Introduction
Attention-Deficit Hyperactivity Disorder (ADHD) is the most commonly diagnosed psychiatric disorder, occurring in 5-7% of children worldwide. Diagnosis is typically made in the school-aged children [1,2]. This disorder is defined as a stable pattern of attention deficit, hyperactivity and impulsive behaviours which is more severe than that usually noted in children of the same age or developmental level [3]. This disorder is categorized into three subtypes of combined, predominantly inattentive and predominantly hyperactive and impulsive [4]. Although many ADHD-related problems decline in puberty, ADHD-related secondary problems (antisocial behaviours, academic problems) could persist or be exacerbated [5,6]. Effective treatment promotes quality of life considerably [6–8]. On the other hand, this disorder leads to high individual and social costs [9]. The literature reported various prevalence rates in school-aged children. Farahat et al., in Egypt, Pineda et al., in Colombia, Pastura et al., in Brazil, and Sanchez et al., in Panama, have reported general prevalence of ADHD 6.9%, 16.4%, 8.6% and 7.4% respectively [2,10–12].
In Iran, several studies investigated this issue and all represented a relatively high prevalence of ADHD in school-aged children worldwide. According to the conducted investigations in different regions, various prevalence was reported. For example, Hebrani et al., study in Mashhad, Mosalanejad et al., study in Zahedan and Meysamie et al., study in Tehran reported general prevalence of this disorder 12.3 %, 15.4%, and 25% respectively [13–15].
In a systematic review of the published articles on ADHD prevalence in children and adolescents in Iran, inconsistent results were found [16].
Help-seeking pathway models propose a series of connections between initial recognition of the child’s mental health problem and the ultimate use of mental health services. For young children, the recognition of a mental health problem by parents or teacher is usually the first step of this process which could be followed by steps of seeking for evaluation, professional diagnosis and treatment. Several factors could influence this process, including predisposing factors such as age, gender, and socioeconomic status, system-related factors including treatment insurance, sources of routine pediatric care, training services, and disorder specifications including severity of behavioural problems from parents’ or teacher’s perspectives [17].
Aim
Because of the complications of ADHD and the importance of treatment in these patients, this research was conducted to determine the prevalence of ADHD in elementary school students of Shahrekord, Iran, and obstacles to seeking for mental health help these students.
Materials and Methods
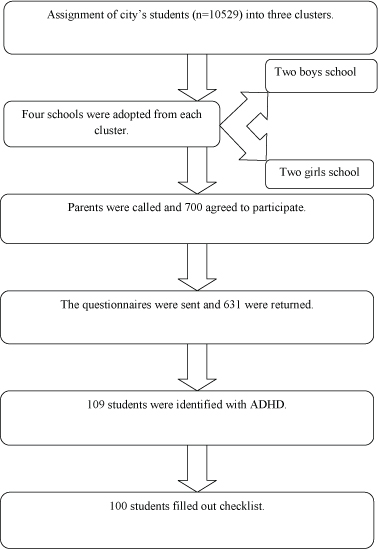
This study was cross-sectional and analytical. The study population consisted of 10,529 students aged 6-12 years in elementary schools for normal students in Shahrekord in academic year 2012-2013. The inclusion criteria were parents’ consent for participation in the study and studying in the school for normal students. To enroll the samples, we initially divided Shahrekord into three clusters namely eastern, central, and western (consisting of totally 53 schools), and selected two girls’ schools and two boys’ schools from each cluster [Table/Fig-1].
The first phase was conducted on a cross-sectional basis on a sample consisting of 700 students selected proportionate to gender and number of students in each grade. Initially, having attended the school and selected the sample after obtaining the principal’s consent, we called the parents and if they consented to participate in the study, a copy of Child Symptom Inventory-4 (CSI-4) and demographic data questionnaire, encoded in a closed envelope, was delivered to the student to have his/her parents fill out and return it to the school. Tavakoli et al., obtained the reliability of parents’ checklist 0.90 by test-retest [18]. Najafi et al., obtained the reliability of the questionnaire 0.92 by Cronbach’s alpha [19].
