Management of Chronic Periodontitis Using Chlorhexidine Chip and Diode Laser-A Clinical Study
Kachapilly Arun Jose1, Majo Ambooken2, Jayan Jacob Mathew3, Annie Valayil Issac4, Ajithkumar Parachalil Kunju5, Renjith Athirkandathil Parameshwaran6
1 Post Graduate Student, Department of Periodontics, Mar Baselios Dental College, Kothamangalam, Kerala, India.
2 Professor and Head, Department of Periodontics, Mar Baselios Dental College, Kothamangalam, Kerala, India.
3 Professor, Department of Periodontics, Mar Baselios Dental College, Kothamangalam, Kerala, India.
4 Post Graduate Student, Department of Periodontics, Mar Baselios Dental College, Kothamangalam, Kerala, India.
5 Post Graduate Student, Department of Periodontics, Mar Baselios Dental College, Kothamangalam, Kerala, India.
6 Post Graduate Student, Department of Periodontics, Mar Baselios Dental College, Kothamangalam, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kachapilly Arun Jose, Post Graduate Student, Department of Periodontics, Mar Baselios Dental College, Kothamangalam, Kerala-686691, India.
E-mail: tsbkgem@gmail.com
Introduction
The use of adjuncts like chlorhexidine local delivery and diode laser decontamination have been found to improve the clinical outcomes of scaling and root planing in non-surgical periodontal therapy in patients with chronic periodontitis.
Aim
To evaluate the effects of diode laser and chlorhexidine chip as adjuncts to scaling and root planing in the management of chronic periodontitis. The objective is to evaluate the outcome of chlorhexidine chip and diode laser as adjuncts to scaling and root planing on clinical parameters like Plaque Index, Gingival Index, probing pocket depth and clinical attachment level.
Study and Design
Department of Periodontics. Randomized clinical trial with split mouth design.
Materials and Methods
Fifteen chronic periodontitis patients having a probing pocket depth of 5mm-7mm on at least one interproximal site in each quadrant of the mouth were included in the study. After initial treatment, four sites in each patient were randomly subjected to scaling and root planing (control), chlorhexidine chip application (CHX chip group), diode laser (810 nm) decontamination (Diode laser group) or combination of both (Diode laser and chip group). Plaque Index (PI), Gingival Index (GI), probing pocket depth (PPD) and clinical attachment level (CAL) were assessed at baseline, one month and three months.
Statistical analysis
Results were statistically analysed using paired T test, one-way ANOVA, Tukey’s HSD test and repeated measure ANOVA.
Results
Post-treatment, the test and control sites showed a statistically significant reduction in PI, GI, PPD, and CAL. After three months, a mean PPD reduction of 1.47±0.52 mm in control group, 1.40±0.83 mm in diode laser group, 2.67±0.62 mm in CHX group, and 2.80± 0.77 mm in combination group was seen. The mean gain in CAL were 1.47±0.52 mm in the control group, 1.40±0.83 mm in diode laser group, 2.67± 0.49 mm in CHX group and 2.67± 0.82 mm in combination group respectively. The differences in PPD reduction and CAL gain between control group and CHX chip and combination groups were statistically significant (p<0.05) at three months, whereas, the diode laser group did not show any significant difference from the control group.
Conclusion
Chlorhexidine local delivery alone or in combination with diode laser decontamination is effective in reducing probing pocket depth and improving clinical attachment levels when used as adjuncts to scaling and root planing in non-surgical periodontal therapy of patients with chronic periodontitis.
Diode laser decontamination, Local drug delivery, Scaling and root planing
Introduction
Periodontal diseases are one of the most common afflictions of mankind in terms of global prevalence. The initiation and progression of periodontal diseases are closely associated with pathogenic bacteria present in the sub gingival biofilm [1]. Mechanical debridement of these bacteria via scaling and root planing is the cornerstone of successful periodontal treatment, which can be accomplished by non-surgical or surgical approach [2]. Majority of the periodontal patients can be managed by non-surgical periodontal treatment. Hence, various adjuncts to scaling and root planing have been introduced into periodontal practice over the years [3]. Among these, local drug delivery and laser treatment have attracted considerable attention in the past two decades.
