%) [8]. Curiously, in their study, macroscopic intrabiliary extension seems to define a unique subgroup of colorectal cancers showing less aggressive features (well-differentiated adenocarcinoma, decreased primary tumour size, and less frequent venous invasion). Takamatsu et al., described a case report of a surgically resected liver metastasis with prominent intrabiliary growth derived from rectal cancer [9]. A partial hepatectomy, partial resection of segment VI, and an extrahepatic bile duct resection with reconstruction of the biliary tract were performed. Ghittoni et al., described a case of a metastasis from colorectal cancer involving the common hepatic biliary duct without invasion of contiguous liver parenchyma [10]. A contrast enhanced ultrasound and ultrasound-guided fine needle aspiration biopsy was used for a confirmed diagnosis. As in the previous cases, liver surgery and bile duct reconstruction could solve the clinical problem. Finally, Estrella et al., reported a recent study that estimated the prevalence of intrabiliary growth in liver metastases by both prospective and retrospective analyses [3]. By retrospective review of 1144 surgical pathology reports, they found intrabiliary growth in 3.6% of metastatic CRCs. Prospective evaluation of 170 liver resections yielded a 3-fold increase in prevalence (10.5%), again evenly divided between major (5.3%) and minor (5.3%) duct involvement. These findings suggest that intrabiliary growth is easily overlooked, even when it involves large or multiple bile ducts.
To our knowledge this patient is the first case of fatal diffuse biliary involvement due to colon cancer progression. Secondary to pre-existing bilobar liver metastasis, lung metastasis and failure with second line chemotherapy, there was no clear hepatic surgical indication. Thus, percutaneous transhepatic drainage seemed to be a reasonable palliative option. Unfortunately, drainage proved to be ineffective in this case. Solid tumour occupation of the entire bile duct prevented improvement in jaundice despite a second drainage. Biliary sepsis was the final event of a terminal situation.
Peungjesada et al., presented the spectrum of CT findings of biliary involvement of metastatic colorectal liver metastasis [12]. Various patterns of radiologic presentation were described in this article. In some cases, biliary invasion was detected only by recognizing the cross-section of a dilated duct usually seen along the corresponding opacified portal venule. However, abdominal CT finding of iodinated contrast enhancement of the dilated bile duct in our study seemed to be an interesting and useful radiological feature. This finding should be confirmed in other cases, and may clarify the discrepancy between the frequency of macroscopic bile duct invasion in liver metastasis of colon cancer in previous cited studies (around 10%) and the absence of clinical data in routine clinical practice. Notably, unlike abdominal ultrasound or magnetic resonance imaging, CT scan is a part of the routine monitoring of patients with advanced colon cancer.
Conclusion
Diffuse biliary involvement due to colon cáncer metástasis is a rare and fatal clinical entity with specific abdominal CT findings. Percutaneous transhepatic drainage is an ineffective option in this setting.
[1]. Kojiro M, Kawabata K, Kawano Y, Hepatocellular carcinoma presenting as intrabile duct tumour growth: a clinicopathologic study of 24 casesCancer 1982 49:2144-47. [Google Scholar]
[2]. Suh KS, Roh HR, Koh YT, Clinicopathologic features of the intraductal growth type of peripheral cholangiocarcinomaHepatology 2000 31:12-7. [Google Scholar]
[3]. Estrella JS, Othman ML, Taggart MW, Intrabiliary growth of liver metastases:clinicopathologic features, prevalence, and outcomeAm J Surg Pathol 2013 37(10):1571-79. [Google Scholar]
[4]. Yamao T, Hayashi H, Higashi T, Colon cancer metastasis mimicking intraductal papillary neoplasm of the extra-hepatic bile ductInt J Surg Case Rep 2015 10:91-93. [Google Scholar]
[5]. Yamamoto J, Sugihara K, Kosuge T, Pathologic support for limited hepatectomy in the treatment of liver metastases from colorectal cancerAnn Surg 1995 221:74-78. [Google Scholar]
[6]. Riopel MA, Klimstra DS, Godellas CV, Intrabiliary growth of metastatic colonic adenocarcinoma: a pattern of intrahepatic spread easily confused with primary neoplasia of the biliary tractAm J Surg Pathol 1997 21:1030-36. [Google Scholar]
[7]. Okano K, Yamamoto J, Moriya Y, Macroscopic intrabiliary growth of liver metastases from colorectal cancerSurgery 1999 126:829-34. [Google Scholar]
[8]. Kubo M, Sakamoto M, Fukushima N, Less aggressive features of colorectal cancer with liver metastases showing macroscopic intrabiliary extensionPathol Int 2002 52:514-18. [Google Scholar]
[9]. Takamatsu S, Teramoto K, Kawamura T, Liver metastasis from rectal cancer with prominent intrabile duct growthPathol Int 2004 54:440-45. [Google Scholar]
[10]. Ghittoni G, Caturelli E, Viera FT, Intrabile duct metastasis from colonic adenocarcinoma without liver parenchyma involvement: contrast enhanced ultrasonography detectionAbdom Imaging 2010 35:346-48. [Google Scholar]
[11]. Kawakatsu S, Kaneoka Y, Maeda A, Intrapancreatic bile duct metastasis from colon cancer after resection of liver metastasis with intrabiliary growth: a case reportWorld J Surg Oncol 2015 13:254 [Google Scholar]
[12]. Peungjesada S, Aloia TA, Kaur H, Intrabiliary growth of colorectal liver metastasis: spectrum of imaging findings and implications for surgical managementAJR Am J Roentgenol 2013 201(4):W582-89. [Google Scholar]