Treatment of Resıstant Cyclophosphamide Induced Haemorrhagic Cystıtıs: Revıew of Literature and Three Case Reports
Turgay Ebiloglu1, Engin Kaya2, Sercan Yilmaz3, Gökhan Özgür4, Yusuf Kibar5
1 Faculty, Department of Urology, Etimesgut Military Hospital, Ankara, Turkey.
2 Faculty, Department of Urology, Section of Pediatric Urology, Gulhane Military Medical Academy, Ankara, Turkey.
3 Faculty, Department of Urology, Section of Pediatric Urology, Gulhane Military Medical Academy, Ankara, Turkey.
4 Faculty, Department of Heamatology, Gulhane Military Medical Academy, Ankara, Turkey.
5 Faculty, Department of Urology, Section of Pediatric Urology, Gulhane Military Medical Academy, Ankara, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Turgay Ebiloglu, Etimesgut Military Hospital, Department of Urology, 06010 Etimesgut/Ankara, Turkey.
E-mail: drturgayebiloglu@gmail.com
Haemorrhagic Cystitis (HC) is defined as diffuse inflammatory bladder bleeding due to many aetiologies. Massive HC often arises from anticancer chemotherapy or radiotherapy for the treatment of pelvic malignancies. Phosphamides are the anti-cancer drugs used for treating breast cancer, B-cell lymphoma, leukemia, rheumatoid arthritis and systemic lupus erythaematosis by cross-linking strands of DNA and preventing the cell division. They are also used in bone marrow transplantation for prevention of Graft Versus Host Disease (GVHD). Hepatic metabolism of phosphamide forms acrolein, and acrolein makes ulceration, haemorrhage, edema and necrosis of the urothelium during its excretion by the urine. Infectious causes of HC in immunocomprimesed patients are adenovirus, BK polyoma-virus (BK), JC virus, and Cytomegalovirus (CMV). The present article attempts to make a review of literature for the treatment of intractable HC and report three cases with HC.
Cidofoxin therapy, Clot, Haematuria
Case Report 1
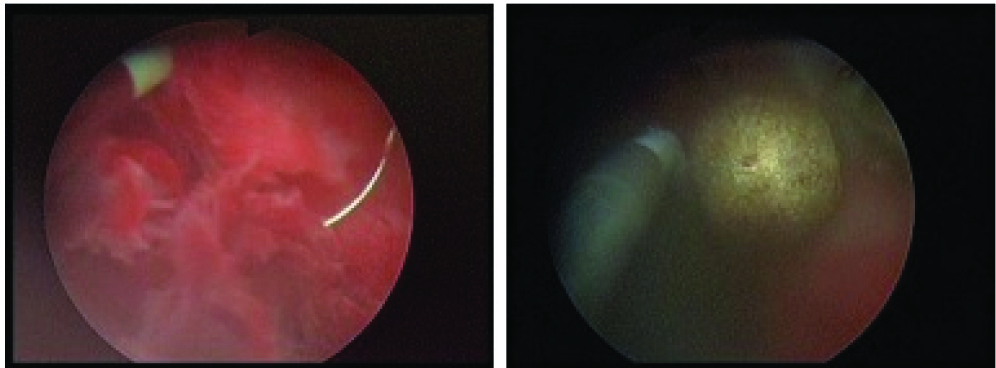
Our first patient was a 22-year-old male patient. He was on the follow up course of ALL with remission. On his 3-month-control WBC count was detected high in CBC with 71% blast formation and relapse of ALL was thought. The patient was hospitalized and salvage chemotherapy was started with IDA-FLAG (idarubicin, fludarabine, cytarabine, G-CSF) regimen. After 1 month from IDA-FLAG, his blood WBC count was still high and his bone marrow aspiration was full of blastic cells. Haploidentical Haematopoietic Stem-Cell Transplantation (HHSCT) was thought of due to the resistant ALL disease. Clofarabin chemotherapy was started concomitant to IDA-FLAG. Clofarabin managed the remission and HHSCT was applied with the stem cells from his father. Cyclophosphamide chemotherapy was started for preventing Growth Versus Host Disease (GVHD). After 10 days from HHSCT, macroscopic haematuria began and MESNA with oral hydration was started for suppression of haematuria. 24 French 3-way urethral catheter was applied and irrigation was started. PCR test detected BK virus as 9.9X109 copy positive in urine sample and haematuria became significant. Cidofovir therapy was started for BK virus. Although BK virus count decreased to 9.1X109 with cidofovir, haematuria became severe. Leflunamide was started for resistant BK virus but haematuria was still severe. Factor 7 was thought of as the last option for stopping haematuria but glob vesicale (haematoglob) developed. Ultrasound (USG) showed the bladder with full of clot. Resection and evacuation of the resected parts of the clot were considered. A 24 F resectesope was proceeded towards urethra. Clot was resected but it was difficult to comply with that big clot. Cystotomy, clot removal, ureteral stenting were applied [Table/Fig-1]. The bladder mucosa seemed haemorrhagic. Three days from operation urine colour was normal but after that time mild haematuria started again and BK virus was still positive. Patient died and septic shock.