The concept of local drug delivery is based on the presumption that an antimicrobial agent placed directly into the pocket shall provide prolonged higher concentrations of the drug locally without any systemic side effects [4]. A number of antibiotics, both commercially available and indigenously prepared, have been employed as adjuncts to mechanical instrumentation in the management of periodontal diseases. Different antibiotics such as tetracycline, nitroimidazoles, fluoroquionolones and macrolides have been used as local drug delivery agents in various studies with promising clinical and microbiological results [5,6].
Chlorhexidine, the most widely used topical antiseptic and antiplaque agent in periodontics, has also been used as an agent for local drug delivery. A recent meta analysis [7] on the effect of local drug delivery in chronic periodontitis patients reported statistically significant reductions in pocket depth following local delivery of chlorhexidine. Chlorhexidine local delivery devices are usually available in the form of biodegradable chips or gels. Previous studies using chlorhexidine chip have suggested it as an effective adjunct to scaling and root planing in the treatment of chronic periodontitis [5,8].
Lasers were introduced into periodontal practice at the turn of this century. The suggested applications of lasers in periodontal treatment are manifold. They are used for intraoral soft tissue procedures such as frenectomy, gingivectomy, gingivoplasty, de-epithelization of reflected flaps, removal of granulation tissue, second stage of dental implants, lesion ablation, coagulation of free gingival graft donor sites and gingival depigmentation [9]. The non-surgical laser assisted periodontal therapy includes preprocedural disinfection, sub gingival curettage, sulcular debridement and decontamination [10].
The microbiological effects of laser decontamination is perhaps a lesser investigated aspect of lasers in periodontal treatment. Just as conventional root debridement removes biofilm and accretions from the hard tooth surface; laser decontamination removes biofilm within the necrotic tissue of the pocket wall. The laser energy interacts strongly with inflamed tissue components (from preferential absorption by chromophores, which are more abundant in diseased tissues) and less strongly with healthy tissue. This nonsurgical therapy uses very low settings and decontaminates rather than cutting the tissue [11].
In spite of being the two prominent adjuncts to scaling and root planing, only few studies have compared local drug delivery and lasers in the management of periodontal diseases. Birang et al., investigated the effects of diode laser and chlorhexidine gel as adjuncts to scaling and root planing in the treatment of chronic periodontitis and found that both modalities improved periodontal and microbiological indices compared to SRP alone [12]. Noguchi et al., studied the combined effect of Nd: YAG laser irradiation along with local application of antibiotic into periodontal pockets [13].
Aim
The present study is being undertaken to compare the effects of a diode laser (Picasso, AMD diode laser) and a chlorhexidine chip (Periocol CG) alone and in combination when used as adjuncts to scaling and root planing in the management of chronic periodontitis.
Materials and Methods
The study was conducted in the outpatients Department of Periodontics, Mar Baselios Dental College, and Kothamangalam. The study design was a prospective randomized single blinded clinical trial. Randomization was done by chit method. The study was approved by the institutional ethical committee. Fifteen patients fulfilling the inclusion and exclusion criteria were included in the study. There were 9 males and 6 females belonging to the age group of 30 – 60 years. The purpose of the study was explained to the patients and written informed consent was obtained.
Inclusion Criteria
Presence of a minimum of 15 teeth.
One interproximal site with probing pocket depth measuring 5mm-7mm in each quadrant.
Patients who are non-smokers.
Patients who are co-operative and able to attend the hospital for regular follow-up.
Exclusion Criteria
Patients suffering from any known systemic disease.
Patients who had received any known surgical or nonsurgical periodontal therapy within six months of the start of the study.
Patients who had taken antibiotics, chemotherapeutic mouth rinses within the last six months of the start of the study.
Patients with known hypersensitivity to chlorhexidine.
In all selected patients, a full mouth supragingival ultrasonic scaling was done. At the start of the study oral hygiene instructions were given and clinical parameters namely Plaque Index (PI), Gingival Index (GI) [14], probing pocket depth (PPD) and clinical attachment level (CAL) were recorded in all selected patients [Table/Fig-1a].
Probing pocket depth measured using stent: a) Baseline; b) 1 month; c) 3 months.