A checklist consisting of 20 items in five categories was used to assess obstacles to access to mental health services. Five items were assigned to system barriers, four items to barriers indicating stigma, three items to barriers indicating no perceived need, three items to financial barriers, and four items to barriers indicating negative expectations of treatment. Internal consistency of the instrument has already been reported as satisfactory (Cronbach’s=0.60) [17].
A copy of CSI-4 was filled out by the student’s teacher, as well. Demographic data questionnaire included age, gender, academic grade, parents’ education and occupation, treatment insurance coverage, having routine pediatric care, and some questions on history of ADHD diagnosis and treatment.
The students with history of ADHD diagnosis or treatment by specialist and those with suspected ADHD by CSI-4 (presenting six or more symptoms of ADHD) were categorized as suspected ADHD. These students were categorized into four groups with regard to help-seeking for mental health services, namely recognized (by parents), evaluated (by professionals such as psychiatrist or psychologist), diagnosed (by professionals), and treated. Of these students, those who underwent no treatment during the past 12 months were assessed for the obstacles to access to mental health services through interview with parents using a 20-item checklist.
CSI-4 is a tool for screening the most prevalent psychiatric disorders in children, developed by Gado and Sprafkin based on DSM-IV, consisting of two inventories for parents and teacher.
Group A inventory, which was used in this study measures three separate subtypes of ADHD consisting of predominantly hyperactive (items 1-9), predominantly inattentive (items 10-18), and combined. Each item is scored by a four-degree scale: Never, sometimes, often, and frequently.
Statistical Analysis
The data were analysed by SPSS. Descriptive data were analysed by percentage, mean, and standard deviation and inferential data by chi-square, correlation, McNemar, Mann-Whitney and t-test.
Results
Of 700 questionnaires distributed among the students, 631 (90%) were given back. Totally 631 grades 1 to 5 elementary school students consisting of 308 (48.8%) boys and 323 (51.2%) girls participated in this study. The mean age of the students was 9±1.4 (range; 6-12) years.
Based on parents questionnaires, totally 59 (9.3%) students had suspected ADHD (95%). From teachers’ viewpoints, 68 (10.8%) students had suspected ADHD, and totally 109 students (17.3%) were diagnosed with ADHD. The data are shown in [Table/Fig-2]. Frequency of subtypes of ADHD was not significantly different between male and female students (p=0.151).
Prevalence of attention-deficit/hyperactivity disorder for the subtypes by parents’ and teachers’ Child Symptom Inventory-4.
| Subtype | Parents | Teachers | ADHD diagnosed |
|---|
| Number | % | Number | % | Number | % |
|---|
| Mainly hyperactive and impulsive | 21 | 3.3 | 22 | 3.5 | 37 | 5.9 |
| Mainly inattentive | 16 | 2.5 | 31 | 4.9 | 37 | 5.9 |
| Combined | 22 | 3.5 | 15 | 2.4 | 35 | 5.5 |
| Total | 59 | 9.3 | 68 | 10.8 | 109 | 17.3 |
By the significance level in [Table/Fig-3], child gender, parents’ education, and father’s occupation were significantly associated with ADHD in children, but the type of housing was not significantly associated with ADHD diagnosis in children. By t-test, no significant association was seen between students’ age and ADHD (p=0.396). Mann-Whitney test indicated no association between students’ ADHD status and birth order.
Association of ADHD prevalence with demographic variables.
