Primary Inverted Papilloma of Middle Ear and Mastoid: A Rare Case Report
Jyotiman Nath1, Bibhuti Das2
1 Post Graduate Trainee, Department of Radiotherapy, Assam Medical College and Hospital, Dibrugarh, India.
2 Post Graduate Trainee, Department of ENT and Head and Neck Surgery, Assam Medical College and Hospital, Dibrugarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jyotiman Nath, Post Graduate Trainee, Department of Radiotherapy, Assam Medical College, Dibrugarh, Assam-786002, India.
E-mail: jyotimannath@gmail.com
Inverted papilloma or Schneiderian papilloma arising primarily from middle ear and mastoid is a very rare entity. It is a benign and locally aggressive condition, with increased risk of recurrence and malignant transformation. Surgery is the primary treatment. Radiation therapy should be considered in case of malignant transformation, recurrent or inoperable disease. Here we are reporting a case of recurrent inverted papilloma with dysplastic changes arising from mastoid cavity in a 60-year-old male. The patient was treated with surgery followed by radiotherapy.
Computed Tomography (CT), Inverted Papilloma (IP), Magnetic resonance imaging (MRI), Radiotherapy (RT)
Case Report
A 60-year-old male presented to the ENT OPD of Assam Medical College Dibrugarh, with purulent foul smelling discharge and severe pain in the right ear associated with marked hearing loss. There was no history of tinnitus and vertigo. The patient gives history of similar symptoms of pain and purulent discharge from the right ear for which he underwent ear surgery twice about 40 years back, but no documentation regarding the procedure was available with the patient.
On otoscopic examination central perforation of right tympanic membrane was noted while left tympanic membrane was intact. Pure tone audiometry showed hearing loss of 60 decibel. On nasal examination there was no evidence of nasal papilloma. CT scan showed right sided chronic supporative otitis media of attico-antral type.
Based on his chief complaints, the patient was considered for radical mastoidectomy. But immediately after 2 months of surgery, he again presented with similar symptoms of severe pain and purulent fowl smelling discharge from the right ear along with gaping in the right post auricular wound with exposed mastoid cavity filled with purulent discharge.
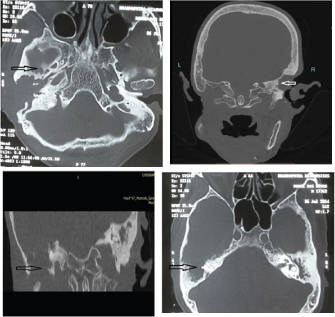
Repeat CT scan showed postoperative bony defect in right petromastoid region with extensive soft tissue lesion with erosive bone changes on right side [Table/Fig-1a-d].
HRCT scan (axial and coronal section) of petrous temporal bone showed postoperative bony defect in right petromastoid bone with irregular soft tissue lesion causing destruction of right scutum, ossicular chain, tegmen tympani, lateral mastoid cortex, TM joint fossa with intact semicircular canel and inner ear structures and left middle ear shows collection without bony destruction.
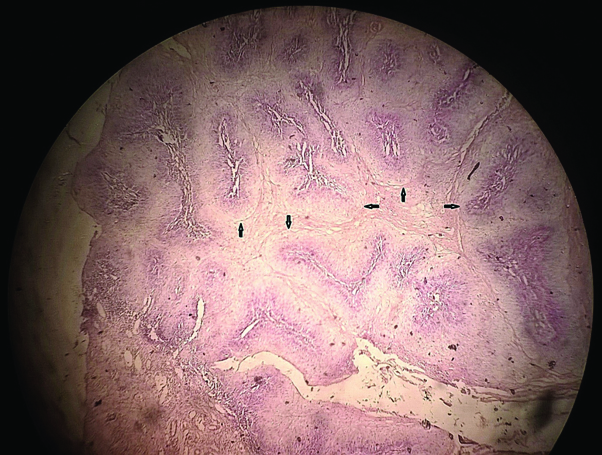
The patient was again planned for mastoid exploration. Extensive granulation tissues were removed following mastoidectomy. The histopathological examination of the tissue removed revealed picture of inverted papilloma with marked dysplasia [Table/Fig-2]. Immunohistochemistry was done to tag mitosis by proliferative marker Ki67 [16/10 HPF] showed moderate degree of proliferative activity.