After 2 weeks in each patient one interproximal site in each quadrant with a probing pocket depth of 5mm-7mm was randomly assigned to receive one of the following treatment modalities by chit method. One of the site assigned as control group was subjected to scaling and root planing (SRP). The other three sites in addition to SRP received laser decontamination (diode laser group), chlorhexidine chip application (CHX chip group) or both (diode laser and chip group). In the control site scaling and root planing (SRP) was done by area specific curettes (Hu – Friedy Chicago IL). Following SRP the laser treatment was performed by Gallium-Aluminium -Arsenide (GaAlAs) diode laser (AMD, Picasso U.S.A) with a tip diameter of 400 μm, optical fiber that emitted light at wavelength of 810nm. The fiber was inserted into the periodontal pocket (1mm short of measured periodontal pocket depth) almost parallel to the tooth and moving from apical to coronal directions continuously. Power setting of 0.5 watts in continuous mode and time duration of 10 seconds per site was used. Both patient and operator wore protective eyeglasses during laser decontamination [15].
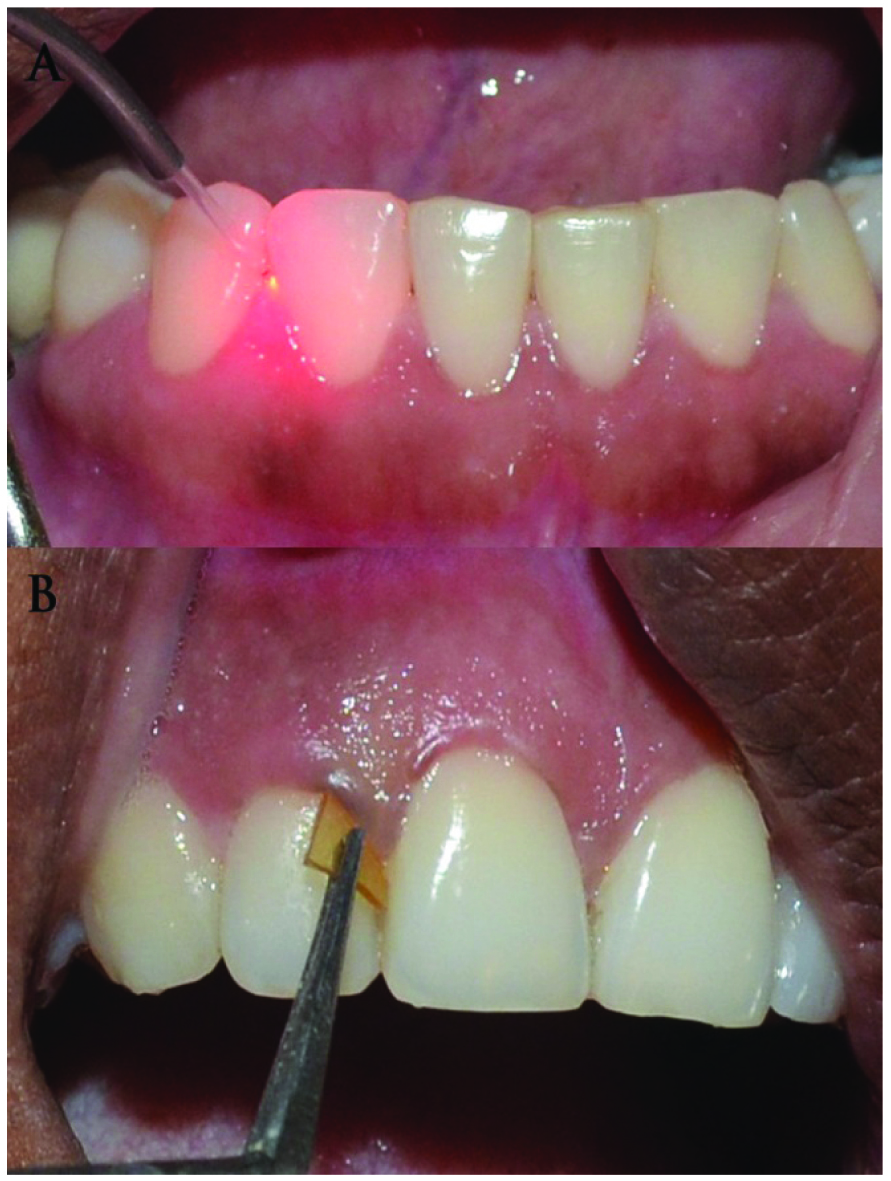
Chlorhexidine Chip placement [Table/Fig-2]: Following SRP the area was dried, and the chlorhexidine chip (Periocol –CG, Eucare pharmaceuticals, Chennai) was inserted into periodontal pocket with tweezers. The flat end of chlorhexidine chip was grasped with a sharp tweezer and the curve end was first inserted into periodontal pocket. Periodontal dressing (Coe-pak, GC U.S.A.) was placed on sites where chlorhexidine chip application was done. All the patients were recalled after 10 days for evaluation of any displacement of chip. Each chip contains approximately 2.5mg of chlorhexidine in a biodegradable matrix of collagen type I derived from the air bladder of fresh water fishes. The size of the chip is 4x5mm and thickness is 0.25-0.32mm, and its weight is about 10mg. It is resorbed in 30 days; however, the coronal edge is degraded in just 10 days. Laser decontamination and CHX chip application: Laser decontamination procedure was performed which was followed by chlorhexidine chip application. Re-evaluation and all clinical parameters were recorded at 1 month and 3 months [Table/Fig-1b&c]. The data was recorded at all intervals by a same examiner who was blinded for the procedure.