Cystotomy (open surgery), clot removal, ureteral stenting, and cystostomy

Case Report 2
Our second patient was a 32-year-old male patient. He had a relapse of ALL with positive Philadelphia chromosome. HHSCT was applied with same drug regimens of the first patient. Cyclophosphamide was begun after HHSCT. After 40 days from transplantation, severe haematuria started. 24 French 3-way urethral catheter was applied and irrigation was started. PCR test detected BK virus as 5 X 109 copy positive in urine sample. Cidofovir therapy was started for BK virus but BK virus count did not decrease. Glob vesicale (haematoglob) developed. USG showed clot formation in the bladder. Firstly, cystoscopic removal of clot was tried but could not be managed. Cystotomy, clot removal, and bilateral nephrostomy were performed secondly. Urine colour became normal after operation but acinetobacter caused septic shock caused the patient death.
Case Report 3
Our third case was a 14-year-old male patient. He had ALL. He had bone marrow transplantation and post transplant cyclophosphamide chemotherapy. After 30 days from transplantation haematuria began. An 18 French 3-way urethral catheter was preceded from urethra and irrigation was started. Bilateral nephrostomy were applied for diversion of urine. BK virus was positive in urine and blood cultures. Cidofovir therapy was started for BK virus but BK virus count did not decrease. Despite these interventions haematuria became severe. Cystoscopy, clot removal, and cystostomy were applied. After operations, irrigation via cystostomy and urethral catheter was continued. Glob vesicale with clot (haematoglob) in bladder appeared after 7 days from operations. A 24 F resectescope was proceeded towards cystostomy tract because of small caliber urethra of a 14-year-old male patient. Haematoglob resection, evacuation, and coagulation of haemorrhagic areas were applied successfully [Table/Fig-2]. Urine colour became normal and patient got well and discharged with remission after a month.
Resection of clot and coagulation of haemorrhagic areas
Discussion
Severe HC is a major complication in the population taking anti-cancer chemotherapy or undergoing haematopoietic stem cell transplantation [1]. It is defined as the presence of gross haematuria with clots and associated clinical complications [2].
MESNA is the oral or intravenous medication binds with acrolein in the urine and always used while phosphamide therapy. The protective effect of MESNA is reported in various studies [3]. Hyperbaric oxygen is another option of preventing HC, but the results are not satisfactory [4]. In our patients, MESNA was used but haematuria did not resolve and became severe. So we used cidofovir, leflunomide and Factor 7 for first patient. Cidofovir is an injectable antiviral medication primarily used as a treatment for DNA viruses in immuno-comprimised patients [5]. Leflunamide is an immunosuppressive disease-modifying antirheumatic drug used in active moderate to severe rheumatoid arthritis and psoriatic arthritis. It is a pyrimidine synthesis inhibitor and reported to be effective in HC with BK virus [6–8]. Factor 7 was thought to stop haemorrhagic areas [9].