Microscopic view showing Schneiderian papilloma (inverted papilloma) showing bulbous downward (inverted) growth of squamous epithelial cell proliferation into underlying stroma with dysplastic changes.
The patient was then treated with postoperative external beam radiation in a cobalt-60 teletherapy machine (Theratron 780 C). A total dose of 54 Gy was delivered in 30 daily fractions of 180 cGy with anterior and posterior oblique wedge fields. After the completion of the course of radiotherapy, there was no pain and discharge from the right ear.
Patient was followed up at one month and then every three month. MRI of the temporomastoid region was done in each follow-up using Siemens Avanto 1.5 Tesla machine.
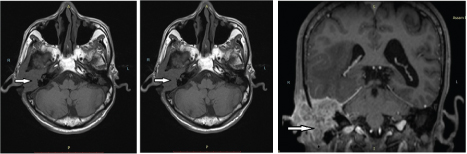
There were no symptoms of pain and ear discharge at the end of one month except having mixed hearing loss. No signs of recurrence were observed till 9 month follow-up. But at 11 month after treatment, the patient again presented with similar symptoms of pain and discharge from the right ear and MRI showed evidence of recurrence of the disease with intracranial invasion [Table/Fig-3a-c].
Axial and coronal section of MR imaging at 11th month after treatment shows recurrence of the tumor. There is evidence of ill defined heterogeneous T1iso and T2 FS hyperintense mass centred on right petromastoid region causing destruction of right floor of the mastoid, tympanic cavity and mendibular fossa inferiorly; and extending superiorly causing destruction of middle cranial cavity with intracranial extension to right imferiortemporal lobe.
Discussion
Inverted Papilloma or Schneiderian papillomas generally arise in the paranasal sinuses, while middle ear and the mastoid cavity as primary site is an extremely rare entity. Less than 20 cases of inverted papilloma arising primarily from middle ear and mastoid cavity have been published in the literature so far [1,2].
The lining epithelium of nasal cavity and paranasal sinus is ciliated columnar which is also known as Schneiderian epithelium. Hence papillomas arising from these sites are called Schneiderian papilloma. Histologically three types of papillomas have been identified; exophytic papilloma, oncocytic papilloma and Inverted Papilloma (IP); out of which IP is the commonest (62%) and can be lined by squamous, transitional or respiratory epithelium. But IP originating primarily from the mastoid and middle ear is extremely rare [1].
Rubin et al in their report in 2012 mentioned about 17 cases of IP of middle ear and mastoid with mean age of presentation at 53 years. Out of these 17 patients, 35.3% of patients had malignant transformation which is higher than that observed in IP of paranasal sinus and 56.25% of patients had recurrence of the disease [1].
Including the case reported by Andrés Coca-Pelaz et al., in December 2015, total 19 cases of inverted papilloma arising primarily from middle ear and mastoid are published till now. The mean age of presentation of all these 19 cases of primary IP was 48 years (range 19-74 years). Out of these 19 patients; 8 were male and 11 were female [2].
Although the pathogenesis of the IP of mastoid and middle ear is not clearly understood; two hypotheses have been described. One is direct extension from sinunasal tract and the other is abnormal migration of embryonic Schneiderian membrane to the middle ear [3]. These lesions are locally aggressive and have a strong tendency to recur and transform into squamous cell carcinoma [4].
Vorasubin N et al., conducted a retrospective review of 70 patients of sinonasal papilloma who underwent surgery. Out of 70 cases, 37 inverted papillomas were identified. Out of these 37 inverted sinonasal papillomas 8% (n=3) had transformation to squamous cell carcinoma and 8% (n=3) had dysplastic changes [5].
Another study by Barens L states that the associated malignancy; most often of squamous cell histology may arise from IP or may appear concomitantly from IP in 11% of cases [6].
Surgical resection is the primary treatment for this condition. Postoperative radiation therapy should be considered in case of malignant histology and incomplete resection. Radiation therapy can also be considered in cases of recurrent and inoperable disease [7].
Because of the higher tendency of recurrence and malignant transformation, the patients of inverted papilloma should be considered for long term follow-up. Besides clinical examination, MRI should be performed during the follow-up [8]. MRI is preferred because of its sensitivity and specificity for differentiating soft tissue mass from postoperative changes and inflammation [2].
