The Arid Melancholy-Netherton Syndrome With Protein Energy Malnutrition
Sonia Pramod Jain1, Pramod Ajit Jain2, Neha Pandey3
1 Professor, Department of Skin and V.D., Mahatma Gandhi Institute of Medical Sciences, Sevagram, Wardha, Maharashtra, India.
2 Professor, Department of Orthopedics, Mahatma Gandhi Institute of Medical Sciences, Sevagram, Wardha, Maharashtra, India.
3 Junior Resident, Department of Skin and V.D., Mahatma Gandhi Institute of Medical Sciences, Sevagram, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sonia Pramod Jain, Professor, Department of Skin and V.D., Mahatma Gandhi Institute of Medical Sciences, Sevagram, Wardha, Maharashtra-442102, India.
E-mail: soniapjain@rediffmail.com
Netherton Syndrome (NS) is a rare autosomal recessive hereditary ichthyosiform disease with a classical triad comprising of an ichthyosiform dermatosis, hair shaft abnormalities and atopic diathesis. There is a mutation in a gene named Serine Protease Inhibitor Kazal type-5 (SPINK5); a new type of serine protease inhibitor involved in the regulation of skin barrier formation and immunity. Skin manifestations include, Ichthyosis Linearis Circumflexa (ILC), polycyclic and serpiginous, erythematous plaques with characteristic migratory, double-edged scale at the margins, or Congenital Ichthyosiform Erythroderma (CIE). Most of the patients have elevated immunoglobulin class E (IgE) and show atopic manifestations. Hair shaft abnormalities like pili torti and/or trichorrhexis nodosa, trichorrhexis invaginata, are seen.
Here, we report a rare case of Netherton Syndrome having ILC and trichorrhexis nodosa with protein energy malnutrition in a five-year-old school going girl. She belonged to a poor socio-economic background and was worried about her physical appearance due to her skin lesions, causing psychosocial morbidity to her.
Ichthyosis linearis circumflexa, LEKTI, SPINK5, Trichorrhexis nodosa
Case Report
A five-year-old female child visited the Department of Skin and VD with generalized erythema, pruritus along with history of scaling skin since birth. She found her skin lesions cosmetically disfiguring which was causing her social embarrasement not only at school but also at the hands of her family and friends, leading to psychological trauma.
She was born by vaginal delivery at full term, without any perinatal complications. No history of consanguinity was present. Her mother described that her hair was fairly normal after birth. In due course, fragility of hair increased with easy breakage and excessive scalp scaling. Her mental development was normal and the milestones were not delayed. However, malnutrition was evident and her weight was 10.7 kilograms. According to Indian Academy of Paediatrics, classification on the basis of weight she was diagnosed as suffering from Protein Energy Malnutrition (PEM) Grade 2. She had earlier received symptomatic treatment with topical and systemic corticosteroids intermittently; but there was no clear efficacy of treatment. There was positive history of atopy in the form of recurrent seasonal rhinitis although family history of atopy was not present. On physical examination there was generalized xerosis, erythema and excoriations, involving her face, neck, back, abdomen, upper chest wall, flexural creases of upper and lower extremities with characteristic polycyclic erythematous patches and serpiginous double-edged scales [Table/Fig-1,2]. The lesions over her upper limbs showed typical rippled appearance [Table/Fig-3]. There were areas of thinning and scaling with mild erythema in her scalp. She had coarse, straight, lusterless hair with some areas having more breakage than others [Table/Fig-4]. Her eyebrows were patchy throughout, especially on the lateral side. She had normal nails. The patient did not have any oral lesions or enlarged lymph nodes.
Polycyclic erythematous patches (shown with help of arrow)

Serpiginous double edged scales over trunk, abdomen and lower extremities.

Lesions over upper limbs with typical rippled appearance.

Coarse, straight, lusterless hairs with some areas having more breakage than others.

