Appearances are Deceptive – Passing a Nasogastric Tube does Not Always Rule Out Oesophageal Atresia
Manish Kumar1, Niranjan Thomas2
1 Associate Professor, Department of Neonatology, Christian Medical College, Vellore, Tamilnadu, India.
2 Professor and Head, Department of Neonatology, Christian Medical College, Vellore, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manish Kumar, Associate Professor, Department of Neonatology, Christian Medical College, Vellore, Tamilnadu-632004, India.
E-mail: maneeshdr@gmail.com
Oesophageal atresia/trachea-Oesophageal fistula is commonly diagnosed in the newborn period by inability to pass a nasogastric tube (NGT). We present the instance of a newborn baby where the diagnosis of oesophageal atresia was delayed because of an apparent successful passage of nasogastric tube to the stomach. Failure to reinsert the NGT raised the suspicion of oesophageal atresia which was confirmed by contrast study showing blind upper oesophageal pouch.
Newborn, oesophageal pouch, Trachea-oesophageal fistula
Case Report
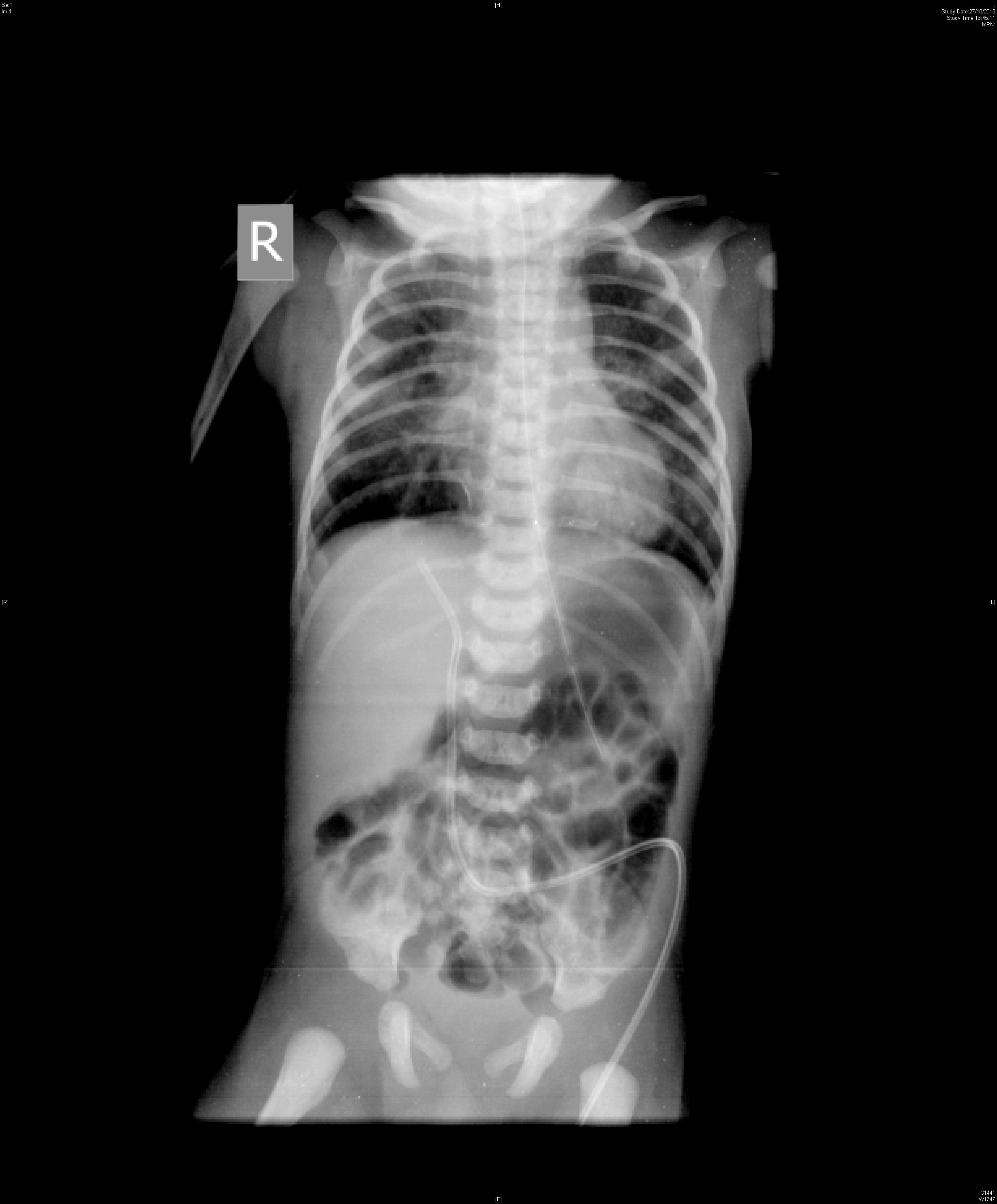
Baby a was born normally through meconium stained amniotic fluid at 40 weeks of gestational age with birth weight of 2790 g. Baby was referred to our hospital at 22 hours of life for management of respiratory distress. Antenatal ultrasound was not done. He was kept nil per oral, started on supplemental oxygen, antibiotics after blood culture and intravenous fluids. A 8 Fr NGT was successfully inserted and position of which was confirmed with auscultation and acidic pH of the aspirate from NGT. Chest x-ray [Table/Fig-1] was suggestive of meconium aspiration syndrome and NGT tip was in stomach. Baby continued to have respiratory distress. On day 3, he had worsening of respiratory distress with recurrent desaturation on high head box oxygen. In view of worsening respiratory distress baby was ventilated initially with conventional mode and later with high frequency oscillator. Antibiotics were upgraded after obtaining blood culture. Inotropes were also started in view of poor perfusion. On day 3, NGT was dislodged and could not be reinserted to full length despite repeated attempts. Failure to pass NGT raised the suspicion of oesophageal atresia. Contrast study was done which showed blind upper oesophageal pouch with no communication to trachea and lower oesophagus [Table/Fig-2]. Echocardiography was done which ruled out congenital heart defect. Baby could not be operated in view of deteriorating cardiorespiratory condition secondary to Klebsiella septicaemia. Baby died on day 4 of life because of septic shock. Parents refused autopsy.
