Smoking in common parlance is an act of addiction which affects the well being of an individual. People practice different ways of smoking owing to their comfort and euphoria. Tobacco is the chief component in cigar smoking. These methods in particular are of two types: conventional smoking and reverse smoking. Among these two types, conventional smoking, where the lit end of the cigar (wrapped or rolled tobacco leaves in the form of a cylinder) is outside the mouth is very common. On the other hand, reverse smoking is a specific and peculiar custom that is much prevalent among low socio economic group population. In developing countries like India, this act of smoking is common among females. In southern part of India (Andhra Pradesh state) where the present study has been carried out, reverse smoking is practiced predominantly by women [1,2]. The peculiar nature of this particular habit is inserting the lit end of the cigar directly into the mouth [1,3].
Effects of reverse smoking habit are established through preliminary hospital-based studies [2] whereas effects of conventional smoking when compared with the reverse smoking are not many. With this background, we aimed to study and compare the clinical, cytological and histopathological changes among reverse smokers and conventional smokers, so as to identify early dysplastic changes of oral mucosa which enables necessary therapeutic interventions, thereby reducing the associated morbidity and mortality.
Materials and Methods
A cross-sectional observational study was carried out among the subjects attending the outpatient Department of Oral Medicine and Radiology, Vishnu Dental College, Bhimavaram, Andhra Pradesh, India with a self-reported habit of smoking for a period of 10-30 years. The sample was randomly selected. The study was carried out for a period of six months between December 2012 to May 2013.
A total of 40 subjects within the age group of 45-60 years participated in the study. Subjects who were not associated with tobacco smoking were excluded from the current study. Subjects participating in the study were explained about the intervention to be conducted on them. The purpose of the study was explained to each participant and a written informed consent was obtained from each subject before enrolling into the study. Ethical approval was obtained from Institutional research ethical committee of Vishnu dental college, Bhimavaram, Andhra Pradesh, India.
The sample was categorised into two groups
Group 1: 20 subjects with reverse smoking habit.
Group 2: 20 subjects with conventional smoking habit.
The clinical presentation of the palatal mucosa of all the study subjects was graded according to classification given by Alvarez Gómez GJ et al., followed by correlative histocytological investigations [3].
Procedure
The cytological smears were obtained before proceeding for the biopsy. The lesion area was scraped with a flat wooden spatula and was uniformly smeared on glass slides. It was then fixed in ethanol and was stained by Papanicolaou staining technique.
Biopsy procedure was carried out under strict aseptic conditions. A 5mm punch biopsy was performed from a representative area of the palatal mucosa under local anaesthesia. The obtained tissue was then fixed in 10% neutral buffered formalin and embedded in paraffin followed by staining with Haematoxylin and Eosin.
The clinical appearance [5] [Table/Fig-1,2] and grade of clinical presentation [3], the cytological staging [6] and histologic grading based on WHO system (2005- criteria used for dysplasia) [7] were used in diagnosing and grading of oral dysplasia [Table/Fig-3].
Palatal changes associated with reverse smoking.
(a) Palatal keratosis seen on palate. (b) Showing excresences on the palate.
(c) Depicting hyperpigmentation on the palate. (d) White patch seen on palate.
(e) Red areas seen on palate. (f) Depicting palatal carcinoma on the palate.
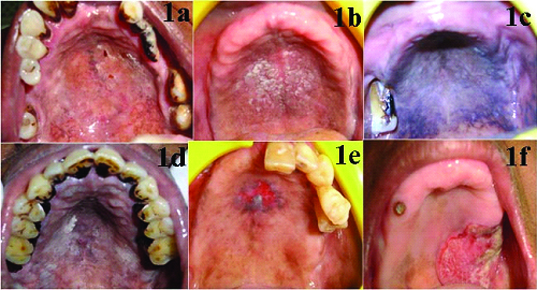
Palatal changes associated with reverse smoking [5].
| Palatal keratosis | Diffuse whitening of the palatal mucosa which may be mild, moderate or severe in intensity. It may occur independently or coexist with other components. They account for 55% of the palatal components.
|
| Excrescences | Excrescences comprise 1-3 mm elevated area, often with central red dots marking the orifices of the palatal mucosa glands and 46% of the palatal changes show excrescences. It represents the initial palatal reaction and they are generally transient. The milder forms of excrescence resemble the smoker’s palate seen in conventional smokers.