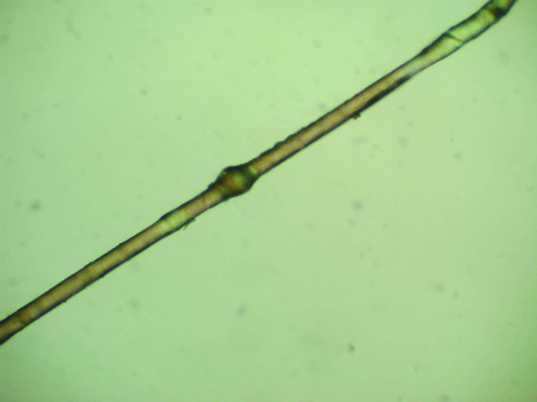
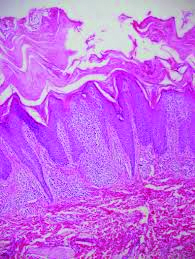
Complete haemogram showed anaemia, eosinophilia and neutrophilia. Serum IgE levels were raised. KOH mount of skin and scalp scaling was negative. Serum albumin was slightly decreased. Her Absolute Eosinophil Count, ESR and blood sugar were within normal limits. Light microscopy of her hair shaft revealed trichorrhexis nodosa [Table/Fig-5]. Histopathology showed severe hyperkeratosis with psoriasiform acanthosis and focal spongiosis present in the epidermis [Table/Fig-6]. Patient was treated with topical emollients and antihistaminics. She was also referred to paediatrician and started on haematinics, multivitamins and calcium supplements. She was given dietary advice along with parental counselling for the same. Patient was asked for regular follow up.
Light microscopy of hair shaft revealing trichorrhexis nodosa.
Histopathology shows severe hyperkeratosis with psoriasiform acanthosis and focal spongiosis present in the epidermis.
Over a period of 6 months the child gained weight. There was reduction in erythema and scaling, although she was not completely relieved of symptoms. The patient was advised to apply topical emollients on daily basis and she still continues to do so.
Discussion
Netherton Syndrome is a severe autosomal recessive skin disorder characterized by congenital ichthyosis, a specific hair shaft abnormality Trichorrhexis Invaginata (TI) or "bamboo hair" and atopic manifestations. Incidence of 1 in 200,000 has been reported but recent study reports that NS could account for up to 18% of congenital erythodermas [1].
The atopic diathesis occurs in approximately 75% of patients with NS [2]. Here atopic diathesis, comprises of eczematous eruptions, atopic dermatitis, asthma, pruritus, allergic rhinitis, angioedema, urticaria, elevated serum IgE level and/or hypereosinophilia [3].
The gene for NS has been identified on chromosome 5q32, named Serine Protease Inhibitor, Kazal Type-5 [3]. It encodes an inhibitor of serine protease enzyme called Lympho-Epithelial Kazal-Type-related Inhibitor (LEKTI) [3]. The function of serine protease enzyme is to break down the intracellular cement leading to desquamation of epidermal cells [2].
LEKTI may play a role in anti-inflammatory and/or antimicrobial protection of mucous epithelium [3]. This protein is also highly expressed in cultured epidermal keratinocytes; hence it could have a similar function in the epidermis [3]. LEKTI deficiency leads to an uninhibited desquamation of horny cells; making the skin becomes red and scaly [2]. Hair shaft abnormalities occur due to intermittent incomplete formation of disulfide bonds in the keratogenous zone [3].
Trichorrhexis invaginata (bamboo hair) is a focal defect of the hair shaft that produces development of torsion nodules and invaginated nodules; leading to an intussusception and a golf-tee-like deformity [3]. Other hair shaft abnormalities found in NS, include pili torti, trichorrhexis nodosa and helical hair [3]. Other common features that may be seen are enteropathy, aminoaciduria, mental retardation, and immunologic abnormalities [4].
Zhang et al., reported NS in a Chinese adult with a novel mutation in the SPINK5 Gene and Immunohistochemical Studies of LEKTI [5]. In an Indian case report by Sacchidanand et al., psoriasis got benefit of doubt on clinical evaluation, which was then diagnosed as NS, masquerading as psoriatic erythroderma in a two-year-old male child born of second degree consanguineous marriage [6]. Another case of NS was reported in India by Srinivas et al., with pili torti in a two-year-old female child [7]. Malakar et al., reported with ILC in a nine-year-old boy, the second issue of a non-consanguineous couple [8].
Patients with NS are more susceptible to systemic absorption of topical medication and are therefore at increased risk of adverse reactions [3]. Various systemic therapies have been attempted, including low-dose oral corticosteroids, retinoids and psoralen ultraviolet-A therapy [3].
Conclusion
Here we report this case of NS with Ichthyosis linearis circumflexa and Trichorrhexis nodosa, as a rarity because to the best of our knowledge NS has never been reported with protein energy malnutrition yielding morbidity to the paediatric patients. The syndrome can be an important condition in dermatology, which requires multi-speciality medical intervention, with not just dermatologists but also paediatricians playing an active part in its management, in order to achieve positive outcomes. Also, while treating such patient’s tender care and counselling is very important, in order to pacify these young souls, as the skin lesions may lead to serious psycho-social trauma and chronic persistant depression in such children.
[1]. Bitoun E, Chavanas S, Irvine AD, Lonie L, Bodemer C, Paradisi M, Netherton syndrome: Disease expression and spectrum of SPINK5 mutations in 21 familiesJ Invest Dermatol 2002 118:352-61. [Google Scholar]
[2]. Salodkar AD, Choudhary SV, Jadwani G, Singh A, Bamboo hair in Netherton’s syndromeInt J Trichol 2009 1:143-44. [Google Scholar]
[3]. Kumar R, Abhinandan HB, Mehta P, Jain S, Netherton’s syndromeIndian J of Paediatr Dermatol 2014 15:120-22. [Google Scholar]
[4]. Boskabadi H, Maamouri G, Mafinejad S, Netherton syndrome, a case report and review of literatureIran J Pediatr 2013 2:611-12. [Google Scholar]
[5]. Xi-Bao Z, San-Quan Z, Yu-Qing H, Yu-Wu L, Quan L, Chang-Xing L, Netherton syndrome in one Chinese adult with a novel mutation in the SPINK5 gene and immunohistochemical studies of LEKTIIndian J Dermatol 2012 57:265-68. [Google Scholar]
[6]. Aradhya SS, Srinivas SM, Hiremagalore R, Shanmukappa AG, Netherton syndrome masquerading as psoriatic erythrodermaIndian J Paediatr Dermatol 2014 15:89-91. [Google Scholar]
[7]. Srinivas SM, Hiremagalore R, Suryanarayan S, Budamakuntala L, Netherton syndrome with pili tortiInt J Trichol 2013 5:225-26. [Google Scholar]
[8]. Malakar S, Lahiri K, Sengupta SR, Ichthyosis linearis circumflexaIndian J Dermatol Venereol Leprol 1996 62:379-80. [Google Scholar]