Subdural Haemorrhage (SDH) is a form of brain haemorrhage in which there is a collection of blood between the dura and the arachnoid layers of the meninges. It is usually associated with mechanical brain injury [1]. The occurrence of subdural haemorrhage may or may not be associated with any visible injury to scalp, skull or brain. Hence, radio imaging tools remain the only method to diagnose subdural haemorrhage and its characteristics in surviving patients [2]. Computed Tomography (CT) is routinely utilized for the diagnosis of acute SDH [3].
The CT scan finding of an SDH depends on the age of the haemorrhage. In the hyperacute phase, they appear relatively iso-dense to the adjacent cortex, with a swirled appearance due to a mixture of a clot, serum, and ongoing unclotted blood. In the acute phase, SDH appears as a hyper-attenuated crescent-shaped extra-axial collection. As the haematoma ages, it becomes more and more hypo dense. Sometimes areas of hyperdensities can be found within a hypodense area, indicating rebleeding as in cases of acute on chronic SDH [4]. The attenuation coefficient defines the extent to which the intensity of an energy beam is diminished as it passes through a particular material [5]. CT numbers/attenuation mainly depends on measurement technique, object composition, and beam energy [6].
From the clinical point of view, classification of subdural haemor-rhage into different ages or post-traumatic Intervals (PTI) based on its density on CT scan decides the further course of management of the patients. Though discussion on the management of subdural haemorrhage is out of the scope of this paper, few points can be noted. Hyperdense subdural haematomas are usually managed by craniotomy and at times by performing craniectomy. The surgical procedures like trephination and twist drill craniotomy are used in the management of hypodense subdural haemorrhage. Subdural Evacuating Port System (SEPS) are more efficient in draining Subdural Haematomas (SDHs) that are hypodense on CT scans than in evacuating mixed density SDHs [7–10].
As far as Magnetic Resonance Imaging (MRI) is considered, it is more sensitive than CT in the detection of SDH because of its multi-planarity and superior tissue differentiation properties. More than 95% sensitivity has been reported with T2- weighted images of SDH because of the marked variation in signal intensity between blood products and adjoining structures [11]. Further with the passage of time, the variation in the MRI appearance of SDH can indicate the approximate stage of haemorrhage and even the age of the blood clot [12]. These observations have immense forensic applications where multiple traumatic events have occurred in the same case, in cases with the paucity of external injuries or in cases with repeated non-accidental trauma. Thus the radiological dating of SDH is of immense help, both from the forensic point of view as well as for the management of the patient.
From the forensic perspective, the radiological tools have been valuable in the detection of foreign bodies, disaster victim identifications, child abuse, gunshot wounds, traffic accidents, and air embolisms [13]. However, only a few studies have described the changes occurring in SDH using CT [14–16] or MRI [12] with relation to the time of occurrence of the traumatic event. Few histological studies on the aging of SDH have also been conducted and till date remains as the gold standard [17,18]. Interest in the application of attenuation numbers in forensic radiology has again evolved recently following many studies on its reliability and reproducibility [19,20]. The purpose of this study was to determine the Post-traumatic Interval of SDH based on Hounsfield measurements on CT in surviving patients.
Materials and Methods
After obtaining clearance from the ethical clearance committee of Post Graduate Institute of Medical Education And Research (PGIMER), Chandigarh, the present study was conducted in Department of Forensic Medicine, in collaboration with Department of Radio diagnosis & Imaging and Department of Neurosurgery during the period July 2009 to December 2010. With a valid written consent of the legal heirs of the patients, a total of 300 cases in the age group of 18 years and above, with a diagnosis of subdural haemorrhage were investigated out of which 100 cases satisfied the inclusion/exclusion criteria and hence was included in this study. This study is also the first of its kind to be conducted in India.
The findings of head CT done at the time of diagnosis were noted. Conservatively treated cases of SDHs with a known mode, manner and topography of the incident were included in this study. All those cases with history of ataxia, stroke attacks, dementia, haemorrhagic tendencies (liver cirrhosis, anticoagulant therapy, and haemorrhagic diathesis), known prior traumatic brain injuries and with more than one episode of epilepsy were excluded from this study. Also, excluded were cases that were surgically treated and in whom rebleeding was noted (clinically and radiological). Time of the accident was recorded in each instance from the hospital as well as police records and further verified from the relatives/friends of the victims. The post-traumatic interval varied from 0.5 hours to a maximum of 249 hours, with a mean of 54.2 hours.
