Background
Varicocele is defined as dilated and twisted veins of the pampiniform plexus in the spermatic cord. It is the most common cause of male infertility. There are various medical and surgical procedures for the treatment of this disease.
Aim
This study was aimed to compare the effects of oral administration of L-Carnitine and varicocelectomy on spermogram parameters.
Materials and Methods
This study was conducted as a double blind clinical trial without randomization. Inclusion criteria were, all married infertile men with varicocele. Patients chose their treatment personally and spermogram was carried out for all patients before and after the third and sixth months of treatment. Then, the sperm parameters of the two groups were compared using repeated measures ANOVA.
Results
In our study, trend of sperm count in the surgery group changed from 22 to 28.61 million (vs 34.6 to 45.37 in L-Carnitine group), motility changed from 21.74 to 35.38 percent (vs 33.9 to 47.48 in L-Carnitine group), normal sperm morphology changed from 46.25 to 60 percent (vs 56.61 to 69.7 in L-Carnitine group) and volume of semen changed from 3.5 to 4.17 cc (vs 2.95 to 4.33 in L-Carnitine group). These values were not statistically different between the two groups.
Conclusion
Based on the results of this study, we can say that medicinal treatment by administration of oral L-Carnitine is as effective as varicocelectomy in improving semen parameters and can be used as an alternative to surgery for varicocele grade II.
Infertility, Medical therapy, Surgical therapy
Introduction
Varicocele is defined as dilated and twisted veins of the pampiniform plexus in the spermatic cord [1,2]. It is the most common cause of male infertility and is observed in almost 15% of the general population, in 35% to 40% of men with primary infertility, and about 2/3 of men with secondary infertility [2–5].
Evidence shows that varicocele decreases the quality of semen and fertility in men [6,7]. Reduced sperm motility is the most common disorder observed in the spermogram of patients with varicocele. Varicocele causes a progressive decrease in the activity of testis and eventually leads to testicular atrophy, so that azoospermia or severe oligospermia is observed in 4.3% to 13.3% of patients [8].
Various medical and surgical procedures are used for the treatment of this disease many studies have reported the effectiveness of varicocelectomy in semen analysis and subsequent partial recovery of infertile men with varicocele, so that following the above procedure, significant improvements were observed in semen quality in most people with severe oligospermia [9–13]. There are still some debates about the need for surgery in low grades of varicocele [10,14,15]. There are few alternative therapeutic methods such as medical therapy [16–18]; however, to achieve a successful therapeutic strategy is still difficult.
L-Carnitine may cause its effect through improving the condition in the luminal environment of the epididymis. It is necessary for beta oxidation of fatty acids in mitochondria and helps to continue the energy supply through the transfer of fatty acids from cytosol to mitochondria [19]. However, there are still many debates on the effects of L-Carnitine and its possible mechanism [20]. In addition, L-Carnitine can imitate the effects of glucocorticoid that also suppresses the macrophages in the semen [21]. L-Carnitine is a derivative of lysine and methionine amino acid [19]. Free L-Carnitine is required for beta oxidation of long chain fatty acids in mitochondria. It also protects DNA and cell membranes from the damage caused by free O2 radicals [19].
The highest concentrations of L-Carnitine is found in the human epididymis with the highest concentration of 2,000 times more than what is found in the blood serum [22,23]. Some studies have proved the effectiveness of oral administration of L-Carnitine for men who have a variety of sperm disorders [24,25]. Besides, several other studies have also shown decreased L-Carnitine levels in the seminal fluid of infertile men [22,23,26].
Other studies found that, in patients treated with a daily dose of 2-3g of oral carnitine, sperm motility and count improved [19,26]. However, previous studies have reported L-Carnitine effect on sperm motility and sperm count differently [22,23,26]. Results of a meta-analysis conducted by Zhou in 2007 to compare L-Carnitine with a placebo showed positive effect of carnitine in male fertility [24]. But, to our knowledge no study was conducted to compare the effects of surgical treatment and oral administration of L-Carnitine on men’s fertility.
Aim
The study was conducted with the aim to compare the effect of L-Carnitine and surgical procedure on sperm parameters.
