Introduction
Hepatic injury of varied aetiology may progress to Acute Liver Failure (ALF). Compromised microcirculation is thought to be a deciding factor of hepatic hypoxia may be involved in disease progression that needs early detection. Ischaemia markers like serum Ischaemia- modified albumin (IMA), ALT-LDH ratio and ALT-LDH index have been suggested for its detection at early stage.
Aim
To find out the association of Ischaemia markers like serum IMA, ALT-LDH ratio and ALT-LDH index in acute hepatic injury cases.
Materials and Methods
Forty one diagnosed acute liver injury cases of varied aetiology admitted in Department of Medicine, and Gastroenterology of SCB Medical College, Cuttack were enrolled in the study along with 30 age and sex matched healthy controls. Blood collected at time of admission and at time of discharge (1st day and 7th day) were evaluated for FPG, RFT, LFT, Serum Albumin along with serum LDH, IMA, PT-INR and platelet count.
Result
Serum bilirubin, hepatic enzymes, IMA, PT-INR was more markedly raised in cases than controls on the 1st day of admission. ALT-LDH ratio and index were significantly low in complicated cases. However, on responding to treatment the ALT-LDH index on 7th day registered a rise in comparison to the 1st day, while serum IMA revealed an insignificant decline showing improvement in hepatic hypoxia. ALT-LDH ratio remains more or less same on response to treatment.
Conclusion
Serum IMA and ALT-LDH Index reveals association with disease process in Acute Hepatic Injury cases both clinically and biochemically and can be used as supportive parameters for the diagnosis of disease process.
Acute liver failure, IMA, ALT-LDH Index
Introduction
Injury to hepatocytes and liver is a common problem worldwide. Though, the incidence of infective hepatitis has been decreased after introduction of available vaccines in developed countries, yet it is still a major contributor to acute hepatic injury in developing countries like India [1]. Besides this, the other prevailing contributors to liver damage in acute hepatic injury include alcoholic hepatitis, drug induced hepatitis, ischaemic hepatitis, toxic hepatitis, obstructive hepatitis and hepatitis of unidentifiable causes [2,3].
Acute hepatic injury begins with an acute or insidious onset being detected by the presence of jaundice or non-specific symptoms of acute illness like fatigue, nausea, vomiting, fever, abdominal discomfort etc., with increase in the activities of enzymes like aspartate aminotransferase (AST) and/or alanine aminotransferase (ALT). The disease can be diagnosed by the rise in ALT ≥ 10 and ALP ≤ 3 times the upper reference limits. However, severity of the disease is best assessed by prothrombin time and total bilirubin. In majority of cases though they recover completely, yet very few cases may become chronic, and some may have a rare fate of severe liver damage that results in a fatal state of Acute Liver Failure (ALF) [4,5].
Though a rare event, ALF is characterised by abrupt onset and rapid progression with high mortality being on complicated with altered mental status, hepatic encephalopathy and coagulopathies [6,7]. Initially, this is indistinguishable from acute hepatic injury. Once encephalopathy develops in severe cases with altered mental state and coagulopathy, management with conservative treatment becomes ineffective. Therefore, it is necessary to detect the disease at an early stage of acute hepatic injury and to prevent further progression of the disease. Model for End Stage Liver Disease (MELD) criteria has been applied widely [4,8], that holds good in chronic liver diseases, but may not be appropriate for acute hepatitis.
The characteristic pathologic finding of ALF is massive necrosis without regeneration. The underlying mechanism being hepatic hypoxia due to acute hepatic injury. The hepatic hypoxia due to sudden impedence in microcirculation by the over activation of macrophages in liver has been suggested to play key role in this condition [9]. The macrophage proliferation in liver can be assessed by liver biopsy, the only reliable means that carries the risk of bleeding in an already unwell patient. Lactate Dehydrogenase (LDH) is another enzyme seen to elevate in this condition. It can be taken into account as an ischemic marker of hepatic damage but has multiple sources of origin. This raised LDH has a shorter half life than ALT, resulting in earlier fall in serum level [10–12]. Taking into consideration the rise in serum LDH, its short half life and early fall in serum level than ALT, ALT-LDH ratio and ALT-LDH index have been hypothesized as markers of hepatic hypoxia, to detect the deteriorating patients at an early stage of acute hepatic injury, before progressing to ALF [13–15].
