A Rare Case of Mayer-Rokitansky-Kuster-Hauser Syndrome Presenting with Acute Psychosis
Kamal Nath1, Bhanita Boro2, Subrata Naskar3
1 Associate Professor, Department of Psychiatry, Silchar Medical College and Hospital, Silchar, Assam, India.
2 Postgraduate Trainee, Department of Psychiatry, Silchar Medical College and Hospital, Silchar, Assam, India.
3 Postgraduate Trainee, Department of Psychiatry, Silchar Medical College and Hospital, Silchar, Assam, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subrata Naskar, Postgraduate Trainee, Department of Psychiatry, Silchar Medical College & Hospital, Silchar, Assam-788014, India.
E-mail: nsubrata09@gmail.com
The psychiatric co-morbidities in female population with mullerian agenesis is an area with limited research. This is probably due to the fact that when those patients are diagnosed not much attention or information is given for long term psychiatric follow-up. Owing to their inability to bear children, these subjects often become socially harassed. Thus these constant stressors may lead to development of psychopathology in future. Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome is a congenital abnormality with absence of uterus, cervix and vagina, but normal secondary sexual characteristics and external genitalia and occurs in every 1 out of 4000-10,000 females. There is also limited literature on the probable common chromosomal aetiology for both psychosis and MRKH patients. We, present here a case of MRKH syndrome, whose initial presentation was psychosis only. In this respect, we also highlight the much neglected need of appropriate psychiatric screening and provision of psychiatric care in this population.
Congenital anomaly, Mullerian agenesis, Primary amenorrhea, Psychosis NOS, Psychological distress
Case Report
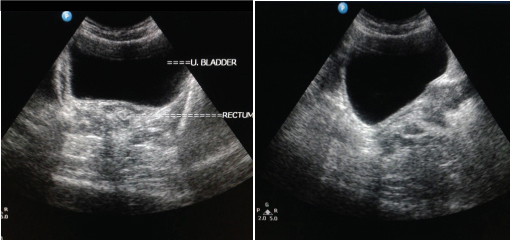
A 22-year-old female patient presented at emergency of a tertiary care hospital with complains of crying spells, irrelevant talk at times, fearfulness, withdrawn behaviour, hearing of voices not heard by others since last one month. Being from a rather lower socioeconomic strata, where the alternative form of treatment for psychiatric disorder is more accessible and believed in, she was taken to a local faith healer. However, her symptoms didn’t improve upon receiving the treatment. She was then taken to a private psychiatrist, who provisionally diagnosed her as a case of unspecified non organic psychosis. She was put on Tab Olanzapine 10 mg with Tab Divalproex sodium 500 mg once a day. Her symptoms gradually improved. Three weeks later, her relatives upon seeing her relatively stable condition abruptly stopped the medications. Five to six days passed without any significant complaints, but soon after that she developed florid symptoms, similar to prior treatment. She was brought to the tertiary care center and admitted to the female psychiatry ward. Mental state examination revealed a thinly build women whose hygiene was maintained with support. She was extremely uncooperative, psychomotor activity was retarded with unprovoked irritation at times. Her affect was shallow, inappropriate with restricted range. Initially, her thought content could not be assessed but there was prominent hallucinatory behaviour in the form of gesturing and muttering. She was conscious, comprehensive, attention could be drawn but concentration maintained with difficulty. Her memory and orientation was intact, however, her abstract thinking was impaired along with judgement and reasoning and her insight was of grade 1. On application of Brief Psychiatric Rating Scale (BPRS) and Hamilton Depression Rating Scale (HAM-D) the score was 35 & 16 respectively. After the initial workup, a provisional diagnosis of unspecified non organic psychosis (F29) according to The ICD-10 Classification of Mental and Behavioural Disorders was made and she was again started on Tab Divalproex Sodium 500mg with Tab Olanzapine increased to 15mg, both at bedtime. On further evaluation, her informants revealed that patient was having primary amenorrhea but she had normal secondary sexual characteristics. A gynecology consultation was sought for, after an ultrasonography of whole abdomen. They reported a normal external genitalia but USG report confirmed the absence of uterine structure between the bladder and rectum [Table/Fig-1]. A provisional diagnosis of Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome was made. Patient was continued on the above mentioned medications and her symptoms gradually improved, she became emotionally stable with improvement in mood, food intake and hygiene. BPRS and HAM-D score at time of discharge was 19 & 8 respectively.
USG report showing the absence of uterine structure between the bladder and rectum.
Discussion
Relation between stress and psychological disturbances are well established facts. In addition to various psychosocial stressors physical deformity in the adolescent group acts as a serious stressor particularly in the female group. Many a times a specific type of physical abnormality or deficiency may have chromosomal or neurodevelopmental aetiology which itself may play as a common aetiological factor for the psychological disorder as well as the physical deformity. Therefore keeping in mind this possible dual association of a major physical/anatomical abnormality and psychological disorder in young adolescent girl, the above case has been presented here after taking valid consent from the family members of the patient.