Materials and Methods
This was a quasi experimental trial study (without randomization) approved by the ethics committee of Kurdistan University of Medical Sciences and conducted in 2015 from April to September. Participants were all infertile men with varicocele who were referred to the Urology Clinic of Tohid hospital in Sanandaj, Iran. Although based on possible differences in post treatment motility of 3.8% (± 3.8), type I error of 5%, and study power of 90% the sample size was calculated as 22 patients in each group, but we conducted our study on 35 patients in each group.
Inclusion criteria was infertile married men with varicocele grade II and higher. Exclusion criteria were testicular atrophy, hormone imbalance (including gonadotropin, testosterone, and prolactin), ejaculation disorders and anatomical abnormalities of the urinary tract including hypospadias, stenosis, urinary tract infection, azoospermia and medication during the previous three months. After explaining the objectives of the study to the patients they signed the informed consent. When patients were informed about surgical or medicinal method they chose their desired method of treatment. Three patients with testicular atrophy and five other patients with hormonal imbalance were excluded from the study. Finally 31 patients in each group were studied.
Varicocele is graded at the time of the initial physical examination according to the Dublin grading system [27] as grade I (Palpable only with Valsalva; invisible), grade II (Palpable even without Valsalva, but still invisible) and grade III (Easily visible through scrotal skin) [28].
The patients in each group underwent a spermogram test by a laboratory expert who was not aware of the grouping. Patients were informed not to have sexual intercourse in the previous 48 - 72 hours. Then, patients in the surgery group underwent inguinal surgery and medicinal group were started on an oral dose of 250 mg L-carnitine four times a day for six months. Then three and six months after surgery and medication, another spermogram was conducted with the same method. Sperm count, motility and concentration were assessed post treatment.
Statistical Analysis
The data were analysed with Statistical Package for the Social Science (SPSS Inc, Chicago, Illinois, USA) version 16.0. We used independent t-test to compare independent quantitative variables (sperm count, sperm motility, sperm volume, pH, RBC and WBC) in both groups. Fisher-exact test was used to compare smoking and grading in both groups. Also, spearman coefficient was used to evaluate correlation between duration of infertility and sperm parameters. At last, sperm parameters in both groups were compared using repeated measures. The p-value less than 0.05 was considered as significant.
Results
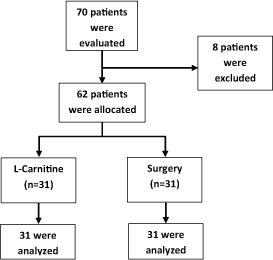
We studied 70 infertile patients with varicocele referring to the clinic. Three patients with testicular atrophy and five other patients with hormonal imbalance were excluded from the study. Then we conducted the study on the remaining 62 patients who were diagnosed with varicocele [Table/Fig-1].
Flow chart of study participants.
Patients were 19 to 41 years with a mean age of 29.06 years. Demographical questionnaire showed that 28 patients (45.2%) were self-employed, 21 patients (33.9%) were employees, two patients (3.2%) were unemployed, seven patients (11.3%) were students, and four patients (6.5%) were engineers. Three of the patients had elementary education (4.8%), two patients finished junior high school (3.2%), one patient was studying at the high school (1.6%), 22 had finished high school (35.5%), and 34 patients had post secondary education (54.8%).
A total of 35 patients (56.4%) had grade II and 27 (43.6%) patients had grade III varicocele [Table/Fig-2].
Comparison of the frequency of varicocele grades in different study groups.