a) Laser decontamination; and b) chlorhexidine chip application.
Statistical Analysis
Statistical analyses were performed using SPSS 16.0. Descriptive analyses were performed by the calculation mean and SD. The data were analysed by paired t-test, one-way-ANOVA, Tukey’s HSD test and repeated measure ANOVA. A statistical significance was assumed when p<0.05.
Results
All the15 subjects completed the study uneventfully.
Intragroup Comparison
The baseline values of all four parameters were not statistically significant between any groups as determined by one-way ANOVA. Tukey’s HSD test was done to analyse statistical significant difference between different groups at one month and three months. The mean reduction in plaque index score [Table/Fig-3], Gingival Index score [Table/Fig-4], mean reduction in probing pocket depth [Table/Fig-5] and mean gain in relative clinical attachment level [Table/Fig-6] were statistically significant between both the interval i.e. baseline to one month (p< 0.01) and baseline to three months (p<0.01) in all the four groups.
Mean plaque index scores in different groups at different observation periods.
| Group | Observation period | Mean± SD | Comparison | Mean± SD | p-value |
|---|
| SRP (control) | Base Line (BL) | 2.03±0.16 | | | |
| 1 month (1M) | 1.28±0.35 | BL Vs 1M | 0.75±0.44 | <0.001 |
| 3 month (3M) | 0.73±0.41 | BL Vs 3M | 1.30±0.41 | <0.001 |
| Diode Laser | Base Line (BL) | 2.05±0.17 | | | |
| 1 month (1M) | 1.27±0.33 | BL Vs1M | 0.78±0.36 | <0.001 |
| 3 month (3M) | 0.72±0.39 | BL Vs 3M | 1.33±0.42 | <0.001 |
| CHX chip | Base Line (BL) | 2.07±0.24 | | | |
| 1 month (1M) | 1.23±0.35 | BL Vs 1M | 0.83±0.50 | <0.001 |
| 3 month (3M) | 0.60±0.16 | BL Vs 3M | 1.46±0.33 | <0.001 |
| Diode Laser+ Chip | Base Line (BL) | 2.05±0.24 | | | |
| 1 month (1M) | 1.25±0.33 | BL Vs 1M | 0.80±0.46 | <0.001 |
| 3 month (3M) | 0.62±0.19 | BL Vs 3M | 1.43±0.24 | <0.001 |
Mean gingival index scores in different groups at different observation periods.
| Group | Observation period | Mean± SD | Comparison | Mean± SD | p-value |
|---|
| SRP (control) | Base Line (BL) | 2.13±0.23 | | | |
| 1 month (1M) | 1.43±0.44 | BL Vs 1M | 0.70±0.57 | <0.001 |
| 3 month (3M) | 0.82±0.51 | BL Vs 3M | 1.32±0.49 | <0.001 |
| Diode Laser | Base Line (BL) | 2.10±0.30 | | | |
| 1 month (1M) | 1.40±0.39 | BL Vs1M | 0.70±0.52 | <0.001 |
| 3 month (3M) | 0.83±0.47 | BL Vs3M | 1.26±0.61 | <0.001 |
| CHX chip | Base Line (BL) | 2.12±0.27 | | | |
| 1 month (1M) | 1.38±0.42 | BL Vs 1M | 0.73±0.53 | <0.001 |
| 3 month (3M) | 0.78±0.36 | BL Vs 3M | 1.33±0.51 | <0.001 |
| Diode Laser+ Chip | Base Line (BL) | 2.15±0.26 | | | |
| 1 month (1M) | 1.35±0.41 | BL Vs1M | 0.80±0.46 | <0.001 |
| 3 month (3M) | 0.77±0.33 | BL Vs 3M | 1.38±0.51 | <0.001 |
Mean PPD in different groups at different observation periods.