Plasma Ischaemia Modified Albumin (IMA), a rule out test of cardiac ischaemia, has gained importance in myocardial infarction as well as in other regional Ischaemia [15,16]. Studies have highlighted that a significantly high IMA/Albumin Ratio, IMAR (ischaemia modified albumin with respect to total serum albumin) has been observed in ACLF (Acute on Chronic Liver Failure), showing altered albumin function in cirrhosis of liver along with raised value of markers of oxidative stress, being co-rrelated with degree of hepatic impairment [17,18]. IMAR levels were shown to be significantly higher in non survivors in comparison to survivors. Significant rise in IMA has also been seen in chronic liver disease cases along with severity of disease [19–21].
Aim
To find out the role of serum IMA, ALT-LDH ratio and ALT LDH index in detecting the degree of hepatic hypoxia in acute liver injury and their association with the disease process.
Materials and Methods
A pilot study was conducted with 41 acute hepatic injury patients of various aetiology admitted to the indoor Department of Medicine and Hepatology of SCB Medical College and Hospital, Cuttack along with 30 age and sex matched healthy controls. The study was carried out in the Department of Biochemistry, SCB Medical College, Cuttack, from December 2012 to December 2014 after institutional ethical clearance. Patients were diagnosed on the basis of ALT ≥ 10 times the upper reference limits and ALP≤ 3 times the upper reference limits, after a detailed history of alcohol intake, drug intake, and blood culture and testing of viral markers. Cases were divided into complicated (n=12) and uncomplicated (n=29) depending on the signs and symptoms of encephalopathy and coagulopathy along with PT-INR (>1.5), bilirubin and ultrasonographic findings. Hepatic involvement due to malignancy, non alcoholic fatty liver disease, previous chronic liver disease and patients having onset of any clinical symptoms such as general fatigue, appetite loss, nausea and jaundice, which began ten days before admission were also excluded from the study.
Both groups of cases and 30 age and sex matched healthy controls were exposed to analysis of routine biochemical investigations that included fasting plasma glucose (FPG), serum urea, creatinine, liver function test, prothrombin time (PT-INR) and serum IMA on the day of admission (first day) as well as on the day of discharge. Routine biochemical parameters were carried out using Flexor- XL autoanalyser. Serum IMA assay was performed by Cobalt binding Assay [15].
Statistical Analysis
The results obtained were analysed using one tailed chi-square test, paired T-test, and Pearson correlation using SPSS- 21 version soft ware.
Results
[Table/Fig-1] documents the biochemical parameters of the study group on the day of admission showing marked rise in total bilirubin, transaminases, alkaline phosphatase, LDH along with PT-INR in acute hepatic injury cases in comparison to control reflecting hepatic damage. A comparative analysis of biochemical parameters between complicated (n=12) and uncomplicated cases (n=29) registered a significant increase in PT-INR, total bilirubin, IMA and MELD score. ALT-LDH index, ALT-LDH ratio registered a significant fall in complicated cases of acute hepatic injury than the uncomplicated group [Table/Fig-2]. On 7th day of treatment 30 patients were discharged and 4 patients had to stay back in the hospital with subsided disease process responding to conservative treatment. However, 7 patients deteriorated in spite of conservative treatment.
Routine biochemical parameters (mean+SD) in controls and cases on day of admission.
| Parameters | Controls (n = 30) | Cases (n =41) |
|---|
| Fasting plasma glucose (mg/dl) | 81.1 ± 9.8 | 89.9 ± 9.3* |
| Serum Urea (mg/dl) | 25.3 ± 6.3 | 45.5 ± 11.7* |
| Serum Creatinine (mg/dl) | 0.86 ± 0.2 | 1.31± 0.56* |
| T. Bilirub in (mg/dl) | 0.9 ± 0.16 | 1.7± 0.50* |
| Serum AST (IU/L) | 24.3 ± 5.5 | 618 ± 96.5* |
| Serum ALT(IU/L) | 19.5 ± 2.5 | 547.5 ± 115.7* |
| Serum Alkaline Phosphatase (IU/L) | 82.6 ± 13.6 | 239.5± 62.4* |
| LDH (IU/L) | 190.9 ± 23.1 | 446.7± 65.8* |
| PT-INR | 0.85 ± 0.21 | 1.44 ± 0.5* |
| IMA (U/ml) | 64.4 ± 7.5 | 93.6 ±10.5* |
*p < 0.001
Special biochemical investigations (mean±SD) in complicated and uncomplicated cases on day of admission.