|
| Patches | Patches are well-defined, elevated plaques showing characteristic histologic features that differ from the features of leukoplakia. It accounts up to 12% of the palatal components.
|
| Red areas | Red areas are well-defined reddening of the palatal mucosa. Clinically, they are indistinguishable from erythroplakias. It accounts upto 2% of the palatal components. Nevertheless, they are the most serious, showing epithelial dysplasia in 52% of the cases. Long-term studies demonstrate a high rate of malignant transformation.
|
| Ulcerated areas | Ulcerated areas are characterized by crater-like ulcerations with deposits of fibrin often surrounded by keratinization. Ulcerations form only 2% of the palatal components. They represent a “burn” type reaction of the palatal mucosa from the intense heat of the lighted end of chutta.
|
| Nonpigmented areas | Non pigmented areas indicate areas of palatal mucosa which are clinically devoid of melanin pigmentation. It may result from following the regression of red areas. Loss of pigmentation may render the palatal mucosa more vulnerable to the action of carcinogens in tobacco.
|
| Multimorphic lesion | Various palatal components may coexist and they also occur in association with non-palatal lesions.
|
Clinically the palatal changes will be recorded and graded based on terms and degrees of severity [3].
| Grading | Clinical changes | Clinical appearance |
|---|
| Grade 0 | No palatal changes. | |
| Grade 1 | Mild palatal changes | Red circular areas over a slightly raised blanched mucosa of the glandular zone of the hard palate. |
| Grade 2 | Moderate palatal changes | Papules of 2-4mm with central umbilication less than 2mm of diameter. Moderate changes include hyperkeratinization and premalignant changes like Leukoplakia. |
| Grade 3 | Severe palatal changes | Papules greater than 4-5mm in size with central umblicus 2-4 mm in size or characterized by crater like ulcerations surrounded by keratinization. |
| Grade 4 | Palatal carcinoma | Exophytic and/or ulcerated lesion in oral mucosa of rapid evolution that clinically is compatible with oral carcinoma. |
The criteria used for cytological staging [6]:
Class I (Normal): Indicates that only normal cells were observed.
Class II (Atypical): Indicates the presence of minor atypia but no evidence of malignant changes.
Class III (Indeterminate): The cells display wider atypia that may be suggestive of cancer.
Class IV (Suggestive of cancer): A few cells with malignant characteristics or many cells with borderline characteristics.
Class V (Positive for cancer): Cells that is obviously malignant.
The criteria used for dysplasia [7]:
Hyperplasia: Describes increased cell numbers. This may be in the spinous layer leading to hyperplasia or acanthosis in the basal/parabasal cell layers.
Mild Dysplasia: Slight nuclear abnormalities, most marked in the basal third of the epithelial thickness. Cells show normal maturation and stratification. A few, but no abnormal mitoses may be present in the parabasal layers.
Moderate Dysplasia: More marked nuclear abnormalities are seen in the basal two-third of the epithelium. Cell maturation and stratification are evident in the upper layers. Mitoses are present in the parabasal and intermediate layers, but none is abnormal.
Severe Dysplasia: Marked nuclear abnormalities involve more than two-thirds of the epithelium. Mitoses, some of which are abnormal, may be present in the upper layers. Maturation and stratification was still seen in most superficial layers.
Carcinoma in situ: It is defined as ‘a lesion in which the full thickness, or almost the full thickness, of squamous epithelium shows the cellular features of carcinoma without stromal invasion.’ Requires top-to bottom change with undifferentiated, primitive cells from the basal layer to the topmost layer.
The collected data for each subject was entered into an excel sheet and subjected to statistical analysis.
Statistical Analysis
All the variables from the study were statistically analysed for the mean values, SD, standard error range, and p-value. Evaluation of results and statistical analysis was carried out using Student’s t-test, Chi-square test and Pearson correlation. In all the above tests, p-value < .05 was taken to be statistically significant, p-value >.05 was taken to be statistically not significant, and p-value < .001 was taken to be statistically highly significant. The data were analysed using SPSS.15 software.