| Group | Observation period | Mean± SD | Comparison | Mean± SD | p-value |
|---|
| SRP (control) | Base Line (BL) | 6.07±0.80 | | | |
| 1 month (1M) | 4.80±0.86 | BL Vs 1M | 1.27±0.46 | <0.001 |
| 3 month (3M) | 4.60±0.74 | BL Vs 3M | 1.47±0.52 | <0.001 |
| Diode Laser | Base Line (BL) | 6.13±0.83 | | | |
| 1 month (1M) | 4.80±0.86 | BL Vs 1M | 1.33±0.82 | <0.001 |
| 3 month (3M) | 4.73±0.88 | BL Vs 3M | 1.40±0.83 | <0.001 |
| CHX chip | Base Line (BL) | 6.00±0.85 | | | |
| 1 month (1M) | 3.47±0.83 | BL Vs 1M | 2.53±0.52 | <0.001 |
| 3 month (3M) | 3.33±0.90 | BL Vs 3M | 2.67±0.62 | <0.001 |
| Diode Laser+ Chip | Base Line (BL) | 6.07±0.80 | | | |
| 1 month (1M) | 3.53±.92 | BL Vs 1M | 2.53±0.52 | <0.001 |
| 3 month (3M) | 3.27±0.96 | BL Vs 3M | 2.80±0.77 | <0.001 |
Mean rCAL in different groups at different observation periods.
| Group | Observation period | Mean± SD | Comparison | Mean± SD | p-value |
|---|
| SRP (control) | Base Line (BL) | 11.47±1.40 | | | |
| 1 month (1M) | 10.20±1.26 | BL Vs 1M | 1.27±0.46 | <0.001 |
| 3 month (3M) | 10.0±1.06 | BL Vs 3M | 1.47±0.52 | <0.001 |
| Diode Laser | Base Line (BL) | 11.40±1.29 | | | |
| 1 month (1M) | 10.07±0.96 | BL Vs 1M | 1.33±0.82 | <0.001 |
| 3 month (3M) | 10.00±1.0 | BL Vs 3M | 1.40±0.83 | <0.001 |
| CHX chip | Base Line (BL) | 11.53±1.24 | | | |
| 1 month (1M) | 8.93±0.88 | BL Vs 1M | 2.60±0.51 | <0.001 |
| 3 month (3M) | 8.87±0.92 | BL Vs 3M | 2.67±0.49 | <0.001 |
| Diode Laser+ Chip | Base Line (BL) | 11.47±0.92 | | | |
| 1 month (1M) | 9.0±0.53 | BL Vs 1M | 2.47±0.52 | <0.001 |
| 3 month (3M) | 8.80±0.56 | BL Vs 3M | 2.67±0.82 | <0.001 |
Intergroup Comparison
The change in mean reduction of PPD compared to control group was 0.06mm, 1.20mm and 1.33mm in diode laser group, Chlorhexidine chip group and combination group respectively. Comparison of SRP with diode laser group showed insignificant result in PPD reduction (p<0.994) and mean gain in rCAL (p<0.993). However, comparison of SRP with CHX chip group and combination group revealed statistically significant improvement in PPD and rCAL (p< 0.01). Comparison of PI and GI based on groups at one month and three months shows no significant changes between any groups (p>0.05). Comparison between adjunct groups showed significant difference in PPD reduction and mean gain in CAL except between CHX group and combination group [Table/Fig-7,8].
Comparison of different groups for mean PPD reduction at 1 month and 3 months.
| Probing pocket depth | 1 month | 3 months |
|---|
| SRP (control) | | Mean Difference | p-value | Mean Difference | p-value |
|---|
| Diode laser | -0.06667 | 0.990 | 0.06667 | 0.994 |
| CHX Chip* | -1.26667 | <0.001 | -1.20000* | <0.001 |
| Diode laser + chip* | -1.26667* | <0.001 | -1.33333* | <0.001 |
| Diode laser | CHX Chip* | -1.20000* | <0.001 | -1.26667* | <0.001 |
| Diode laser + chip* | -1.20000* | <0.001 | -1.40000* | <0.001 |
| CHX Chip | Diode laser + chip | 0.00000 | 0.999 | -0.13333 | 0.953 |
*denotes significant difference.