[Table/Fig-4] shows few of the cases of primary inverted papilloma of middle ear and mastoid published in the literature [2,4,8–11].
M- Male, F- Female, MA- Mastoid, ME- Middle EAR, EAC- External Auditory Canal, RT- Radiotherapy
| Sl. no. | Author name (year) [reference no.] | Age (Years), sex | Findings(involving sites) | TransformationYes/no | Treatment provided |
|---|
| 1 | de Filippis et al., 2002 [8] | 58,M | MA, ME | No | Surgery |
| 2 | Shen et al., 2011 [10] | 56, M | ME, EAC | Yes | Surgery plus RT |
| 3 | Kainuma et al., 2010 [11] | 65, M | MA,ME, EAC | No | Surgery plus RT |
| 4 | O’Cornell B et al.,2010 [4] | 52, M | ME | - | Surgery |
| 5 | Rubin et al., 2012 [1] -17th case | 73,M | MA, ME | No | Surgery |
| 6 | Lisa Van der putten et al., 2013 [9]-18th Case | 74, F | MA, ME | No | Surgery |
| 7 | Andrés Coca-Pelaz, 2015 [2]- 19th Case | 74, M | ME | No | Surgery |
| 8 | Present case | 60, M | MA, ME | Yes | Surgery plus RT |
Conclusion
Inverted papilloma (Schneiderian papilloma) originating primarily from the mastoid and middle ear is very rare. Recurrence rates and association with malignancy are higher in IP of the middle ear and mastoid than that of the nose and paranasal sinuses. Surgery is the primary treatment. Radiation therapy has role in cases of multiple recurrence, incomplete resection and malignant transformation. Long term follow-up after treatment is mandatory.
[1]. Rubin F, Badoual C, Moya-Plana A, Malinvaud D, Laccourreye O, Bonfils P, Inverted papilloma of the middle earEuropean Annals of Otorhinolaryngology, Head and Neck Diseases 2012 129(4):207-10. [Google Scholar]
[2]. Coca-Pelaz A, Gómez-Martínez J, Vivanco-Allende B, Hermsen M, Llorente J, Primary inverted papilloma of the middle ear with intracranial invasionHead Neck 2015 doi: 10.1002/hed.24329 [Google Scholar]
[3]. Wenig BM, Schneiderian-type mucosal papillomas of the middle ear and mastoidAnn Otol Rhinol Laryngol 1996 105:226-33. [Google Scholar]
[4]. O’Connell B, Rivas A, Wanna G, Haynes D, Inverting Papilloma of the Middle Ear: A Case ReportThe Laryngoscope 2010 120(S3):S85-S85. [Google Scholar]
[5]. Vorasubin N, Vira D, Suh JD, Bhuta S, Wang MB, Schneiderian papillomas: Comparative review of exophytic, oncocytic, and inverted TypesAm J Rhinol Allergy 2013 27(4):287-92. [Google Scholar]
[6]. Barnes L, Diseases of the nasal cavity, paranasal sinuses and nasopharynx. In: Barnes L, editorSurgical pathology of the head and neck 2009 New YorkInforma Healthcare:343-422. [Google Scholar]
[7]. Strojan P, Ferlito A, Lund VJ, Kennedy DW, Silver CE, Rinaldo A, Sinonasal inverted papilloma associated with malignancy: the role of human papillomavirus infection and its implications for radiotherapyOral Oncol 2012 48:216-18. [Google Scholar]
[8]. De Filippis C, Marioni G, Tregnaghi A, Marino F, Gaio E, Staffieri A, Primary Inverted Papilloma of the Middle Ear and MastoidOtology & Neurotology 2002 23(4):555-59. [Google Scholar]
[9]. Van der Putten L, Bloemena E, Merkus P, Hensen E, Schneiderian papilloma of the temporal boneCase Reports 2013 2013(dec05 1):bcr2013201219-bcr2013201219. [Google Scholar]
[10]. Shen J, Baik F, Mafee M, Peterson M, Nguyen Q, Inverting Papilloma of the Temporal BoneOtology & Neurotology 2011 32(7):1124-33. [Google Scholar]
[11]. Kainuma K, Kitoh R, Kenji S, Usami S, Inverted papilloma of the middle ear: A case report and review of the literatureActa Otolaryngol 2011 131(2):216-20. [Google Scholar]