Results
The demographic details of the study are given in [Table/Fig-4]. No subjects were dropped out during the study both in group 1 and group 2. The mean age of subjects in group 1 is 58.65±6.92 years and group 2 is 51.40±11.32 years. When the means of both the groups were compared, significant difference was observed in reverse smokers with a p-value of 0.019 [Table /Fig-4]. The gender distribution of the subjects in group 1 shows 15 females and 5 males. Group 2 shows 20 male subjects [Table/Fig-5].
Demographic statistics of both reverse smokers and conventional smokers.
| Habit | N | Mean | Deviation | Std. Error mean | p-value |
|---|
| Age | Reverse smokers | 20 | 58.65 | 6.923 | 1.548 | 0.019* |
| Conventional smokers | 20 | 51.40 | 11.325 | 2.532 |
*Student t- test.
Gender distribution of patients in both reverse smokers and conventional smokers.
| Habit | Total | p-value |
|---|
| Reverse smokers | Conventional smokers |
|---|
| Males | 5 | 20 | 25 | 0.001* |
| Females | 15 | 0 | 15 |
| Total | 20 | 20 | 40 |
* Chi –square test
When the frequency and duration of the habits are compared between the two groups, the frequency of smoking is much higher in conventional smokers and the duration of smoking is significantly higher in reverse smoking [Table/Fig-6].
Frequency and duration of smoking habits.
| Habit | N | Mean | Std. Deviation | Z-score | p-value |
|---|
| Frequency (per day) of Smoking | Reverse smoking | 20 | 2.60 | 1.314 | -2.919 | 0.004* |
| Conventional smoking | 20 | 5.20 | 3.365 |
| Total | 40 | | |
| Duration (in years) of Smoking | Reverse smoking | 20 | 26.50 | 10.273 | -2.531 | 0.011* |
| Conventional smoking | 20 | 19.75 | 5.955 |
| Total | 40 | | |
* Mann-Whitney U test
The clinical presentation of the palatal changes among group 1 and 2 subjects is depicted in [Table/Fig-7]. Majority of the subjects in group 1 were witnessed with palatal keratosis and white patch and in group 2, subjects were witnessed with nicotina palatii.
Clinical appearance in the palatal mucosa of reverse smokers and conventional smokers.
| Clinical appearance | Reverse smokers | Conventional smokers | Total |
|---|
| No palatal changes | 2 | 4 | 6 |
| 10.0% | 20.0% | 15.0% |
| Hyper pigmentation | 2 | 3 | 5 |
| 10.0% | 15.0% | 12.5% |
| Palatal keratosis | 4 | 0 | 4 |
| 20.0% | .0% | 10.0% |
| Palatal excresences | 1 | 0 | 1 |
| 5.0% | .0% | 2.5% |
| Excresences & keratosis | 1 | 0 | 1 |
| 5.0% | .0% | 2.5% |
| White patch | 4 | 0 | 4 |
| 20.0% | .0% | 10.0% |
| Nicotina palatii | 0 | 9 | 9 |
| .0% | 45.0% | 22.5% |
| Palatal erythema | 2 | 4 | 6 |
| 10.0% | 20.0% | 15.0% |
| Multimorphic palatal lesions | 2 | 0 | 2 |
| 10.0% | .0% | 5.0% |
| Chronic non healing ulcer | 2 | 0 | 2 |
| 10.0% | .0% | 5.0% |
| p-value | 0.004* |
*Chi–square test
The severity of clinical changes of the palatal mucosa in both the groups is depicted in [Table/Fig 8]. In group 1, 40% of the subjects (8) have shown moderate palatal changes and In 25% of the subjects (5) mild palatal changes and 15 % of the subjects (3) severe palatal changes and 10% of the subjects (2) with palatal carcinoma. In group 2, 80% of the subjects (16) have shown mild palatal changes and the remaining subjects showed no palatal changes. The severity of clinical changes in reverse smokers had shown statistically significant results with a p-value of 0.001 when compared to conventional smokers.