Comparison of different groups for mean difference in rCAL gain at 1 month and 3 months *denotes significant difference.
| Clinical attachment level | 1 month | 3 months |
|---|
| SRP (control) | | Mean Difference | p-value | Mean Difference | p-value |
|---|
| Diode laser | -0.06667 | 0.990 | 0.06667 | 0.993 |
| CHX Chip* | -1.33333 | <0.001 | -1.20000 | <0.001 |
| Diode laser + chip* | -1.20000 | <0.001 | -1.20000 | <0.001 |
| Diode laser | CHX Chip* | -1.26667 | <0.001 | -1.26667 | <0.001 |
| Diode laser + chip* | -1.13333 | <0.001 | -1.26667 | <0.001 |
| CHX Chip | Diode laser + chip | 0.13333 | 0.926 | 0.00000 | 0.999 |
Discussion
Periodontal diseases comprise a group of chronic inflammatory lesions initiated and propagated by the accumulation of sub gingival biofilm. The removal of these biofilms and their retentive factors like calculus remains the cornerstone of the periodontal therapy. Mechanical sub gingival debridement i.e., scaling and root planing is considered as the gold standard of nonsurgical periodontal procedure. Previous studies indicates that the treatment of pockets by scaling and root planing followed by routine maintenance therapy every three months results in the maintenance of attachment levels and the reduction of probing depths [16,17]. In view of the current knowledge related to the nature of disease progression and studies showing that deep pockets can be maintained without further attachment loss, our approach to surgical pocket therapy has been changing. Periodontal disease therapy has therefore been directed at altering the periodontal environment to one which is less conducive to the retention of bacterial plaque [18].
Scaling and root planing has been shown to be an effective treatment for periodontitis. Mechanical therapy may however fail to eliminate the pathogenic bacteria because of their location within gingival tissues or in other areas inaccessible to periodontal instruments [19]. As the depth increases to ≥ 5mm, scaling and root planing becomes progressively less effective [20]. This has led to the development of alternative or adjunct treatment that might provide added benefits along with scaling and root planing. Mechanical and adjunct measures to minimize or eliminate bacterial plaque have been used in periodontal therapy in the past with varying results. Clinical trials on local drug delivery using chlorhexidine chip and diode laser decontamination have reported conflicting results in clinical and microbiological parameters of periodontal disease.
The present study was done to compare the effects of chlorhexidine chip, diode laser irradiation and the combination of both as adjuncts to SRP. A split mouth design involving one interproximal site from each quadrant was selected. In this type of study design, the patient is matched to himself, or serves as his own control, is recognized as having the ability to greatly facilitate the interpretation of trials by minimizing the effects of inter-patient variability. However, in split mouth design, when comparing different treatment modes within the same dentition, carry across or spill-over effects may occur [21]. Hence, to eliminate the carry-across effects on experimental sites, the present study randomly selected sites which were at least three teeth apart, possibly minimizing the interaction between therapy modes [22]. No side effects were observed or reported subsequent to the chlorhexidine chip application and laser decontamination, which indicated the safety of the procedure.
Even though oral prophylaxis was done at baseline, it was repeated after 2 weeks, because to standardize and compare with gold standard procedures of non surgical therapy and to avoid bias.
The inter group comparison of plaque index and gingival index showed insignificant differences between all groups at three months. However, more reduction was seen with test groups when compared with control (SRP) group. This might be attributable to the added interventions at the test sites.
Present study showed no significant improvement in pocket depth and clinical attachment gain in laser group when compared to control group. This result was controversial to studies conducted by Moritz A et al., Dukic et al., that showed a significant improvement [23,24]. This conflicting result may be due to the higher power settings and multiple radiations used in those studies.
To augment mechanical debridement, topical antiseptics are used to kill periodontal pathogens at the initial therapy and to suppress their repopulation in the maintenance phase. This concept of controlled- release local delivery of therapeutic agents was developed into a viable concept by Dr. Max Goodson in 1979. Local delivery systems containing antibiotics or antiseptic drugs allow the therapeutic agents to be targeted to the diseased site with minimal systemic effects. Local delivery systems when retained in the pocket can release the antimicrobial agents at levels that are 10-100 folds higher than the levels that can be delivered by systemic antibiotics. This approach also addresses the critical concern of unnecessarily exposing the patient to large doses of systemic antibiotics, which can also result in bacterial resistance. Chlorhexidine has wide spectrum of activity encompassing gram-positive and gram negative bacteria, yeast and some lipophilc viruses. Friedman and Golomb developed the first slow-release device containing chlorhexidine. Controlled delivery system has duration of drug release more than 24 hours. The effects of locally delivered controlled-release chlorhexidine have been shown to be evident upto 11weeks [25] which corresponds to 3 months. In this study CHX chip group comparison with control group showed statistically significant reduction in PPD and mean gain in CAL. Birang et al., Puri K et al., Kumar AJ et al., Grover V et al., and Kondreddy K et al., reported results similar to our study [12,26–29].
