An Unusual Lesser Sac Collection Causing Gastric Outlet Obstruction with Coincidental Occurrence of Leriche’s Syndrome: A Case Report
Anand Singla1, Darshanjeet Singh Walia2, Rishabhpreet Kaur3
1 Junior Resident, Department of General Surgery, Government Medical College, Patiala, Punjab, India.
2 Assistant Professor, Department of Pathology, Government Medical College, Patiala, Punjab, India.
3 Student, Government Medical College, Patiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Anand Singla, F-6, Tej Bagh Colony, Patiala, Punjab-147001, India.
E-mail: anand_singla84@yahoo.co.in
Gastric outlet obstruction in adults is usually caused by pyloric stenosis secondary to peptic ulcer disease or malignancy. However, there are few other causes such as a foreign body and external compression due to pseudocyst pancreas. We present a rare aetiology of a large collection of pus in the lesser sac in our patient causing gastric outlet obstruction. A perforated peptic ulcer was suspected in our patient who had symptoms of sudden onset pain in epigastric region which was referred to back. This was followed by pain in upper abdomen, vomiting, constipation and fever for which patient was being managed conservatively before being referred to us. The CECT didn’t show any leakage of contrast to the lesser sac making the possibility of healed perforation likely as all other causes were ruled out at the time of presentation to our hospital. The CECT scan ruled out other causes of gastric outlet obstruction with normal wall thickness of the stomach and duodenum along with normal looking liver, pancreas and no lymphadenopathy. The liver function tests and serum amylase were within normal limits. Along with this, there was another unrelated rare coincidental finding of aortoiliac occlusive disease termed as Leriche’s syndrome. Ultrasound guided percutaneous drainage was done following which the patient’s obstruction was relieved and patient was referred to the department of vascular surgery for the mangement of aortoiliac occlusive disease.