Severity of clinical palatal changes in reverse smokers and conventional smokers.
| | Graded clinical changes |
|---|
| No palatal changes | Mild palatal changes | Moderate palatal changes | Severe palatal changes | Palatal carcinoma | Total | p-value |
|---|
| Reverse smokers | Count | 2 | 5 | 8 | 3 | 2 | 20 | 0.001* |
| % within HABIT | 10.0% | 25.0% | 40.0% | 15.0% | 10.0% | 100.0% |
| Conventional smokers | Count | 4 | 16 | 0 | 0 | 0 | 20 |
| % within HABIT | 20.0% | 80.0% | .0% | .0% | .0% | 100.0% |
| Total | Count | 6 | 21 | 8 | 3 | 2 | 40 |
| % within HABIT | 15.0% | 52.5% | 20.0% | 7.5% | 5.0% | 100.0% |
Cytological staging [6] in group 1 revealed class I cytology in 35% of the subjects (7), 40% of the subjects (8) in group 2 and class II cytology in 55% of the subjects (11) in group 1, 60% of the subjects (12) in group 2. Class III cytology is observed in 10% of the subjects (2) of group 1. There is no statistical significant difference observed in cytological staging between the groups with a p-value of 0.35 [Table/Fig-9].
Cytological staging in reverse smokers and conventional smokers.
| CYTOLOGICAL STAGING | Total | p-value |
|---|
| CLASS I | CLASS II | CLASS III |
|---|
| Reverse smokers | 7 | 11 | 2 | 20 | 0.35 |
| 35.0% | 55.0% | 10.0% | 100.0% |
| Conventional smokers | 8 | 12 | 0 | 20 |
| 40.0% | 60.0% | .0% | 100.0% |
| Total | 15 | 23 | 2 | 40 |
| 37.5% | 57.5% | 5.0% | 100.0% |
*Chi –square test
Histopathological grading [7] of both the groups is shown in [Table/Fig-10], where the results in both the groups tend to show mild dysplastic features in majority of the subjects. Group 1 and group 2 revealed mild dysplastic features in 35% of the subjects and 15% of the subjects in group 1 showed moderate dysplastic features and significant difference was observed between the two groups with a p-value of 0.02.
Histopathological changes in reverse smokers and conventional smokers.
| Histopathological changes | Reverse smokers | Conventional smokers | Total |
|---|
| Hyper orthokeratinized epithelium | 2 | 4 | 6 |
| 10.0% | 20.0% | 15.0% |
| Hyper para Keratinized epithelium | 0 | 2 | 2 |
| .0% | 10.0% | 5.0% |
| Hyper ortho Keratinized epithelium with melanin pigmentation in basal layer | 3 | 1 | 4 |
| 15.0% | 5.0% | 10.0% |
| Hyper para keratinized epithelium with melanin pigmentation in basal layer | 0 | 2 | 2 |
| .0% | 10.0% | 5.0% |
| Inflammatory cells in connective tissue | 0 | 4 | 4 |
| .0% | 20.0% | 10.0% |
| Mild dysplasia | 7 | 7 | 14 |
| 35.0% | 35.0% | 35.0% |
| Hyper orthokeratosis with mild dysplasia | 3 | 0 | 3 |
| 15.0% | .0% | 7.5% |
| Moderate dysplasia | 3 | 0 | 0 |
| 15.0% | .0% | .0% |
| Invasive squamous cell carcinoma | 2 | 0 | 2 |
| 10.0% | .0% | 5.0% |
| p-value | 0.02* | | |
*Chi –square test.
Correlation between clinical appearance and other parameters in reverse smokers showed a significant positive correlation between the clinical appearance, graded clinical changes and cytological, histological changes [Table/Fig-11]. The results support that through the clinical appearance we can judge the severity of the lesion and its histopathological and cytopathological severity.
Correlation between clinical appearance and other parameters in reverse smokers.
| | Gradedclinical changes | Cytological staging | Histopatho-logical staging |
|---|
| Clinical appearance | Pearson Correlation | .732** | .751** | .676** |
| Sig. (2-tailed) | .000 | .000 | .001 |
| N | 20 | 20 | 20 |
*Pearson Correlation
Discussion
Tobacco is consumed in a variety of different ways, though smoking is the most prevalent form of its use. Cigars deliver nicotine both through smoke and direct oral contact with wrapped tobacco [8]. Chutta is a cigar made of tobacco leaves wrapped in cylindrical shape [5]. Chutta smoking is a popular form of tobacco use which is very much prevailed among the population of coastal belt region of Andhra Pradesh, India [9]. The habit of reverse smoking by holding the glowing end of chutta [3] within the oral cavity is better described in this part of India and is practiced extensively by older women living in rural areas [9]. The present study provides new insight into the underlying mucosal (palatal mucosa) changes both macroscopically and microscopically.