Intergroup comparison of test groups revealed that the CHX chip group and combination of laser decontamination and chlorhexidine chip group showed statistically significant difference in PPD reduction and gain in CAL compared to diode laser group at three months. But comparing chlorhexidine group with combination group there was no statistical significance this can be interpreted in two ways. On one hand, the results of single laser decontamination can be enhanced by the subsequent placement of chlorhexidine chip into a periodontal pocket. Conversely, there is no added benefit of laser decontamination of a pocket prior to local delivery of chlorhexidine.
Limitations
There were some limitations like study period was too short and study population was too less to come to a final conclusion and no microbial evaluation was done to evaluate the antimicrobial effect of both laser and chlorhexidine chip.
Conclusion
Within the limitations of the present study, the following conclusions may be derived chlorhexidine local delivery alone or in combination with diode laser decontamination is effective in improving oral hygiene, reducing gingival inflammation, reducing probing pocket depth and improving clinical attachment levels when used as adjuncts to scaling and root planing in non-surgical periodontal therapy of patients with chronic periodontitis. Adjunctive use of a single application of diode laser decontamination has no significant effect on the clinical periodontal parameters over the results achieved by scaling and root planing.
Further studies employing larger sample size with multiple laser applications are warranted to substantiate the role of laser decontamination of periodontal pockets as an adjunct to scaling and root planing in the management of chronic periodontitis.
[1]. Holt SC, Ebersole JL, Porphyromonas gingivalis, treponema denticola, & tannerella forsythia: ‘the red complex’, a prototype polybacterial pathogenic consortium in periodontitisPeriodontol 2000 2005 38:72-122. [Google Scholar]
[2]. Umeda M, Takeuchi Y, Noguchi K, Huang Y, Koshy G, Ishikawa I, Effects of nonsurgical periodontal therapy on the microbiotaPeriodontol 2000 2004 30:98-120. [Google Scholar]
[3]. Newman MG, Takei HH, Klokkevold PR, Carranza FA, Clinical Periodontology 2006 10th edSt. Louis MissouriSaunders Elsevier [Google Scholar]
[4]. Dodwad V, Shubhravaish Aakriti M, Chhokra M, Local drug delivery in periodontics: a strategic interventionInt J Pharm Pharm Sci 2012 4(4):30-34. [Google Scholar]
[5]. Divya PV, Nandakumar K, Local drug delivery protocol in periodonticsTrendsiomater Artif Organs 2006 19:74-80. [Google Scholar]
[6]. Matesanz-Pérez P, García-Gargallo M, Figuero E, Bascones-Martínez A, Sanz M, Herrera D, A systematic review on the effects of local antimicrobials as adjuncts to subgingival debridement, compared with subgingival debridement alone, in the treatment of chronic periodontitisJ Clin Periodontol 2013 40(3):227-41. [Google Scholar]
[7]. Kalsi R, Vandana KL, Prakash S, Effect of local drug delivery in chronic periodontitis patients: A meta-analysisJ Indian Soc Periodontol 2011 15(4):304-09. [Google Scholar]
[8]. Srivastav R, Verma PK, Tandon P, RameshKumar M, Gupta KK, Srivastava A, Chlorhexidine chip and tetracycline fibers as adjunct to scaling and root planing: A clinical studyBraz J Oral Sci 2009 8(4):201-20. [Google Scholar]
[9]. Keshava A, Girish S, Lasers a boon or mith in periodontal treatmentIndian Journals. com 2013 4(4):1-6. [Google Scholar]
[10]. Schwarz F, Aoki A, Becker J, Sculean A, Laser application in non-surgical periodontal therapy: a systematic reviewJ Clin Periodontol 2008 35(8):29-44. [Google Scholar]