| Variable | Surgery (n=31) | L-Carnitine (n=31) | p-value |
|---|
| Varicocele Grading, no (%) | | | <0.001† |
| Grade II | 8 (25.8%) | 27 (87.1%) |
| Grade III | 23 (74.2%) | 4 (12.9%) |
| Smoking, no (%) | 9 (29%) | 6 (19.4%) | 0.374 |
| Sperm Count, no, million (SD) | 22 (±14.78) | 34.6 (±26.53) | 0.025† |
| Sperm Motility, percent (SD) | 21.74 (±8.05) | 33.9 (±10.44) | <0.001† |
| Sperm Concentration, no,million/ml (SD) | 3.57 (±1.47) | 2.95 (±0.87) | 0.05 |
| pH | 7.35 (±0.25) | 7.54 (±0.29) | 0.008† |
| RBC, no (SD) | 1.7 (±0.8) | 1.75 (±1.23) | 0.89 |
| WBC, no (SD) | 2.5 (±1.31) | 2.47 (±1.67) | 0.956 |
† statistically significant
SD: standard deviation
All the patients were married. 41 patients were non-smokers. Duration of the infertility ranged from 1 to 9 years, with a mean of 3.3 years. No statistically significant correlations was observed between duration of infertility and sperm volume (rs= -0.026, p = 0.87), motility (rs= -0.168, p= 0.29), and sperm count (rs= -0.214, p= 0.18).
There was no statistically significant difference between average sperm count and sperm concentration in varicoceles grades 1 and 2; however, sperm motility in varicocele grade III was significantly lower than grade II (p < 0.001). In the surgery group, frequency of grade III varicocele was higher (p < 0.001). Average sperm count, sperm motility, sperm volume, and pH in L-Carnitine group were significantly higher than surgery group (p < 0.05) [Table/Fig-3].
Comparison of sperm parameters in different grades of varicocele.
| Variable | Grade II (n=35) | Grade III (n=27) | p-value |
|---|
| Sperm Count, no, million (SD) | 31 (±24.7) | 24 (±18.1) | 0.203 |
| Sperm Motility, percent (SD) | 32 (±10.9) | 22 (±8.4) | <0.001† |
| Sperm Concentration, no, million/ml (SD) | 3.17 (±1.06) | 3.38 (±1.45) | 0.524 |
† statistically significant
SD: standard deviation
Average sperm count in the surgery group before the study was 22 million (vs 34.6 in L-Carnitine group) which rose to 28.61 million after six months (vs 45.37 in L-Carnitine group). The average motility in the surgery group before the study was 21.74 percent (vs 33.9 in L-Carnitine group) which increased to 35.38 percent after six months (vs 47.48 in L-Carnitine group). The average normal sperm morphology in the surgery group prior to the study was 46.25 percent (vs 56.61 in L-Carnitine group) which increased to 60 percent after six months (vs 69.7 in L-Carnitine group). The average volume of semen in the surgery group prior to the study was 3.5 cc (vs 2.95 in L-Carnitine group) which increased to 4.17 cc after six months (vs 4.33 in L-Carnitine group) [Table/Fig-4].
Comparison of mean and standard deviation of time liquefaction in the two medicines and surgery groups during the study.
| Index | Study group | Before the study | Three months later | Six months later | p- value |
|---|
| Time Liquefaction, second | Surgery | 13.48 (±4.6) | 13.70 (±5.64) | 12.58 (±4.31) | 0.448 |
| L-Carnitine | 20.51 (±19.11) | 17.54 (±5.62) | 17.83 (±6.91) | |
| Normal Morphology, percent (SD) | Surgery | 46.25 (±18) | 47.8 (±18.1) | 60 (±14.22) | 0.803 |
| L-Carnitine | 56.61 (±11.77) | 59.06 (±14.60) | 69.70 (±10.24) | |
| pH | Surgery | 7.35 (±0.25) | 7.37 (±0.229) | 7.50 (±0.29) | 0.555 |
| L-Carnitine | 7.54 (±0.294) | 7.58 (±0.358) | 7.96 (±2.25) | |
| WBC, no (SD) | Surgery | 2.5 (±1.31) | 2.22 (±1.47) | 2.18 (±1.51) | 0.463 |
| L-Carnitine | 2.47 (±1.64) | 1.61 (±1.32) | 2.51 (±2.06) | |
| RBC, no (SD) | Surgery | 1.70 (±0.806) | 1.68 (±1.13) | 2.1 (±1.11) | 0.097 |
| L-Carnitine | 1.75 (±1.23) | 1.15 (±1.06) | 1 (±1.51) | |
| Sperm Motility, percent (SD) | Surgery | 21.74 (±8.05) | 24.96 (±9.03) | 35.38 (±9.77) | 0.959 |
| L-Carnitine | 33.9 (±10.44) | 37.54 (±11.18) | 47.48 (±10.08) | |
| Sperm Count, no, million (SD) | Surgery | 22 (±14.78) | 23.40 (±18.83) | 28.61 (±16) | 0.391 |
| L-Carnitine | 34.6 (±26.53) | 39.87 (±30.47) | 45.37 (±27.73) | |
| Sperm Concentration, no, million/ml (SD) | Surgery | 3.5 (±1.4) | 3.32 (±1.21) | 4.17 (±1.22) | 0.12 |
| L-Carnitine | 2.95 (±0.875) | 3.08 (±1.279) | 4.33 (±1.04) | |
The analysis was carried out by repeated measures.