As a matter of fact, the act of reverse smoking leads to diverse changes in the palatal mucosa and these are often described as “palatal changes”. These changes may exist independently or in combination with each other and pose a different clinical picture such as palatal keratosis, excresences, patches, red areas, ulcerations and pigmentation changes [Table/Fig-1,2] [5]. These lesions can be multiple and has been studied macroscopically and microscopically by Van Wyk, Schwartz, Sutherland [1,10–12].
The damaging and harmful effects of tobacco usage on oral health are well recognised and several documents have reviewed the scientific evidence relating to the oral dysplastic changes attributable to tobacco use [13].
In majority of the times, the diagnosis and grading of oral epithelium dysplasia is truly based on a combination of architectural and cytological changes [13]. Currently, the gold standard procedure to assesss oral potentially malignant and malignant lesions seems to be microscopic evaluation of Haematoxylin and Eosin stained sections for the presence of architectural and cytological changes which in general are described as epithelial dysplasia [14]. In the present study, the same aforementioned gold standard method was followed to evaluate the lesions.
In the present study mean age of subjects in group 1 showed a significant difference when compared with the group 2. This shows that reverse smoking is observed only in elder age groups [9] [Table/Fig-4].
In the present study females were predominantly involved in reverse smoking to a greater extent than males [Table/Fig-5]. There are several explanations as why reverse smoking is predominantly accustomed by females in Coastal Andhra Pradesh [15,16]. There are few taboos involved in this habit, Firstly, females started smoking in the reverse way because they wanted to keep it secret from their husbands. Secondly, the strong winds, or splashing of water during household work, increase the chances of extinguishing the chutta if it is smoked in the conventional way. Thirdly, the chuttas are smoked in the reverse way to prevent hot ashes falling on children and clothes. Fourthly, treatment for toothache where the heat generated by reverse smoking probably produces a soothing sensation and then reverse smoking may continue as a habit [2]. For conventional smoking a different pattern is observed. This habit is practised to a far greater extent among males than females.
The frequency of smoking is much higher in conventional smokers when compared to reverse smoking i.e. even with small frequency of reverse smoking it can produce wide adverse effects. The duration of smoking is significantly higher in reverse smoking than the conventional smoking as most of the population in reverse smokers belong to older age group [Table/Fig-6].
In the present study, the common palatal change observed in reverse smokers was palatal keratosis, which is in accordance with the study of Alvarez Gómez GJ et al., and Mehta FS et al., [3,17], while among conventional smokers were those of Nicotina palatine owing to the effects of tobacco on oral mucosa [Table/Fig-7].
The present study reveals clinical changes in the palatal mucosa. With respect to that, in reverse smokers, majority (40%) of the subjects showed moderate changes while in conventional smokers, majority (80%) of the subjects showed mild palatal changes respectively [Table/Fig-8]. The severity of clinical changes in reverse smokers has shown statistically significant results when compared to conventional smokers. These findings were in accordance with those of Ortiz GM et al., who reported an increased incidence of palatal changes (96.7%) in reverse smokers [18]. According to Van Der EB et al., the prevalence rate of palatal lesions was found to be 55% among reverse smokers [19].
Our results are similar to the study conducted by Ramulu et al., suggesting there is association between smoking habits and various atypical changes [1]. Per se, the reverse smoking habit leads to tremendous (atypical) changes in the glandular zones of the palatal areas. There is an appreciable difference of palatal changes both in hard palate and soft palate. Since, soft palate usually contains less number of glands and are not backed by bone, the probability of occurrence of these changes is pretty much less in this region compared to hard palate region where the changes occur at a higher rate owing to its greater number of glands and are backed by bone.
These atypical changes are of mild and severe type where the mild atypical changes of the surface epithelium usually are confined to the ducts of the glands and to the surrounding epithelium. Severe atypical changes are witnessed in the lining of the epithelium of the ducts and also to a certain extent in the surrounding epithelium on the surface. Reddy et al., reported that earliest atypical changes in the orifices of the ducts of the glands are papules and is a consequence to hyperplasia of the mucous glands [20].