[11]. Convissar RA, Principles and practice of laser dentistry 2011 St. Louis, MoMosby Elsevier [Google Scholar]
[12]. Birang R, Yaghini J, Adibrad M, Kiany S, Mohammadi Z, Birang E, The effects of diode laser (980 nm wavelength) and chlorhexidine gel in the treatment of chronic periodontitisJ Laser Med Sci 2011 2(4):131-38. [Google Scholar]
[13]. Noguchi T, Sanaoka A, Fukuda M, Suzuki S, Aoki T, Nd: YAG laser irradiation with local antibiotic application into periodontal pocketsJ Int Acad Periodontol 2005 7(1):8-15. [Google Scholar]
[14]. Loe H, The gingival index, the plaque index and retention index systemJ Periodontol 1967 38(6):610-16. [Google Scholar]
[15]. Convissar RA, Principles and practice of laser dentistry 2010 First editionElsevier publishers [Google Scholar]
[16]. Badersten A, Nilveus R, Egelberg J, Effect of non-surgical periodontal therapy. I. Moderately advanced periodontitisJ Clin Periodontol 1981 8:57-72. [Google Scholar]
[17]. Badersten A, Nilveus R, Egelberg J, Effect of non-surgical periodontal therapy. II. Severely advanced periodontitisJ Clin Periodontol 1984 11:63-76. [Google Scholar]
[18]. Chandra C, Valavalkar N, Vandana KL, The comparative evaluation of xanthan gel with chlorhexidine (Chlosite) in smokers and non-smokers: A clinical and microbiological assessmentJ Indian Soc of Periodontol 2011 15:221-27. [Google Scholar]
[19]. Sachdeva S, Agarwal V, Evaluation of commercially available biodegradable tetracycline fiber therapy in chronic periodontitisJ Indian Soc Periodontol 2011 15:130-34. [Google Scholar]
[20]. Heitz M, Trombelli L, Heitz F, Neeleman I, Moles D, A systemic review of the effect surgical debridement versus non-surgical debridement for the treatment of chronic periodontitis without surgical accessJ Clin Periodontol 2002 29(3):92-102. [Google Scholar]
[21]. Ahmed K, Malvin J, Lynn H, Chang K, Comparison of direct digital and conventional intraoral radiographs in detecting alveolar bone lossJ Am Dent Assoc 2003 11:1468-75. [Google Scholar]
[22]. Kranti K, Seshan H, Zope S, Clinical evaluation of topical subgingival application of biodegradable xanthan based 1.5% Chlorhexidine gel for treatment of periodontal pocketsJ Adv Dental Research 2010 1(1):47-54. [Google Scholar]
[23]. Moritz A, Schoop U, Goharkhay K, Schauer P, Doertbudak O, Wernisch J, Treatment of periodontal pockets with a diode laserLasers Surg Med 1998 22:302-11. [Google Scholar]
[24]. Dukic W, Bago I, Aurer A, Roguljić M, Clinical effectiveness of diode laser therapy as an adjunct to non-surgical periodontal treatment: a randomized clinical studyJ Periodontol 2013 84(8):1111-17. [Google Scholar]
[25]. Kornman KS, Controlled release local delivery antimicrobials in periodontics: prospects for the futureJ Periodontol 1993 64:782-91. [Google Scholar]
[26]. Puri K, Dodwad V, Bhat K, Puri N, Effect of controlled-release Periochip™ on clinical and microbiological parameters in patients of chronic periodontitisJ Indian Soc Periodontol 2013 17(5):605-11. [Google Scholar]
[27]. Kumar AJ, Ramesh Reddy BV, Chava VK, Effect of chlorhexidine chip in the treatment of chronic periodontitisJ Nat Sci Biol Med 2014 5(2):268-72. [Google Scholar]
[28]. Grover V, Kapoor A, Malhotra R, Battu VS, Bhatia A, Sachdeva S, To assess the effectiveness of a chlorhexidine chip in the treatment of chronic periodontitis: A clinical and radiographic studyJ Indian Soc Periodontol 2011 15(2):139-46. [Google Scholar]
[29]. Kondreddy K, Ambalavanan N, Ramakrishna T, Kumar RS, Effectiveness of a controlled release chlorhexidine chip (Periocol CG) as an adjunctive to scaling and root planing when compared to scaling and root planing alone in the treatment of chronic periodontitis. a comparative studyJ Indian Soc Periodontol 2012 16(4):5537 [Google Scholar]