SD: standard deviation
During the study sperm parameters improved in both groups; however, no statistically significant difference was observed between the two groups. Thus, L-Carnitine was as effective as surgery in the improvement of sperm parameters.
Discussion
This study was conducted to compare the effect of oral administration of L-Carnitine and varicocelectomy on sperm parameters. Results of the study showed that, changes in sperm count, sperm motility, sperm normal morphology, and sperm concentration after varicocelectomy and administration of L-Carnitine were statistically higher than those values before the intervention. More patients with grade II varicocele were in the medicine group than in the surgery group and had higher sperm count, sperm motility, and sperm normal morphology than the surgery group. The sperm parameters during the study did not show a significant difference between the two groups. As a result, oral administration of L-Carnitine in grade II varicocele was as effective as varicocele surgery. It can improve the factors of male gametes through increasing the sperm count, sperm motility, sperm normal morphology, and semen deficiency. So, L-Carnitine can have a positive role in the management of infertility. Because of ethical issues we did not use randomization and it was our study limitation. Therefore, positive effects of L-Carnitine can only be generalized to grade II varicocele.
Another study showed that varicocelectomy increased the average sperm count, sperm motility, sperm normal morphology, and average seminal fluid volume [29]. Kibar et al., reported that there was a significant improvement in the sperm count after varicocelectomy, percentage of natural sperm motility, sperm normal morphology, sperm head form, and acrosom defect [30]. The results of a study conducted by Matkov et al., showed a significant increase in the percentage of sperm motility and sperm count in the semen [31]. There are few studies [32] that have reported ineffectiveness of varicocelectomy on seminal parameters. Hence varicocelectomy is known to be the only method [11].
Several studies on L-Carnitine were conducted, however their results are contradictory [24]. None of these studies compared the effects of surgery and L-Carnitine. A study conducted by Khademi et al., showed that L-Carnitine improved sperm concentration and sperm morphology [33]. In addition Li et al., showed a positive correlation between the levels of L-Carnitine in seminal fluid and sperm count, motility, and vitality [34]. Another study reported a significant increase in sperm concentration, overall motility, and forward motility, two months after the start of L-Carnitine [19]; however, no changes were observed in sperm volume and normal sperm morphology. Sperm concentration increased from 15 to 46 million per milliliter and the percentage of sperm motility increased from 21% to 48%; however, changes in semen volume and percentage of normal sperm morphology before and after treatment showed no significant difference. Compared with the period after administration of L-Carnitine and two months after termination of the treatment a significant decrease occurred in sperm concentration and motility. Cavallini et al., conducted a study on patients with idiopathic oligo asthenozoospermia (OAS) associated with varicocele [35]. They found that L-Carnitine/acetyl L-Carnitine + suppositories cinnoxicam were useful in treating low-grade varicocele and idiopathic oligo-asthenozoospermia. In Moncada’s study [36], taking L-Carnitine for 2 months was associated with increased motility.
Although, in Zhou et al., study confirmed the positive effect of L-Carnitine on enhancing male fertility as well [24]; some related studies have failed to show the same results. Sigman’s study showed that L-Carnitine had no statistical or clinical effect on sperm motility [22]. Lenzi’s study also showed that L-Carnitine was not effective in increasing the sperm count and normal sperm morphology [19].