In the present study, out of 20 reverse smokers 2 subjects (10%) found to have carcinomatous transformation of palatal lesion [Table/Fig-8]. This observation is in accordance with the study conducted by Ramulu et al., who reported oral cancer in 2.4 % of the patients who were presented with nicotinic stomatitis due to reverse smoking which showed atypical changes to the extent of microinvasive carcinomas histopathologically [1]. They concluded that the chemicals released during reverse smoking induces hyperplasia and hypertrophy initially both in the ductal epithelium and surface epithelium. As a consequence, the ductal lining undergoes dysplastic changes from which micro invasive carcinoma and then invasive carcinoma may arise [21].
There exists an association between reverse smoking, nicotinic stomatitis and carcinoma of the hard palate. Reddy et al., stated that reverse smoker has a relative risk of developing carcinoma of hard palate 47 times more than non smoker [22]. According to Quigley et al., the excess heat generated (120°c) during smoking and higher content of nicotine is responsible for malignant transformation in reverse smokers [23].
The habit’s characteristic approach of placing fired end into the mouth causes the heat to lie inside the mouth with the lips providing the required seal. The unheated extreme of the cigar carries the air to the zone of combustion whilst the cigar/cigarette is kept moist (through lips), increases the time of consumption from 2 to 18 minutes. As the intern temperature of the cigar is increased over 760°c consequently the intra oral temperature is Raised around 120°c. This continuous encounter (based on the frequency and duration) of palatal mucosa to extreme temperatures results in thermal injury which along with products of combustion ultimately increases the frequency of lesions when compared to conventional smoking [3]
As reported by Van Der EB et al., majority of the palatal cancer cases were observed within the reverse smokers group [19]. On comparision of cytological findings, majority of the reverse smokers and conventional smokers had witnessed class II cytology with statistically significant results [Table/Fig-9]. These findings were in accordance with the study of Mehta FS et al., [15]. The reason might be that palatal lesions occurring in highly keratinized areas of the mouth hamper the exfoliation of possible atypical cells which arise from the deeper layers of the epithelium. Thus it appears that the reliability of cytological diagnosis is inversely associated with the degree of keratinization.
On comparing the histologic findings among reverse and conventional smokers, where the results in both the groups tend to show mild dysplastic features in majority of the subjects and few subjects showed moderate dysplastic features in group 1 with a significant difference [Table/Fig-10]. The present observation was in accordance with that of Reddy et al., [18,24], Ramulu et al., [1]. The present study showed the relationship of this habit to the development of macroscopic stomatitis nicotina and to the microscopic finding of epithelial atypia and even of carcinomatous changes without macroscopic evidence of palatal changes.
A significant positive correlation between the clinical appearance, graded clinical changes and cytological, histological changes was observed in reverse smokers [Table/Fig-11]. The above findings were in accordance with the study conducted by Mehta FS et al., [15,17].
Within its limitations, the present study had extracted the possible outcomes of the effects of tobacco smoking underlying sub clinically. The possible limitations in the current study would be less sample size, the future research is directed to overcome this obstacle and entail a definite probability of sub clinical effects of tobacco smoking.
Conclusion
Smoking in any form, either traditionally or with a peculiar habit of reverse smoking definitely alters the oral mucosa, in particular the palatal mucosa. Prevention of tobacco use is a key element in public health. Although the literature contains description of some of the toxic effects of handling tobacco, there has been very little evidence on the consequences of smoking underlying at clinical and cellular level.
Despite the relative paucity of existing scientific data, the need to assess and evaluate the underlying consequences of tobacco smoking both macroscopically and microscopically prompted us to conduct the current study. The present study is mainly intended to evaluate the clinical palatal changes by correlating with the cytological and histopathological findings of the affected mucosa (palatal mucosa). The importance of this correlation lies in the prime detection of high risk lesions at an infant stage and therefore aiding in treatment effective procedures.
The present study evidenced significant variations between the observed clinical palatal changes with that of cytological and histopathological findings. When compared to the conventional smokers, reverse smokers present clinically with aggressive changes of the palatal mucosa, although the cytological and histopathological features may correlate.
In conclusion, even though the clinical palatal changes appears to be normal there seems to be significant changes associated with the effect of smoking when observed through cytological and histopathological procedures. So, thus the habit of tobacco smoking may significantly cause the prompt changes where the individuals are at a greater risk of developing carcinomatous changes.
*Student t- test.
* Chi –square test
* Mann-Whitney U test
*Chi–square test
*Chi –square test
*Chi –square test.
*Pearson Correlation