| Variable | ADHD | Total | p-value |
|---|
| No | % | No | % |
|---|
| Gender | Male | 63 | 10 | 308 | 48.8 | 0.025 |
| Female | 46 | 7.3 | 322 | 51.2 |
| Total | 109 | 17.3 | 631 | 100 |
| Father’s education | Illiterate | 4 | 0.63 | 21 | 3.3 | 0.003 |
| Elementary | 10 | 1.58 | 32 | 5.1 |
| Guidance | 23 | 3.64 | 83 | 13.2 |
| Diploma | 40 | 6.33 | 212 | 33.6 |
| Higher than diploma | 32 | 5.07 | 283 | 44.8 |
| Mother’s education | Illiterate | 2 | .31 | 15 | 2.4 | 0.004 |
| Elementary | 9 | 1.42 | 37 | 5.9 |
| Guidance | 20 | 3.16 | 85 | 13.5 |
| Diploma | 50 | 7.92 | 239 | 37.9 |
| Higher than diploma | 28 | 4.43 | 255 | 40.3 |
| Father’s occupation | Private | 68 | 10.77 | 325 | 51.5 | 0.004 |
| Civil servant | 38 | 6.02 | 300 | 47.55 |
| Jobless | 3 | 0.47 | 6 | .95 |
| Mother’s occupation | Housewife | 75 | 11.9 | 388 | 61 | 0.077 |
| Private | 5 | .8 | 50 | 8 |
| Civil servant | 29 | 4.6 | 193 | 31 |
| House type | Apartment | 63 | 10 | 366 | 58 | 0.936 |
| Villa | 46 | 7.3 | 265 | 42 |
McNemar test indicated no significant difference between teachers’ and parents’ viewpoints (p=0.401). However, there was a 17% difference between their viewpoints.
The patients were categorized into four groups for the steps of receiving mental health services, namely recognized by parents or teachers, evaluated, diagnosed, and treated, and the association of these steps with demographic characteristics and the symptom severity was assessed. The association between the steps of receiving services and the child gender is shown in [Table/Fig-4].
The association between the steps of receiving services and gender.
| Stage | Girls | Boys | Total | p-value |
|---|
| No | % | No | % | No | % |
|---|
| Identified | Yes | 17 | 37 | 32 | 50.8 | 49 | 45 | 0.107 |
| No | 29 | 63 | 31 | 49.2 | 60 | 55 |
| Assessed | Yes | 5 | 10.9 | 23 | 36.5 | 28 | 25.7 | 0.002 |
| No | 41 | 89.1 | 40 | 63.5 | 81 | 74.3 |
| Diagnosed | Yes | 3 | 6.5 | 17 | 27 | 20 | 18.3 | 0.005 |
| No | 43 | 93.5 | 46 | 73 | 89 | 81.6 |
| Treated | Yes | 4 | 8.7 | 13 | 20.6 | 17 | 15.6 | 0.074 |
| No | 42 | 91.3 | 50 | 79.4 | 92 | 84.4 |
Problem recognition rate was not significantly associated with the child gender, age, parents’ education and occupation, and having regular pediatric care, but significantly associated with attention deficit severity by parents’ questionnaire (p<0.001).
One hundred parents of the children with ADHD filled out the checklist of obstacles of access to mental health services. Results are shown in [Table/Fig-5].
Frequency of the obstacles of access to mental health services in students with ADHD.
| Obstacles | The relevant question | Score |
|---|
| Health and mental system | We could not take an appointment | 8 |
| Referring to a specialist is time-consuming and difficult. | 15 |
| The personnel dealt with disrespect. | 5 |
| Commuting to specialist office was difficult because of being far. | 10 |
| I did not know where or whom to refer to. | 47 |
| The counselor told us that our child has no problem. | 39 |
| Disease stigma | We were worried about relatives’ words. | 25 |
| We were afraid of his/her hospitalization | 4 |
| He did not come with us voluntarily. | 8 |
| Family members disagreed. | 26 |
| We felt embarrassed to talk with someone about his/her problems. | 14 |
| We thought that he/she did not have ADHD. | 4 |
| Lack of need | We thought that he/she had no important problem. | 41 |
| We thought that he/she recovered spontaneously. | 55 |
| We thought that he/she was able to solve problem. | 11 |
| Financial | Referring to a specialist is costly. | 17 |
| We did not have any treatment insurance. | 9 |
| Negative expectations | We thought that treatment was useless. | 14 |
| We did not trust psychologist and psychiatrist. | 10 |
| We referred previously and it was futile. | 15 |
| We were advised not to refer. | 9 |
| We were worried about drugs’ side effects. | 53 |
Discussion
Several studies have reported highly variable rates ranging from as low as 3% to as high as nearly 25% among school-aged children worldwide [20,21]. Different prevalence rates obtained in these studies could be attributable to different methodologies and instruments for assessment of ADHD in children as well as cultural differences. In the present study the prevalence was significantly higher in boys than girls. Although in a review article on ADHD prevalence in Iran, the subtype of mainly hyperactive was more prevalent in boys inattentive attention-deficit was more prevalent in girls [16]. In this study relative frequency of ADHD subtypes was not significantly different between girls and boys. Although the prevalence of this disease is variable, the mean prevalence of the disease is higher in men than women [22].