| Parameters | Uncomplicated(n = 29) | Complicated(n= 12) |
|---|
| LDH (U/L) | 413.7± 46.9 | 523.8± 26.8** |
| PT-INR | 1.27± 0.4 | 1.84 ±0.48** |
| IMA (U/ml) | 90.9 ± 9.0 | 100.0±11.3* |
| ALT – LDH ratio | 1.27± 0.30 | 1.09 ± 0.18* |
| ALT – LDH index | 2.49 ± 0.72 | 1.74 ± 0.30** |
| MELD Score | 11.9 ± 3.63 | 21.9± 4.8** |
*p < 0.05, ** p<0.001
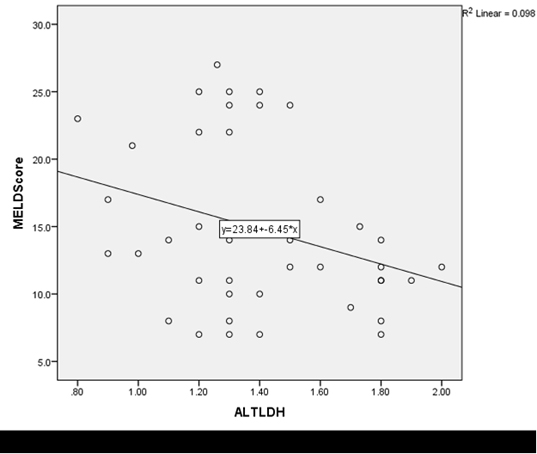
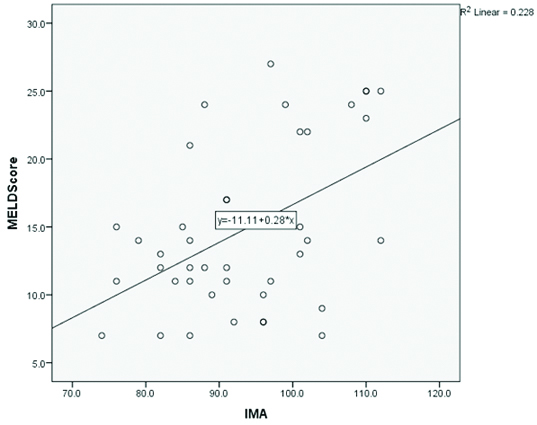
On 7th day of treatment, these 34 patients from both complicated and uncomplicated groups showed signs of improvement both clinically and biochemically. Comparison of hypoxic parameters on 7th day i.e., IMA, ALT- LDH ratio and ALT- LDH index in the 34 responders to treatment, with values on day of admission revealed insignificant fall in IMA with significant rise in ALT-LDH index [Table/Fig-3]. Thus, there was a transition in these hypoxic parameters in responders of conservative treatments. However, in the non-responders to conservative treatments who were 7 in number, these ischemic parameters remained more or less same, without marked change, along with increase in transaminases and LDH on 7th day requiring their prolonged stay in the hospital. Pearson correlation of IMA and ALT-LDH index with MELD score [Table/Fig-4,5] on first day in the cases revealed the association of hepatic hypoxia with the disease process.
Comparison of special parameters (mean ± SD) of responders (n = 34) on 1st and 7th day of treatment.
| Parameters | Responders (n=34)(1st Day) | Responders (n=34)(7th Day) |
|---|
| ALT (IU/L) | 523.4±100.9 | 449.6 ± 89.9* |
| LDH (IU/L) | 439.1±65.4 | 376.4± 64.2* |
| IMA (U/mL) | 91.6 ±9.9 | 83.6±9.0 |
| ALT –LDH ratio | 1.21±0.26 | 1.22±0.25 |
| ALT – LDH Index | 2.29±0.7 | 2.74 ±0.85* |
*p< 0.001
Correlation of MELD score with ALT LDH index (p < 0.002) in patients of acute liver injury Correlation (-0.314).
Correlation of MELD score with IMA (r=0.478, p< 0.001) in patients of acute liver injury.