Aortoiliac syndrome, Collection in omental bursa, Perforated duodenal ulcer
Case Report
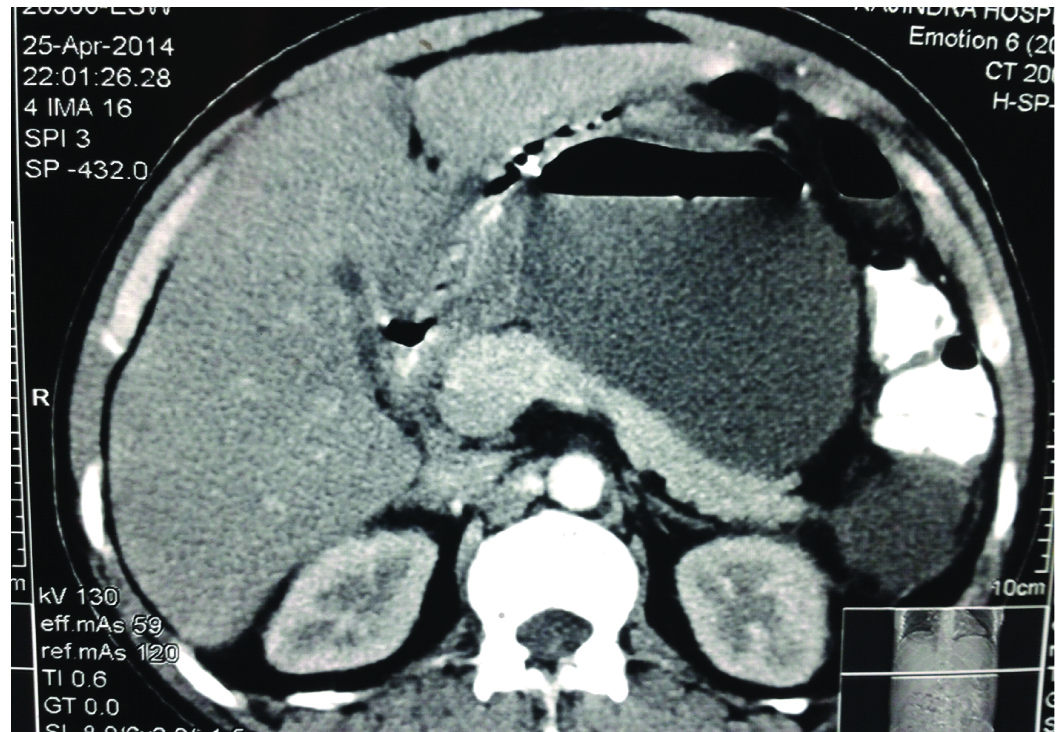
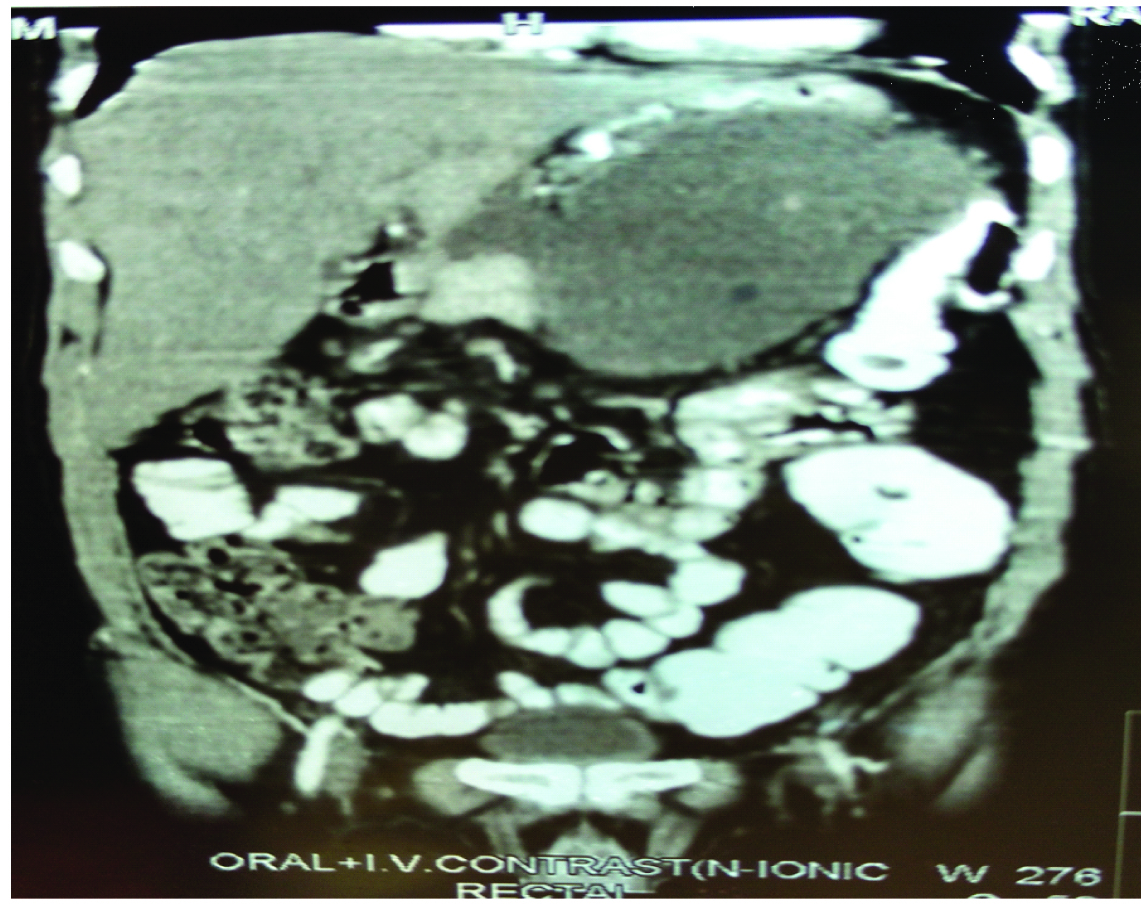
A 45-year-old male, chronic smoker, had complaints of sudden onset severe pain in upper abdomen, vomiting, constipation, fever, loss of weight and pain in gluteal region for which the patient was already receiving treatment (was kept nil per orally with regular nasogastric tube aspiration, PPI’s, antibiotics, analgesics and intravenous fluids) but was referred to our institution as the patient’s condition did not improve. On examination a mass was palpable in epigastric region and rest of the examination was unremarkable. His liver function tests and level of pancreatic enzymes were normal. USG showed a large collection 8cm x 8cm in epigastric region. On CECT Scan a large cystic multi-loculated collection was seen in lesser sac measuring 13.5cm x 10.9cm x 10.7cm. However, liver and pancreas were reported to be normal along with normal wall thickness of stomach and duodenum. This collection was indenting and compressing the body of stomach, causing significant luminal narrowing [Table/Fig-1,2]. Major drainage vessels were normally opacified in proximal abdominal aorta before the level of renal arteries beyond which calcified atheromatous plaque was seen upto the bifurcation into common iliac vessels. For the collection present in lesser sac ultrasound guided percutaneous drainage was done and a drainage tube was left in situ and about 2 litres of pus drained, which came out to be sterile on culture sensitivity. Following this, the patient’s condition improved and repeated USG abdomen showed that the collection reduced to 4.2cm x 4cm and then disappeared in a week and no focal lesion of the pancreas was seen.