ADHD prevalence was significantly associated with parents’ education, as other studies found a significant association between ADHD among children and parents’ socioeconomic status and educational level [23,24]. In addition, there was a significant association between fathers’ occupation and ADHD prevalence [25]. Totally 45% of the parents were reported to recognize the problem in their children. According to Bussing et al., study in the USA, the parents were reported to recognize the problem in 93% of the boys and 82% of the girls, which is higher than the present study [17].
In this study, 36.5% of the children with suspected ADHD were examined by mental health specialist. Bussing et al., study also indicated that 39% of children with suspected ADHD were specially evaluated, and boys were more likely to be evaluated than girls by more than five times.
The diagnosis rate in children with ADHD was reported 18.3%. In the study of Bussing et al., the diagnosis rate was reported 32% (17), which is higher than the present study. The treatment rate was reported 15.6% in the present study. In Bussing et al., study 23% of children were reported to be under treatment during the study.
The above findings indicate that the access rate to mental health services is lower than that those reported in other countries, and also in girls than in boys, which could be due to the fact that ADHD is associated with fewer externalizing symptoms in girls. Generally, the most prevalent category of obstacles facing access to mental health services were those relevant to feeling no need, followed by negative expectations of treatment and mental health system problems. The barriers to treatment were driven by the beliefs of patients and their families, while others were the result of limitations in the health care system.
Limitations
Since study of socioeconomic status is difficult in Iran, to ensure the appropriateness of socioeconomic classification of students, we selected the students from the schools in downtown and suburbs, and non-public schools. To deal with dropouts, we considered a sample of 700 individuals. To facilitate comparison of the findings with previous studies, we excluded the students of sixth grade of elementary school from investigation.
Conclusion
The findings indicate that community training about mental health services and promotion of the system for referring patients to specialty centers could significantly improve access to the resources. In addition, public training is necessary to change the attitudes toward psychiatric drugs and the potential course of ADHD in case of lack of treatment.
[1]. Matthews M, Nigg JT, Fair DA, Attention deficit hyperactivity disorderCurr Top Behav Neurosci 2014 16:235-66. [Google Scholar]
[2]. Farahat T, Alkot M, Rajab A, Anbar R, Attention-Deficit Hyperactive Disorder among Primary School Children in Menoufia Governorate, EgyptInt J Family Med 2014 2014:257369 [Google Scholar]
[3]. Faraone SV, Sergeant J, Gillberg C, Biederman J, The worldwide prevalence of ADHD: is it an American condition?World Psychiatry 2003 2(2):104-13. [Google Scholar]
[4]. Skounti M, Philalithis A, Galanakis E, Variations in prevalence of attention deficit hyperactivity disorder worldwideEur J Pediatr 2007 166(2):117-23. [Google Scholar]
[5]. Fischer M, Barkley RA, Fletcher KE, Smallish L, The adolescent outcome of hyperactive children: predictors of psychiatric, academic, social, and emotional adjustmentJ Am Acad Child Adolesc Psychiatry 1993 32(2):324-32. [Google Scholar]
[6]. Bussing R, Zima BT, Gary FA, Garvan CW, Barriers to detection, help-seeking, and service use for children with ADHD symptomsJ Behav Health Serv Res 2003 30(2):176-89. [Google Scholar]
[7]. Klein RG, Mannuzza S, Olazagasti MA, Roizen E, Hutchison JA, Lashua EC, Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years laterArch Gen Psychiatry 2012 69(12):1295-303. [Google Scholar]