Discussion
Injury to hepatocyte from various aetiology is common worldwide, though vaccination has reduced the incidence rate of virus aetiology [1,2]. Rise in serum transaminases >10 times upper reference limit with <3 times rise of alkaline phosphatase are the diagnostic features of this, which is mostly a self limiting process [1,3,4]. Rarely, it gets complicated with coagulopathy and/or mental disorders ending with acute hepatic failure [5–10]. Hepatic hypoxia resulting from blockage of microcirculation due to macrophage proliferation may be the underlying mechanism for progression to ALF [9,10]. Raised value of LDH of anaerobic aetiology along with transaminases have been observed in hypoxic liver injury cases [11,12]. However, it has a short half life than transaminases, for which ALT-LDH index, ALT- LDH ratio have been taken into consideration [13,14]. IMA has come out as an hypoxic marker in acute coronary syndrome as well as other ischemic conditions [15,16]. Alteration of activity and metal binding ability of albumin due to chronic liver disease and oxidative stress has been demonstrated in various studies [17,18]. Marked dysfunction of albumin due to damage to circulating albumin was demonstrated in advanced cirrhosis cases by Jalan et al., showing, a correlation of IMA-to-serum albumin ratio (IMAR) with disease severity, suggesting its prognostic value in acute-on-chronic liver failure [18]. However, raised IMA and IMA-to-serum albumin ratio IMAR have been observed in chronic hepatitis and chronic liver disease cases by Zuwala-Jagietto et al., Chen et al., and Cakir et al., in association with inflammatory markers and oxidative stress [19–21]. Observation of Chen et al., regarding IMA and IMA-to-serum albumin ratio (IMAR) reflecting liver function and oxidative stress revealed raised values in chronic hepatitis on cirrhosis patients, in comparison to healthy volunteers which remained unaltered after a 3 day albumin infusion [20]. IMA and IMAR were significantly higher in children with chronic liver disease than control and IMAR was positively correlated with paediatric end stage liver disease score in study population of Cakir et al., [21].
In the present study, prominent elevation of serum IMA was observed, being more marked in complicated cases revealing a state of raised hepatic hypoxia and oxidative stress. The other hypoxic marker ALT-LDH index, ALT- LDH ratio registered a low value in complicated cases in comparison to uncomplicated cases suggesting advanced state of Ischaemia in complicated cases with a raised LDH value. A similar observation is also noticed by Kotoh et al., in his group of acute hepatic injury cases [14]. However, with a positive response to conservative treatment, a change in both these hypoxic markers along with IMA was noted on day of discharge or 7th day of treatment. The insignificant fall in IMA, along with a significant increase in ALT- LDH index indicates an improvement in hypoxic state of liver due to early fall in LDH level than ALT similar to Kotoh et al., on 5th day of treatment [14]. Several studies [13,14,20] have highlighted that ALT-LDH index could reflect the rapid clinical change of ALF. Those not responding to conservative treatment i.e., the deteriorating patients registered a near same value of both hypoxic parameters on 1st and 7th day of treatment with indication to stay in the hospital, with an unchanged or near to equal LDH value, reflecting a delayed return of serum LDH to normal due to sustenance of hypoxic state, which may lead to acute liver failure with poor prognosis. The association of both markers IMA, ALT- LDH index with MELD score revealed the association of hypoxia with the disease process of acute hepatic injury.
As reported by several authors overactivation of macrophages plays a key role in the progression of ALF [9]. The activated and proliferated macrophages in the liver could injure the endothelial cells and cause a disturbance in hepatic microcirculation. LDH, an enzyme of anaerobic glycolysis, causing conversion of pyruvate to lactate is over expressed in hypoxic conditions [11–14].
Although, raised LDH activity in acute liver injury is supposed to be due to increased LDH production by hepatic anaerobic condition and to enzyme leakage through damaged hepatocyte membrane like ALT, accordingly the persistence of ALT-LDH index in non responders might be the result of increased production of LDH from residual living hepatocytes due to continued hypoxia. This massive hepatic hypoxia for long duration may lead to lobular necrosis that may result in pathologic changes of ALF. Direct cytotoxicity towards hepatocytes by cytotoxic T cells by various triggers and hypoxic liver injury caused by disturbance of hepatic microcirculation by proliferated macrophages as suggested above are supposed to be involved in acute liver injury [14].
Limitation
However, limitations in this study were small patient group, and the heterogeneous, primary aetiology for the acute hepatic Injury cases.
Conclusion
IMA and ALT-LDH index, associated with disease process as markers of hypoxia can be taken as supportive parameters to the previously existing MELD score to detect the conservative survivors at an early stage, before deteriorating to ALF. ALT-LDH index however reflects a better hypoxic marker than ALT/LDH ratio in the prognosis of the disease process.
Their prognostic association with the disease process can be better assessed, when the study will be prospectively conducted in a large population.