Radiological Procedure
Non-contrast computed tomography of the head was done using single slice hi-speed GE machine scanner with a tube current of 130 mA, tube voltage of 120 kVp and a slice thickness of 10 mm (Window Width -150 HU, Window centre -75HU). The clinical, as well as police records of the patients, were reviewed and the time interval between the occurrence of trauma and Non-contrast computed tomography was noted. All the measurements were performed on a picture archiving and communication system (PACS) workstation.
The crescentic subdural haematoma having the maximum length (the linear distance between the corners of the subdural haemorrhage crescent) in any single slice was chosen for HU measurement. To avoid the partial volume effect and to maintain a constant relationship between the diameter of ROI and the breadth of the haemorrhage, a circular region of interest (ROI) along the maximum breadth of the haematoma was chosen for HU measurement in all cases [19,20]. The diameter of the circular ROI was adjusted to half the maximum breadth of SDH. If the haematoma was present in more than one slice, then the average HU measurement of all those slices were taken as mentioned above. The HU measurements were measured away from the rim of the subdural haemorrhage to avoid partial volume effect. The reader-dependent differences in HU measurements were assessed by two observers blinded to PTI. To assess intra-reader reliability, each reader repeated HU measurements thrice in an individual case with an interval of three weeks between each measurement.
Though the scanner and the protocol utilized in the present study, not being state of the art, an attempt was made to determine roughly the effect of the volume of the subdural haematoma on its attenuation. The volume of the chosen SDH was calculated by the ABC/2 or XYZ/2 method [21], i.e. half the product of depth, length and breadth of the SDH. Length was measured as the linear distance between the corners of the SDH crescent. The breadth was measured as the maximum distance of haematoma from the inner table of the skull perpendicular to the length. The depth was determined by multiplying the number of slices on which haematoma was visible, by the slice thickness.
Statistical Analysis
Data was analysed using SPSS (SPSS 17 for Windows, Chicago, IL, USA). A p-value <0.05 was considered significant. The relationship between the mean of the first and the second reader’s observation was determined using Kendall’s tau b test. Intra-reader reliability was assessed using the intraclass correlation coefficient (ICC). Since the data was not normally distributed, Nonparametric Mann-Whitney test was carried out to determine the difference in the mean values of the first and the second reader’s observation. In order to predict PTI based on density/attenuation and volume of the SDH, logistic regression was applied, for which the cases were divided into 2 groups based on PTI (Group 1 < 48 h, Group 2>48h).