[8]. Caci H, Paille S, Attention-deficit/hyperactivity disorder in childhood/adolescence and impairments associated with daily life: French data from the European Lifetime Impairment SurveyArch Pediatr 2014 21(12):1283-92. [Google Scholar]
[9]. Pelham WE, Foster EM, Robb JA, The economic impact of attention-deficit/hyperactivity disorder in children and adolescentsAmbul Pediatr 2007 32(6):711-27. [Google Scholar]
[10]. Pineda DA, Lopera F, Palacio JD, Ramirez D, Henao GC, Prevalence estimations of attention-deficit/hyperactivity disorder: differential diagnoses and comorbidities in a Colombian sampleInt J Neurosci 2003 113(1):49-71. [Google Scholar]
[11]. Pastura G, Mattos P, Araujo AP, Prevalence of attention deficit hyperactivity disorder and its comorbidities in a sample of school-aged childrenArquivos de neuro-psiquiatria 2007 65(4A):1078-83. [Google Scholar]
[12]. Sanchez EY, Velarde S, Britton GB, Estimated prevalence of attention-deficit/hyperactivity disorder in a sample of Panamanian school-aged childrenChild Psychiatry Hum Dev 2011 42(2):243-55. [Google Scholar]
[13]. Hebrani P, Abdolahian E, Behdani F, Vosoogh I, Javanbakht A, The prevalence of attention deficit hyperactivity disorder in preschool-age children in Mashhad, north-East of IranArch Iran Med 2007 10(2):147-51. [Google Scholar]
[14]. Mosalanejad M, Mosalanejad L, Lashkarpour K, Prevalence of ADHD among students of zahedan university of medical science in iranIran J Psychiatry Behav Sci 2013 7(2):83-90. [Google Scholar]
[15]. Meysamie A, Fard MD, Mohammadi MR, Prevalence of Attention-Deficit/Hyperactivity Disorder Symptoms in Preschool-aged Iranian ChildrenIran J Pediatr 2011 21(4):467-72. [Google Scholar]
[16]. Shooshtary MH, Chimeh N, Najafi M, Mohamadi MR, Yousefi-Nouraie R, Rahimi-Mvaghar A, The prevalence of Attention Deficit Hyperactivity Disorder in Iran: A systematic reviewIran J Psychiatry 2010 5(3):88-92. [Google Scholar]
[17]. Bussing R, Zima BT, Gary FA, Garvan CW, Barriers to detection, help-seeking, and service use for children with ADHD symptomsJ Behav Health Serv Res 2003 30(2):176-89. [Google Scholar]
[18]. Tavakolizadeh J, Epidemiology of attention–deficit/hyperactivity disorder at primary school pupils in GonabadAndisheh Va Raftar Quarterly 1989 3(1):2 [Google Scholar]
[19]. Najafi M, Mohammadi MR, Assari S, Basirnia A, Tehranidoost M, Alaghband-rad J, Improving the Dictation in Attention Deficit Hyperactivity Disorder by Using Computer Based Interventions: A Clinical TrialIran J Psychiatry 2006 1(3):123-27. [Google Scholar]
[20]. Swanson JM, Sergeant JA, Taylor E, Sonuga-Barke EJ, Jensen PS, Cantwell DP, Attention-deficit hyperactivity disorder and hyperkinetic disorderLancet 1998 351(9100):429-33. [Google Scholar]
[21]. Bianchini R, Postorino V, Grasso R, Santoro B, Migliore S, Burlo C, Prevalence of ADHD in a sample of Italian students: a population-based studyRes Dev Disabil 2013 34(9):2543-50. [Google Scholar]
[22]. Erskine HE, Ferrari AJ, Nelson P, Polanczyk GV, Flaxman AD, Vos T, Epidemiological modelling of attention-deficit/hyperactivity disorder and conduct disorder for the Global Burden of Disease Study 2010J Child Psychol Psychiatry 2013 54(12):1263-74. [Google Scholar]
[23]. Pineda DA, Lopera F, Henao GC, Palacio JD, Castellanos FX, Confirmation of the high prevalence of attention deficit disorder in a Colombian communityRev Neurol 2001 32(3):217-22. [Google Scholar]
[24]. DeWolfe N, Byrne JM, Bawden HN, ADHD in preschool children: parent-rated psychosocial correlatesDev Med Child Neurol 2000 42(12):825-30. [Google Scholar]
[25]. Bener A, Kamal M, Predict attention deficit hyperactivity disorder? Evidence -based medicineGlobal J Health Sci 2014 6(2):47-57. [Google Scholar]