CT Scan section showing lesser sac collection compressing the stomach which appears slit like causing Gastric outlet obstruction with normal looking liver and pancreas.
Coronal view showing lesser sac collection compressing the stomach which appears slit like causing Gastric outlet obstruction with normal looking liver and pancreas.
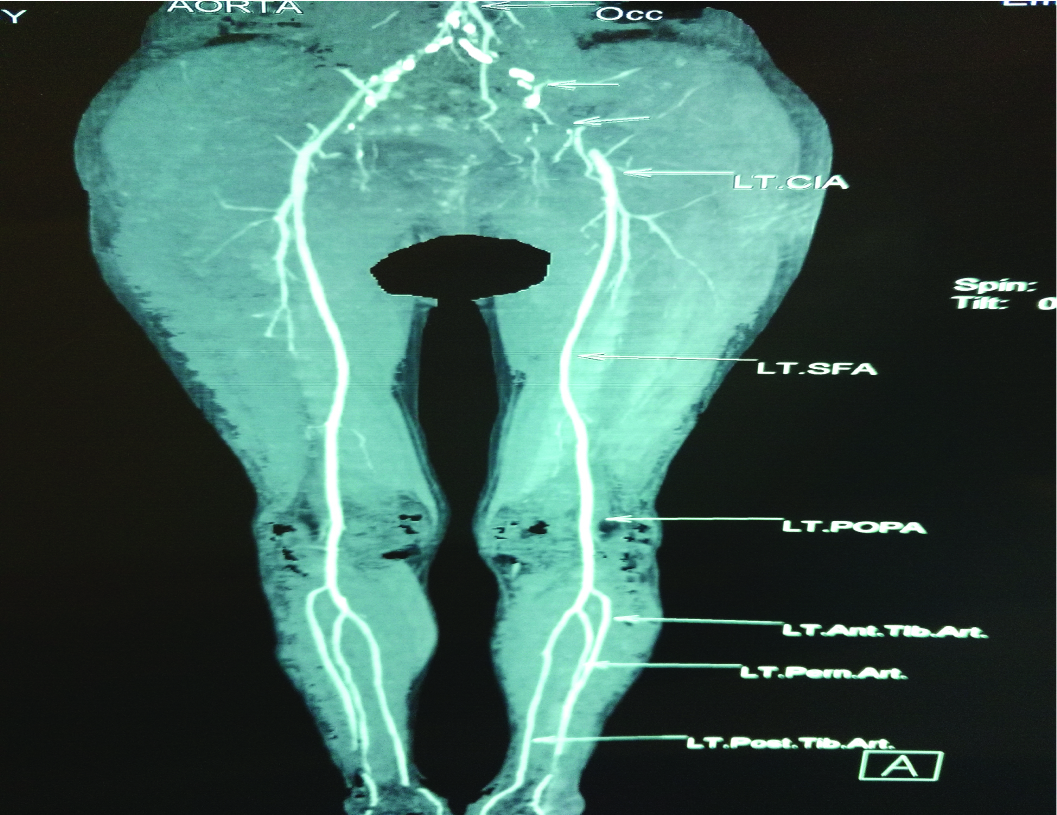
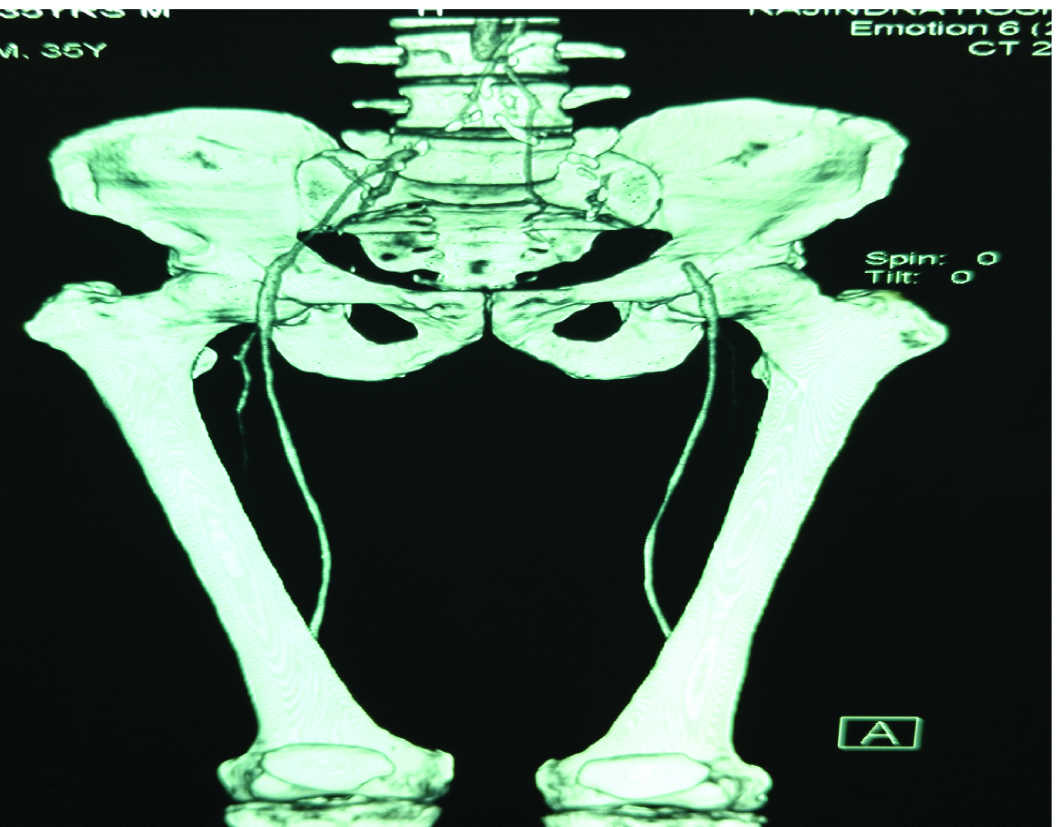
On further detailed history and examination patient gave the history of pain in gluteal region which increased on walking and relieved at rest. History of erectile dysfunction was also present. Examination showed feeble peripheral pulses in both the lower limbs. His fasting lipid profile showed increased triglycerides. CT angiography of the lower limb showed abdominal aorta below the level of renal arteries having calcified atheromatous plaques, causing marked luminal narrowing and complete occlusion of lumen just proximal to its bifurcation. Bilateral proximal common iliacs and left internal iliac were almost completely obliterated by atheromatous plaques [Table/Fig-3,4]. Distal common iliac artery and internal iliac artery on right side were normally opacified. In view of this aortoiliac occlusive disease, patient was referred to the department of vascular surgery for bilateral aortofemoral bypass surgery.
CT Angiography section showing abdominal aorta below the level of renal arteries having marked luminal narrowing and complete occlusion of lumen just proximal to its bifurcation.
CT Angiography section showing complete obliteration of bilateral proximal common iliacs and left internal iliac.
Discussion