Results
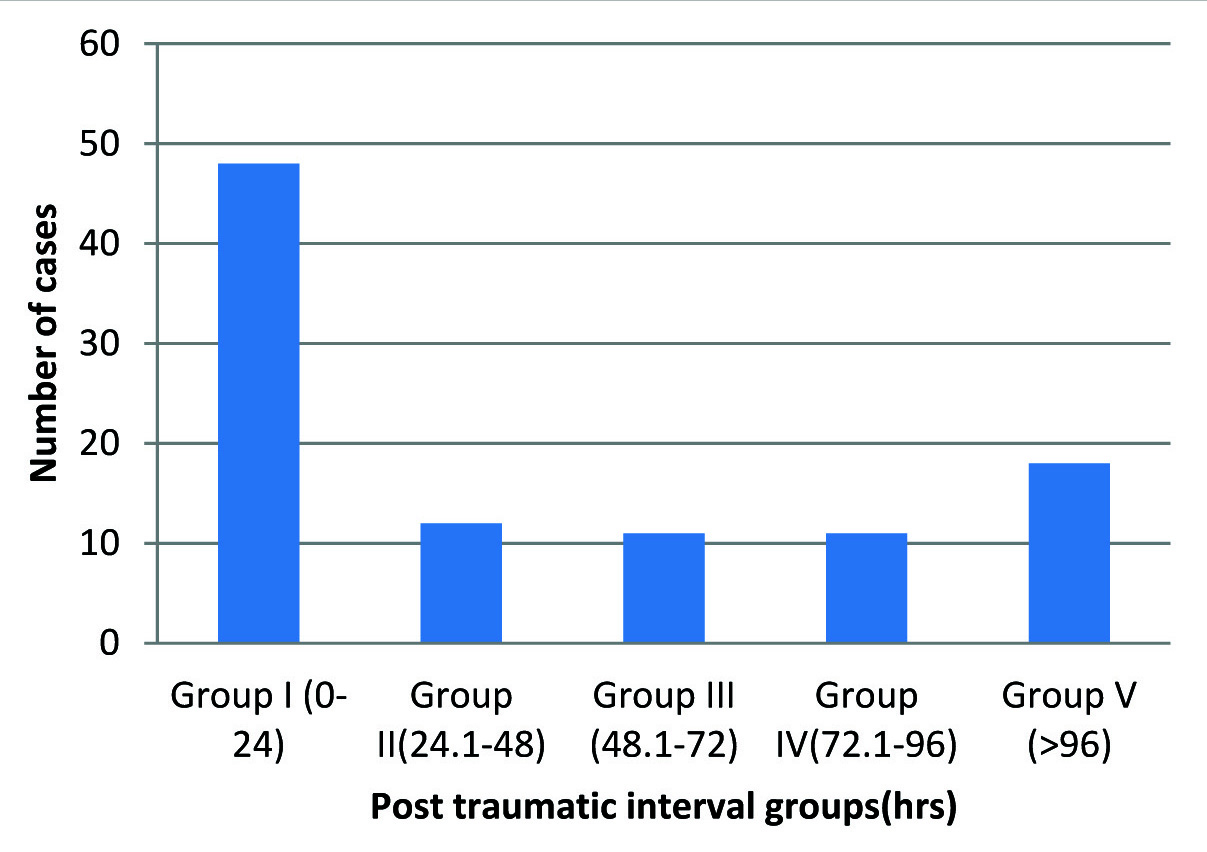
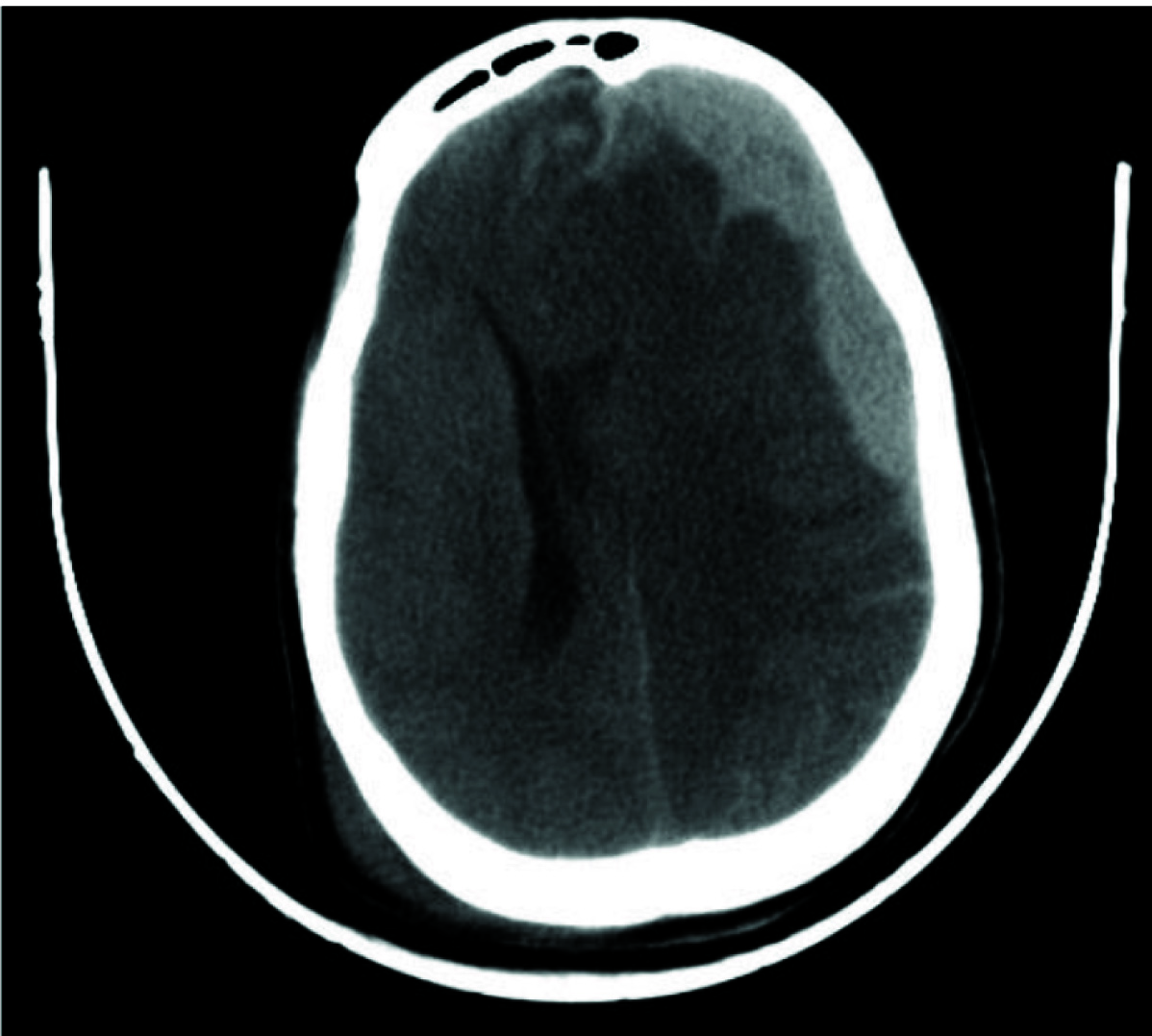
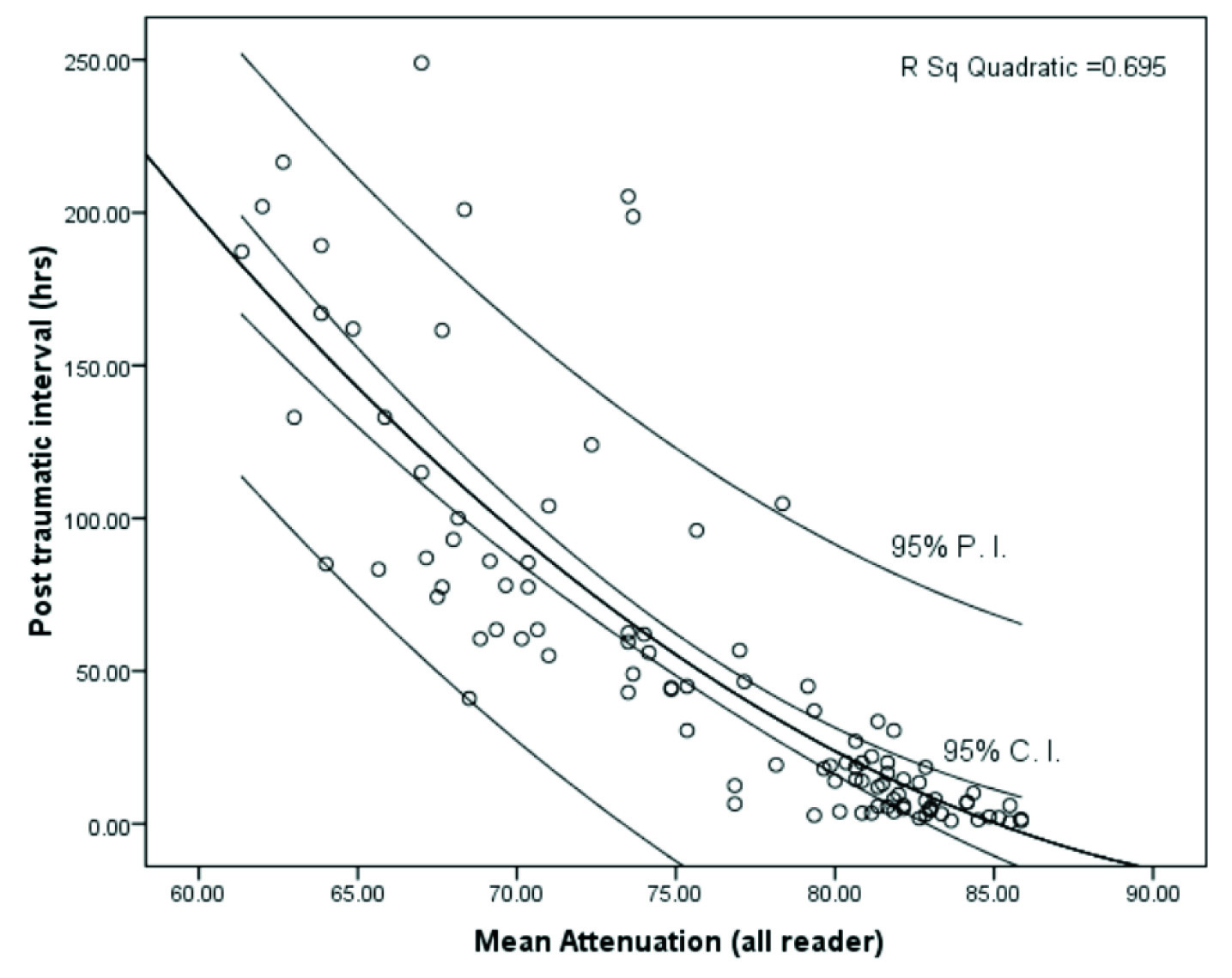
A total of 100 cases in the age group of 18-85 years were studied. The post-traumatic time interval varied from 0.5 hours to a maximum of 249 hours, with a mean of 54.2 hours [Table/Fig-1]. All the cases of SDH were hyperdense in the present study [Table/Fig-2]. The volume of the SDH varied from 0.16 cm3 to 92.4cm3 with a mean of 13.62cm3 (SD=20.39, SEM=2.03) [Table/Fig-3]
Frequency distribution of cases according to the post-traumatic interval
Axial view: A crescentic subdural haematoma over the left fronto-parieto-temporal region with a contralateral midline shift
Distribution of cases according to the post-traumatic interval and mean attenuation of subdural haemorrhage
The data was tested for normality using Kolmogorov-Smirnov test [Table/Fig-4] and was found out to be non-normal. Hence, Mann-Whitney test [Table/Fig-5] was applied to determine the difference between the mean of both readers observations and was found out to be insignificant (p=0.752, mu=4870.50). Kendall tau b test [Table/Fig-5] was applied between the average attenuation of the two readers and showed a significant correlation (tk=0.892, p=0.0001). The intra-class correlation coefficient for intra-reader reliability of the first and second readers were 0.968 (p =0.0001) and 0.960 (p = 0.0001) respectively.
Kolmogorov Smirnov test (for testing normality of data).