Mayer –Rokitansky-Kuster- Hauser Syndrome (MRKH) is a congenital abnormality characterized by the absence of vagina, cervix and the uterus [1]. The reproductive abnormalities of MRKH syndrome are due to incomplete development of the mullerian duct. Mullerian agenesis occurs in every 1 out of 4000-10,000 females [2]. The diagnosis of the syndrome is usually made at puberty. Patients usually present with primary amenorrhea in adolescence with normal physical growth and development. This diagnosis of mullerian agenesis has been an incidental finding in our patient who actually presented with florid psychotic symptoms. By reporting the case we want to throw light over a neglected area of much required psychological support and treatment in females with this kind of anatomical abnormality of reproductive system which manifests with amenorrhea and infertility and in the long run undergoes through major stresses. Very few cases have been reported so far which may be due to rarity of such patients or may reflect the incomplete evaluation of the patient from a psychiatric point of view. Only very few literatures report about females with MRKH Syndrome and their affecting psychological profile resulting from mental trauma and stress.
Jacoline G et al., conducted a study on 66 women with MRKH compared with 33 controls and concluded that “MRKH has a lasting negative impact on affected women’s level of psychological distress and self-esteem” [3]. A number of genetic research has been conducted to find the common genetic link between MRKH and psychiatric illnesses. On one hand, one such study showed that deletion of 17q12 is a recurrent, pathogenic copy number variant that carries significant risk of schizophrenia, whereas on the other study by Hinkes B et al., and Ledig S et al., showed that 17q12 complex micro deletion is associated with MRKH syndrome [4,5]. These studies provided the much needed genetic link between MRKH syndrome and the possible psychiatric illnesses associated with it. A case study by Gupta et al., concluded that “the MRKH syndrome greatly affects the psychological profile of the female resulting in mental trauma and stress [6]. Psychological counselling is the primary treatment modality which can ameliorate the stress associated with the condition.” Another case study by Bhad et al., reported a possible link between schizophrenia and MRKH syndrome in a 24-year-old unmarried Indian female [7].
Conclusion
Hence, with this case report we want to urge to the scientific community to look for the associated psychiatric illnesses that may accompany this syndrome and alongside offer advice on the non-surgical methods for treatment of vaginal agenesis such as Frank’s or Ingrams’s dilator method [8]. For long term management, psychoeducation of the patient and the family and supportive psychotherapy are very much important and appropriate steps.
[1]. Guerrier D, Mouchel T, Pasquier L, Pellerin I, The Mayer-Rokitansky-Küster-Hauser syndrome (congenital absence of uterus and vagina)–phenotypic manifestations and genetic approachesJ Negat Results Biomed [Internet] 2006 5:1[cited 2015 Dec 15]. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1368996&tool=pmcentrez&rendertype=abstract [Google Scholar]
[2]. Hillard PJA, The 5-minute Obstetrics and Gynecology Consult [Internet]. Hillard PJA, editor 2008 Lippincott Williams & Wilkins[cited 2015 Dec 15]. pp. 667. Available from: https://books.google.com/books?id=fOoFIQOdIhkC&pgis=1 [Google Scholar]
[3]. Heller-Boersma JG, Schmidt U, Edmonds DK, Psychological Distress in Women With Uterovaginal Agenesis (Mayer-Rokitansky-Kuster-Hauser Syndrome, MRKH)Psychosomatics [Internet] 2009 50(3)[cited 2015 Dec 15]. Available from: https://kclpure.kcl.ac.uk/portal/en/publications/psychological-distress-in-women-with-uterovaginal-agenesis-mayerrokitanskykusterhauser-syndrome-mrkh(06e96a4a-e7d1-486e-be1b-ab1a184ad311).html [Google Scholar]
[4]. Hinkes B, Hilgers KF, Bolz HJ, Goppelt-Struebe M, Amann K, Nagl S, A complex microdelaetion 17q12 phenotype in a patient with recurrent de novo membranous nephropathyBMC Nephrol. [Internet] 2012 13:27Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3412739/pdf/1471-2369-13-27.pdf [Google Scholar]
[5]. Ledig S, Schippert C, Strick R, Beckmann MW, Oppelt PG, Wieacker P, Recurrent aberrations identified by array-CGH in patients with Mayer-Rokitansky-Küster-Hauser syndromeFertil Steril [Internet] 2011 95(5)Elsevier Ltd:1589-94.Available from: http://www.ncbi.nlm.nih.gov/pubmed/20797712 [Google Scholar]
[6]. Gupta M, Kharb V, Rokitansky-küster-hauser TM-. Case Report MRKH Syndrome: Psychological Disturbances and Suicide Introduction: Corresponding Author: Treatment: Conclusion: Discussion: 2012;34;1;971-73 [Google Scholar]
[7]. Bhad R, Chadda R, Kumar N, Goyal P, A rare association of schizophrenia and Mayer-Rokitansky-Küster-Hauser syndromeIndian J Psychiatry [Internet] 2015 57(3)Medknow Publications and Media Pvt. Ltd:324-25.[cited 2015 Dec 15] Available from: http://www.indianjpsychiatry.org/article.asp?issn=0019-5545;year=2015;volume=57;issue=3;spage=324;epage=325;aulast=Bhad [Google Scholar]
[8]. Lee MH, Non-surgical treatment of vaginal agenesis using a simplified version of Ingram’s methodYonsei Med J 2006 47(6):892-95. [Google Scholar]