Chest x-ray showing nasogastric tube tip in stomach.
Contrast radiograph showing blind upper oesophageal pouch with no communication to trachea and lower oesophagus.

Discussion
The incidence of oesophageal atresia (OA) is 1:2500 births [1]. The classical presentation is excessive frothing of saliva and choking episodes with or without feeds. Five types of OA had been described: type A to E. Type C (OA with distal fistula) is the most common lesion which accounts for approximately 90% of the OA. Prenatal diagnosis of OA is not possible in all the cases. Stringer et al., has described that the sensitivity of ultrasound was only 42% to diagnose OA antenatally. The polyhydramnios and an absent stomach bubble had positive predictive value of 56% [2]. Diagnosis of OA in newborn is generally straightforward with classical history of excessive frothy oral secretions, choking episodes and inability to pass NGT to stomach. The classical teaching to diagnose oesophageal atresia is passing a large calibre (10 Fr) feeding tube from the mouth to stomach when there is suspicion of oesophageal atresia based on clinical feature or prenatal ultrasound finding of absent stomach bowel or polyhydramnios. Chest x-ray both AP and lateral view should be taken if you are unable to pass the feeding tube beyond 10 cm. Diagnosis of OA is presumed when the tip of feeding tube tip is stopped around thoracic inlet and a coiled NGT in upper oesophageal pouch [1]. The presence of bowel gas indicates the presence of a trachea-oesophageal fistula. Routinely, contrast study is not required to establish the diagnosis of OA. In our case, diagnosis of OA was missed initially because of lack of clinical suspicion, antenatal ultrasound and correct placement of NGT into stomach which was confirmed on chest x-ray. The most likely reason that we could assign was that the NGT had gone into the trachea and through the trachea-oesophageal fistula into the lower oesophagus and further into stomach. Delay in diagnosis had further complicated the management of an already sick baby.
Similar to our case, Celayir and Erdogan had described an infant with OA in whom diagnosis was delayed due to initial passage of oral tube into stomach via distal tracheoesophageal fistula [3]. Kuti et al., and Soccorso et al., had also described similar cases [4,5].
Conclusion
Hence, smooth passage of NGT into stomach may not always rule out all cases of OA. Rarely NGT can make its way into stomach through abnormal route which cannot be excluded with usual auscultation and acidic NGT aspirate. Whenever, there is doubt a larger 10 Fr and stiffer feeding tube should be used to rule out OA and contrast radiograph should be done if diagnostic dilemma persists. This knowledge and high index of suspicion can help in early diagnosis that can prevent life-threatening events of aspiration.
[1]. Spitz L, Esophageal atresiaJ Pediatr Surg 2006 41(10):1635-40. [Google Scholar]
[2]. Stringer MD, McKenna KM, Goldstein RB, Filly RA, Adzick NS, Harrison MR, Prenatal diagnosis of esophageal atresiaJ Pediatr Surg 1995 30(9):1258-63. [Google Scholar]
[3]. Celayir AC, Erdoan E, An infrequent cause of misdiagnosis in esophageal atresiaJ Pediatr Surg 2003 38(9):1389 [Google Scholar]
[4]. Kuti K, Patel R, Chapman S, Jawaheer G, A rare pitfall in the diagnosis of oesophageal atresiaPediatr Radiol 2013 43(8):902-04. [Google Scholar]
[5]. Soccorso G, England RJ, Godbole PP, Fisher RM, Marven SS, Mind the gap: delayed diagnosis of oesophageal atresia and tracheo-oesophageal fistula due to passage of a nasogastric tubeArch Dis Child Fetal Neonatal Ed 2012 97(6):F463-64. [Google Scholar]