Mechanical obstruction to gastric emptying due to any underlying disease process leads to Gastric Outlet Obstruction (GOO) [1]. The most common symptoms are abdominal pain, nausea, and post-prandial non bilious vomiting. The pattern and the rate of symptom onset, on the other hand, may depend on the underlying pathology. The basic mechanism of GOO is an obstruction of pyloric canal or proximal duodenum by intrinsic or extrinsic (compression) factors. GOO is caused by upper gastrointestinal malignancies as well as peptic ulcers, gastric polyps, caustic material ingestion, pyloric stenosis, duodenal web, gallstone obstruction (Bouveret’s syndrome), gastric tube complications, pancreatic pseudocysts, and various bezoars which constitute the benign aetiology [1]. In addition to these classical factors, there are also rare causes including the presence of a Riedel’s lobe, exophytic giant haemangioma of the liver, worm ball, amoebic liver abscesses originating from liver, massive biloma, cystic lymphangioma of the lesser sac [2–7]. Liver tumours, haemorrhage, necrosis, and infarction are very rare. The conditions requiring emergency surgical intervention like, spontaneous rupture or intraperitoneal bleeding are extremely rare [1,8]. In our patient a large lesser sac collection of pus led to gastric outlet obstruction which is a rare cause. There was history of sudden onset severe epigastric pain which was referred to the back. Serum amylase level was normal and pancreas was reported to be normal on CECT scan. Therefore the cause of this collection was presumed to be a perforated peptic ulcer which had healed at the time of CECT examination as patient was referred to us after being managed conservatively for a week. The other possibility considered was an attack of pancreatitis which had subsided but left an infected peripancreatic collection in the lesser sac. All the other causes that could have caused this collection were ruled out [Table/Fig-1,2].