| Time | Observer 1(1st reading) | Observer 1(2nd reading) | Observer 1(3rd reading) | Observer 2(1st reading) | Observer 2 (2nd reading) | Observer 2(3rd reading) |
|---|
| Kolmogorov Smirnov- Z | 1.878 | 1.937 | 1.660 | 1.967 | 1.886 | 1.690 | 1.470 |
| p- value | .002 | .012 | .008 | .001 | .002 | .007 | .026 |
Mann Whitney Test and Kendall’s tau b.
| Observer | Mean Rank | Mannwhitney -U Statistic | p-Value |
|---|
| 1st Observer | 101.80 | 4870.5 | 0.752 |
| 2nd Observer | 99.20 |
Kendall’s tau b=0.892, p=.0001
Logistic regression [Table/Fig-6] (Forward LR method) of relevant forensic PTI was also performed. The maximum number of cases were observed within 24hrs of PTI (n=48), and most of them had overall average HU measurements above 80 HU. More than 85% of cases with overall mean attenuation of less than 70HU were observed predominantly after the 3rd day. None of the cases with PTI greater than 48 hours had an overall mean attenuation greater than 80 HU. Based on this, cases were divided into two groups, with one group having PTI of less than 48 hours (n=60) and the other with PTI of more than 48 hours (n=40). The prediction of PTI was based on density and volume. In logistic regression, after applying forward likelihood ratio method, only density was found out to be significant and is used in the model to predict PTI. This model correctly classified 93% of the original cases. Volume was non-significant in the prediction of PTI (p=0.866).