Conclusion
Based on our findings medicinal treatment using oral L-Carnitine is as effective as varicocelectomy in improving semen parameters. Therefore, oral L-Carnitine can be used as an alternative to surgery in grade II varicocele.
† statistically significant
SD: standard deviation
† statistically significant
SD: standard deviation
The analysis was carried out by repeated measures.
SD: standard deviation
[1]. Gat Y, Bachar GN, Zukerman Z, Belenky A, Gornish M, Varicocele: a bilateral diseaseFertil Steril 2004 81:424-29. [Google Scholar]
[2]. Granados Loarca EA, Alcahe Gallimidi VR, Escobar Monzon C, The assessment of varicocele by ultrasoundActas Urol Esp 1999 23:579-82. [Google Scholar]
[3]. Jarow JP, Effects of varicocele on male fertilityHum Reprod Update 2001 7:59-64. [Google Scholar]
[4]. Cocuzza M, Cocuzza MA, Bragais FM, Agarwal A, The role of varicocele repair in the new era of assisted reproductive technologyClinics (Sao Paulo) 2008 63:395-404. [Google Scholar]
[5]. Agarwal A, Deepinder F, Cocuzza M, Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approachUrology 2007 70:532-38. [Google Scholar]
[6]. Retz PC, Sandlow JI, Varicocele: current concepts in pathophysiology, diagnosis, and treatmentUrol Clin North Am 2002 29:921-37. [Google Scholar]
[7]. Sandlow J, Pathogenesis and treatment of varicocelesBMJ 2004 328:967-68. [Google Scholar]
[8]. Pontonnier F, Mansat A, Mieusset R, Varicocelectomy for infertility is more effective in cases of sperm count less than 5 million/ml. Apropos of 70 casesAnn Urol (Paris) 1986 20:249-51. [Google Scholar]
[9]. Lacerda JI, Del Giudice PT, da Silva BF, Adolescent varicocele: improved sperm function after varicocelectomyFertil Steril 2011 95:994-99. [Google Scholar]
[10]. Marmar JL, Agarwal A, Prabakaran S, Reassessing the value of varicocelectomy as a treatment for male subfertility with a new meta-analysisFertil Steril 2007 88:639-48. [Google Scholar]
[11]. Will MA, Swain J, Fode M, The great debate: varicocele treatment and impact on fertilityFertil Steril 2011 95:841-52. [Google Scholar]
[12]. Inci K, Hascicek M, Kara O, Sperm retrieval and intracytoplasmic sperm injection in men with nonobstructive azoospermia, and treated and untreated varicoceleJ Urol 2009 182:1500-05. [Google Scholar]
[13]. Esteves SC, Oliveira FV, Bertolla RP, Clinical outcome of intracytoplasmic sperm injection in infertile men with treated and untreated clinical varicoceleJ Urol 2010 184:1442-46. [Google Scholar]
[14]. Ficarra V, Cerruto MA, Liguori G, Treatment of varicocele in subfertile men: The Cochrane Review–a contrary opinionEur Urol 2006 49:258-63. [Google Scholar]
[15]. Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM, Does varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trialEur Urol 2011 59:455-61. [Google Scholar]
[16]. Ghanem H, Shaeer O, El-Segini A, Combination clomiphene citrate and antioxidant therapy for idiopathic male infertility: a randomized controlled trialFertil Steril 2010 93:2232-35. [Google Scholar]
[17]. Oliva A, Dotta A, Multigner L, Pentoxifylline and antioxidants improve sperm quality in male patients with varicoceleFertil Steril 2009 91:1536-39. [Google Scholar]
[18]. Fang Y, Zhao L, Yan F, Escin improves sperm quality in male patients with varicocele-associated infertilityPhytomedicine 2010 17:192-96. [Google Scholar]
[19]. Lenzi A, Sgro P, Salacone P, A placebo-controlled double-blind randomized trial of the use of combined L-Carnitine and l-acetyL-Carnitine treatment in men with asthenozoospermiaFertil Steril 2004 81:1578-84. [Google Scholar]