*p < 0.001
*p < 0.05, ** p<0.001
*p< 0.001
[1]. Dufour DR, Lott JA, Nolte FS, Gretch DR, Koff RS, Seeff LB, Diagnosis and Monitoring of hepatic injury II. Recommendations for use of laboratory tests in Screening, Diagnosis and MonitoringClin Chem 2000 46(12):2050-68. [Google Scholar]
[2]. Devarbhavi H, Anti tuberculous drug induced liver injury: Current perspectiveTrop Gastroenterol 2011 32(3):167-74. [Google Scholar]
[3]. Devarbhavi H, An Update on drug –induced liver injuryJournal of Clinical and Experimental Hepatology 2012 2(3):247-59. [Google Scholar]
[4]. Lee WM, Strauvitz RT, Larsuy AM, Introduction to the revised American Association for the study of liver diseases position paper on acute liver failureHepatology 2012 55:965 [Google Scholar]
[5]. Bhatia V, Bavdekar A, Yachha SK, Management of acute liver failure in infants and children: consensus statement of the pediatric gastroenterology chapter IAPIndian Pediatr 2013 50:477-82. [Google Scholar]
[6]. Kaur S, Kumar P, Kumar V, Sarin SK, Kumar A, Aetiology and prognostic factor of acute liver failure in childrenIndian Pediatr 2013 50(7):677-79. [Google Scholar]
[7]. Grady JO’, Acute liver failurePost Grad Med J 2005 81(953):148-54. [Google Scholar]
[8]. O’Grady JG, Alexander GJ, Hayllar KM, Williams R, Early Indicators of prognosis in fulminant hepatic failureGastroenterology 1989 97:439-45. [Google Scholar]
[9]. Mita A, Hashikura Y, Tagawa T, Nakayama J, Kawakuba M, Miyagawa S, Expression of Fas ligand by hepatic macrophages in patients with fulminant hepatic failureAm J Gastroenterol 2005 100(11):2551-59. [Google Scholar]
[10]. Fuchs S, Bogomolski-Yahalom V, Paltiel O, Alkemak Z, Ischeamic hepatitis: clinical and laboratory observations of 34 patientsJ Clin Gastroenterol 1998 26:183-86. [Google Scholar]
[11]. Cassidy WM, Reynolds TB, Serum lactic dehydrogenases in the differential diagnosis of acute hepatocellular injuryJ Clin Gastroenterol 1994 19:118-21. [Google Scholar]
[12]. Ebert EC, Hypoxic liver injuryMayo Clin Proc 2006 81(9):1232-36. [Google Scholar]
[13]. Balasubramanian S, Kaarthigeyan K, Srinivas S, Rajeswari R, Serum ALT: LDH ratio in typhoid fever and acute viral hepatitisIndian Pediatr 2010 47:339-41. [Google Scholar]
[14]. Kotoh K, Enjoji M, Kato M, Kohjima M, Nakamuta M, Takayanagi R, A new parameter using serum lactate dehydrogenase and alanine amino transferase level is useful for predicting the prognosis of patients at an early stage of acute liver injury: A retrospective studyComparative Hepatology 2008 7:6 [Google Scholar]
[15]. Talwalkar SS, Bon Homme M, Miller JJ, Elin RJ, Ischaemia modified albumin, A marker of acute ischemic events: a pilot studyAnnals of Clinical and Laboratory Science 2008 38(2):132-37. [Google Scholar]
[16]. Behera S, Mangaraj M, Mohapatra PC, Diagnostic efficacy of Ischaemia modified albumin and its correlation with lipid profile, oxidative stress in acute myocardial infarct patients on admissionAsian Pac J Trop Dis 2012 2(1):62-65. [Google Scholar]
[17]. Arroyo V, Human serum albumin: Not just a plasma volume expanderHepatology 2009 50(2):355-57. [Google Scholar]
[18]. Jalan R, Schnurr K, Mookerjee RP, Sen S, Cheshire L, Hodges S, Alterations in the functional capacity of albumin in patients with decompensated cirrhosis is associated with increased mortalityHepatology 2009 50(2):555-64. [Google Scholar]
[19]. Zuwala-Jagietto J, Warwas M, Pazgan-Simon M, Ischaemia-Modified Albumin (IMA) is increased in patients with chronic hepatitis C infection and related to markers of oxidation stress and inflammationActa Biochim Pol 2012 59(4):661-67. [Google Scholar]
[20]. Chen CY, Tsai WL, Lin PJ, Shiesh SC, The value of serum Ischaemia modified albumin for assessing liver function in patients with chronic liver diseaseClin Chem Lab Med 2011 49(11):1817-21. [Google Scholar]
[21]. Cakir M, Karahan SC, Mentese A, Sag E, Cobanoglu U, Polat TB, Ischaemia modified Albumin levels in children with chronic liver diseaseGut Liver 2012 6(I):92-97. [Google Scholar]