| Chi-square | df | Sig. |
|---|
| 8.166 | 8 | .417 |
| -2 Log likelihood | Cox & Snell R Square | Nagelkerke R Square |
| 5.642a | .628 | .849 |
| Classification Tablea |
|---|
| Observed | Predicted |
|---|
| Actual time | Percentage Correct |
|---|
| <= 48.00 | 48.01+ |
|---|
| Step 1 | Actual time | <= 48.00 | 56 | 4 | 93.3 |
| 48.01+ | 3 | 37 | 92.5 |
| Overall Percentage | | | 93.0 |
| a. The cut value is .500 | | | |
| Variables in the Equation |
|---|
| B | S.E. | Wald | df | Sig. | Exp(B)Odds Ratio | 95.0% C.I.for EXP(B) |
|---|
| Lower | Upper |
|---|
| Mean | -.639 | .139 | 21.009 | 1 | .000 | .528 | .401 | .694 |
| Constant | 47.925 | 10.506 | 20.809 | 1 | .000 | | | |
a. Variable(s) entered on step 1: mean.
Discussion
The timing of a traumatic event by post-mortem findings carries immense significance for the forensic experts. Multiple methods to determine the age of injury are available which include but not limited to the healing of abrasions, contusions, and other injuries. The aim of the present study was to determine the post-traumatic interval of the early subdural haematomas based on computed tomography attenuation numbers. In this study, crescent shaped haemorrhages were distinctively selected to determine the effect of blood volume on attenuation.
The variation in density pattern is observed on computed tomography about extravasation of blood with time [14–16]. An acute subdural haemorrhage has a computed tomographic attenuation value that is dependent largely on the proportions of red blood cells, haemoglobin and iron content, and fibrin. An acute thrombus is formed from fibrin, platelets, neutrophils, and red blood cells, and as the cells start losing its integrity, swelling often occurs [17].
Attenuation also depends on beam energy and may, therefore, differ significantly between different CT scanners. Earlier studies have reported Scanner-dependent variability in CT numbers [19,22,23]. However, in Strandberg et al., study, the use of two different CT-scanners did not affect the results in a significant way [20]. This contention was avoided in our study by the utilization of a single CT machine with a single standard specification for all the cases.
Few studies have been attempted long back for dating the subdural haemorrhage using computed tomography. Bergstroem et al., observed that the densities of extra-axial haematomas decreased at a predictable rate of time [16]. Scotti et al., reported the attenuations of subdural haemorrhages on CT as hyperdense in 100% of cases in acute cases (7days), iso-dense in 70% of sub-acute, (8-22 days) group and hypo dense in 76% of the chronic (>22 days) group [15]. Lee et al., in their study found that the density of acute (<7 days) was hyperdense in 98.6%, iso-dense in 1.1% and hypo dense in 0.3% of the cases [14]. All the above studies have tried to classify subdural haemorrhage into acute, subacute or chronic depending on the attenuation. The present study, unlike others, included only early cases of SDH and further differentiation of the haemorrhage according to age was attempted within this short post-traumatic interval. It is pertinent to note that these studies also do not mention the specific radiological methods applied in estimating the age of the subdural haematoma.
After about 10-14 days of the clot formation, the density drops to about 30HU and becomes isodense with the adjacent cortex [4]. Since the cases in the present study were well within or close to 10 days, all the cases had a high attenuation, which is in concordance with all the above published data. Further classification showed that the maximum number of cases was observed within 24hours of the post-traumatic interval (n=48), and most of them had attenuation numbers above 80HU. More than 85% of cases with attenuation less than 70HU were observed predominantly after the 3rd day. Only 4 cases with a PTI of less than 24hours had a lower attenuation in the range of 71-80HU. Correlation of attenuation of the haematoma and time interval between injury and computed tomography was found to be highly negative i.e. there was a decrease in the attenuation of the haematomas with the progression of the post-traumatic interval [Table/Fig-3].