[20]. Abd-Allah AR, Helal GK, Al-Yahya AA, Pro-inflammatory and oxidative stress pathways which compromise sperm motility and survival may be altered by L-CarnitineOxid Med Cell Longev 2009 2:73-81. [Google Scholar]
[21]. Buyse J, Swennen Q, Niewold TA, Dietary L-Carnitine supplementation enhances the lipopolysaccharide-induced acute phase protein response in broiler chickensVet Immunol Immunopathol 2007 118:154-59. [Google Scholar]
[22]. Sigman M, Glass S, Campagnone J, Pryor JL, Carnitine for the treatment of idiopathic asthenospermia: a randomized, double-blind, placebo-controlled trialFertil Steril 2006 85:1409-14. [Google Scholar]
[23]. Hinton BT, Snoswell AM, Setchell BP, The concentration of carnitine in the luminal fluid of the testis and epididymis of the rat and some other mammalsJ Reprod Fertil 1979 56:105-11. [Google Scholar]
[24]. Zhou X, Liu F, Zhai S, Effect of L-Carnitine and/or L-acetyL-Carnitine in nutrition treatment for male infertility: a systematic reviewAsia Pac J Clin Nutr 2007 16:383-90. [Google Scholar]
[25]. Lombardo F, Lupini C, Fiducia M, L-Carnitine fumarate, l-acetyL-Carnitine and other components in male infertility: a pilot study of nutraceutics on sperm motilityJournal of Andrological Sciences 2010 17:30-33. [Google Scholar]
[26]. Zopfgen A, Priem F, Sudhoff F, Relationship between semen quality and the seminal plasma components carnitine, alpha-glucosidase, fructose, citrate and granulocyte elastase in infertile men compared with a normal populationHum Reprod 2000 15:840-45. [Google Scholar]
[27]. Iacono F, Ruffo A, Prezioso D, Romeo G, Illiano E, Di Lauro G, Treatment of Bilateral Varicocele and Other Scrotal Comorbidities Using a Single Scrotal Access: Our Experience on 34 PatientsBioMed Research International 2014 :1-4.Doi:10.1155/2014/403603 [Google Scholar]
[28]. Kim HH, Goldstein M, A new clinical grading system for varicoceleFertility and Sterility [Internet] 2008 90Elsevier BV:S467Available from: http://dx.doi.org/10.1016/j. fertnstert.2008.07.324 [Google Scholar]
[29]. Moslemi Zadeh N, Isapour A, Peyvandi S, Moosa Nejad NA, Khani H, Effect of varicocelectomy on semen analysis parameters in patients with abnormal semen parametersJournal of Gorgan University of Medical Sciences 2005 7:34-38. [Google Scholar]
[30]. Kibar Y, Seckin B, Erduran D, The effects of subinguinal varicocelectomy on Kruger morphology and semen parametersJ Urol 2002 168:1071-74. [Google Scholar]
[31]. Matkov TG, Zenni M, Sandlow J, Levine LA, Preoperative semen analysis as a predictor of seminal improvement following varicocelectomyFertil Steril 2001 75:63-68. [Google Scholar]
[32]. McClure RD, Khoo D, Jarvi K, Hricak H, Subclinical varicocele: the effectiveness of varicocelectomyJ Urol 1991 145:789-91. [Google Scholar]
[33]. Khademi A, Alleyassin A, Safdarian L, The effects of L-Carnitine on sperm parameters in smoker and non-smoker patients with idiopathic sperm abnormalitiesJ Assist Reprod Genet 2005 22:395-99. [Google Scholar]
[34]. Li K, Li W, Huang YF, Shang XJ, Level of free L-Carnitine in human seminal plasma and its correlation with semen qualityZhonghua Nan Ke Xue 2007 13:143-46. [Google Scholar]
[35]. Cavallini G, Ferraretti AP, Gianaroli L, Biagiotti G, Vitali G, Cinnoxicam and L-Carnitine/acetyl-L-Carnitine treatment for idiopathic and varicocele-associated oligoasthenospermiaJ Androl 2004 25:761-70. [Google Scholar]
[36]. Moncada ML, Vicari E, Cimino C, Effect of acetylcarnitine treatment in oligoasthenospermic patientsActa Eur Fertil 1992 23:221-24. [Google Scholar]