Leriche’s syndrome includes erectile dysfunction, weakness in the lower limbs, ischemic pain due to claudication, absent or diminished femoral pulses, pallor and coldness of both the feet and legs [9]. Our patient had pain in both lower limbs more so in gluteal region which increased on walking along with failure to have penile erection. CT Angiography showed abdominal aorta below the level of renal arteries having marked luminal narrowing and complete occlusion of lumen just proximal to its bifurcation [Table/Fig-3,4].
Pulses are notably absent below the involved segment of the vessel with absence of capillary refill [10]. Abundant collateralization between abdominal, pelvic and infra-inguinal arteries, makes critical limb ischemia a rare event. In our patient all the peripheral pulses were feeble due to the formation of collateral circulation. A more common presentation is of claudication of varying severity and levels as was found in our patient.
Conclusion
In cases of GOO, rare causes should always be considered. Ultrasound or Computed Tomography guided percutaneous drainage along with suitable antibiotics is the mainstay of treatment of intraabdominal abscesses, except in multiple abscess and abscess in vicinity to vital structures where an exploratory laparotomy may be necessary. Although, presence of two rare conditions in the same patient was a more rare coincidence.
[1]. Eris C, Yildiz MK, Odabasi M, Akbulut S, Abuoglu H, Ozkana E, Gastric outlet obstruction caused by focal nodular hyperplasia of the liver: A case report and literature reviewInt J Surg Case Rep 2013 4(8):681-83. [Google Scholar]
[2]. Guner A, Kahraman I, Aktas A, Kece C, Reis E, Gastric outlet obstruction due to duodenal bezoar: a case reportInternational Journal of Surgery Case Reports 2012 3:523-25. [Google Scholar]
[3]. Akbulut S, Cakabay B, Sevinc MM, Basak F, Gastric outlet obstruction caused by Riedel’s lobe of the liver: a diagnostic and therapeutic challenge for surgeonsHepato-Gastroenterology 2011 58:589-92. [Google Scholar]
[4]. Aydin C, Akbulut S, Kutluturk K, Kahraman A, Kayaalp C, Yilmaz S, Giant hepatic hemangioma presenting as gastric outlet obstructionInternational Surgery 2013 98:19-23. [Google Scholar]
[5]. Pujahari AK, Singh KV, An unusual cause of gastric outlet obstruction: a case reportTropical Gastroenterology 2003 24:79-80. [Google Scholar]
[6]. Gorospe EC, Leggett CL, Nadkarni NA, Massive biloma presenting as gastric outlet obstructionAnnals of Gastroenerology 2012 25(2) [Google Scholar]
[7]. Kumar SS, Das SP, Kate V, Cystic lymphangioma of the lesser sac in adult presenting with features of gastric outlet obstruction – A case reportJCDR 2015 9(11):PD15-PD16. [Google Scholar]
[8]. Aydin C, Akbulut S, Kutluturk K, Kahraman A, Kayaalp C, Yilmaz S, Giant hepatic hemangioma presenting as gastric outlet obstructionInternational Surgery 2013 98:19-22. [Google Scholar]
[9]. Nandeesh BN, Mahadevan A, Tandon A, Satishchandra P, Shankar SK, Aortoiliac occlusive disease masquerading as cerebrovascular accidentAnnals of Indian Academy of Neurology 2007 10(3):178-81. [Google Scholar]
[10]. Tintinall JE, Kelen GD, Stapczynski JS, Emergency medicine 2004 6th edMcGraw HillNew York:415-18. [Google Scholar]