The determination of the post-traumatic interval of the subdural haemorrhage is a complex problem and has been worked out by a very few investigators. Hence a very limited number of studies with which the results of the present study could be compared. These findings accord with the results of other studies examining Intra-reader reliability of attenuation measurements [19]. Currently, the dating of subdural haemorrhage by measuring the CT number alone could lead to inaccuracies as it depends on measurement technique, object composition, and beam energy. Therefore with further research on this subject, the attenuation of subdural haemorrhages can be measured with more reliability and, thereby placing them accurately into particular post-traumatic interval groups.
The forensic relevance of the age/time course of intracranial haemorrhage is especially relevant to reconstructing sequel events and a determination by HU, differentiating acute from hyperacute haemorrhage would add crucial value-especially for postmortem radiology exams. However, the outcome of living patients may not be entirely transferable to post-mortem radiology. The application of the current methodology to post-mortem cases will be an oversimplification. Though, the few post-mortem radiological studies conducted previously have inferred minimal difference with the autopsy findings in cases of craniocerebral trauma, not much work has been done on decomposed bodies [23,24]. Further in these studies [23,24], the cases had a time interval of less than 24hours between the death and postmortem radiological examination. These studies concentrated mainly on the gross features rather than going into specifics like aging and the degree of the autolytic process if any.
From the radiological point of view, the dating of early SDH remains limited, in the fact that all the SDH were hyper dense, but concurs with the already published data [4,25,26]. However, on a further classification of these HU numbers about post-traumatic intervals, information was obtained on the range of attenuation for a particular post-traumatic interval. Though few studies suggest that dating of subdural haematoma cannot be done accurately using radiological methods [25–27], the present study, yet gives a reliable and a reproducible method for the estimation of the age of early subdural haemorrhage.
Not many studies have been conducted recently on the radiological dating of SDH. Those studies which have dealt with the radiological dating of SDH have not specified the radiological methods and hence the comparison with different studies have been limited. The results from one of the recently conducted questionnaire based study showed that there was a considerable variation among the radiologists, regarding medico-legal opinions on the age of SDH and concluded it unsuitable to use in court because of non-uniformity [28].
Limitations of The Study
The study was limited by the small sample of materials investigated. SDH of longer duration (>11days) were not studied. The influence of hypothermia, shock, hypoxia, variations in the blood pressure, the effect of medications during emergency care, potential effects of associated injuries and failure of the internal organs were not evaluated. Repeat CT examinations of the same patient at various times were not done in our study. Also, a single CT scan machine was used in this study hence variations in attenuation between different CT Scanners could not be appreciated.
Because of the difficulty in differentiation into antemortem and postmortem breakdown of cellular components, it is hard to predict the post-traumatic intervals in decomposing bodies.
Finally, the CT Scanner and protocol that have been used in this study is not the state of the art concerning its various parameters. Though single slice CT scanners are not used in state of the art head scans [29], the constraints on the availability of advanced scanners in a developing country like India, has compelled us to use the resources at hand.
Future Prospects
A long-term study involving more number of cases helps in the better understanding of the attenuation variations of the SDH with relation to time.
Further this study could be extended to cases below 18 years of age that hold a lot of medico-legal significances.
More innovative research can be done by the application of HU measurements on different organs in determining the time since death.
Considering a few recent studies being done on the postmortem use of the radiological technologies in the interpretation of the cranio-cerebral traumatic injuries [23,24] one can with some confidence say that these methods hold a lot of stake for the future of radiological autopsy or may indeed replace few of the routinely conducted forensic autopsies of the present times.
Conclusion
The present study has adopted one of the most objective and scientific methods in determining the attenuation of the subdural haematomas in contrast to the other previous studies where none has been applied or has not been mentioned. Though this study has been limited to the early post-traumatic intervals, it could still grasp some significant findings in the form of variations in the attenuation of the subdural haemorrhage with relation to time of the injury. The attenuation of the acute subdural haemorrhage decreased with increase in the post-traumatic interval. On further classification of these HU numbers about post-traumatic intervals, information was obtained on the range of attenuation for a particular post-traumatic interval. The variations in the hospital care and treatment, the mode of injuries (high velocity), have considerably changed over the years and hence could have contributed to the observed variations despite proper study design. These are also in part due to the dynamic character of such injuries and the various manner in which trauma victims react to an injury.
Kendall’s tau b=0.892, p=.0001
a. Variable(s) entered on step 1: mean.