Irrigation agents for haemorrhagic cystitis in literature are alum, prostaglandins, ice irrigation, formalin, ε-aminocaproic acid and fibrin glue. Despite these therapeutic options, severe HC continues to be a devastating condition with significant associated morbidity and mortality [10]. Similarly our first and second cases died after development and treatment of HC.
Because of many side effects above, use of these irrigation agents is limited especially in children [10]. If these conservative therapies fail, clot evacuation by cystoscopy or resectoscope is the next step. Ohhara et al., coagulated the haemorrhagic areas broadly in bladder and reported good result [11]. After evacuation of clot, irrigation with agents above should be applied to bladder to obtain from clot formation and maintain urine leakage. In our first case we performed clot resection by resectoscope but it was not enough for evacuation. In our second case we performed cystoscopy and could not evacuate the clot either. In our third case we performed resection and evacuation of clot successfully due to smaller clot size than first two cases.
Diversion of urine in haemorrhagic cystitis is reported in some case reports. Percutaneous Nephrostomy (PN) is the easiest diversion method. PN drainage decreases urokinase levels within the bladder. Urokinase is a proteolytic enzyme produced by the kidney under the control of serum urokinase levels and acts to convert plasminogen to plasmin [12]. Stable clot can be able to form under low urikinase levels and this situation allows bladder mucosal healing. PN also decreases bladder urine and thereby decreases the microvascular trauma associated with bladder distention [13]. Cystectomy remains the final treatment option for patients with severe radiation cause HC that is resistant to other treatments. Alkan et al., applied laparoscopic cystectomy to a patient and Okaneya et al., applied cystectomy and ileal neoblabber to a patient with severe HC [14,15]. Both reported good results and well tolerability. Ureterocutaneostomy without cystectomy is not reported in literature. In our first case we performed open clot removal and bilateral ureteral stenting. In our second patient we performed open clot removal and bilateral nephrostomy. Both patients had normal urine colours, but the second patient lived longer. On the other hand, we performed bilateral nephrostomy for third case and he was discharged from hospital with remission. So bilateral nephrostomy seems to be a better option rather than ureteral stenting.
Conclusion
Open clot removal without cystectomy with ureter catheterization or nephrostomy is a new treatment option for intractable HC.
Abbreviations
BK : BK polyoma-virus
CMV : Cytomegalovirus
GVHD : Graft versus host disease
HC : Haemorrhagic cystitis
HHSCT : Haploidentical haematopoietic stem-cell transplantation
USG : Ultrasound
[1]. Lukasewycz SJ, Smith AR, Rmabachan A, MacMillan ML, Lewis JM, Shukla AR, Intractable haemorrhagic cystitis after haematopoietic stem cell transplantation: Is there a role for early urinary diversion in children?J Urol 2012 188(1):242-46. [Google Scholar]
[2]. Bedi A, Miller CB, Hanson JL, Goodman S, Ambinder RF, Charache P, Association of BK virus with failure of prophylaxis against haemorrhagic cystitis following bone marrow transplantationJ Clin Oncol 1995 13:1103 [Google Scholar]
[3]. Ali SA, Danda SK, Basha SA, Rasheed A, Ahmed O, Ahmed MM, Comparision of uroprotective activity of reduced glutathione with Mesna in Ifosfamide induced haemorrhagic cystitis in ratsIndian J Pharmacol 2014 46(1):105-08. [Google Scholar]
[4]. Del Pizzo JJ, Chew BH, Jacobs SC, Sklar GN, Treatment of radiation induced haemorrhagic cystitis with hyperbaric oxygen: long-term follow upJ Urol 1998 160(3 Pt 1):731-33. [Google Scholar]
[5]. De Clercq E, Therapeutic potential of Cidofovir (HPMPC, Vistide) for the treatment of DNA virus infectionsVerh K Acad Geneeskd Belg 1996 58(1):19-47. [Google Scholar]
[6]. Dougados M, Emery P, Lemmel EM, Zerbini CA, Brin S, van Riel P, When a DMARD fails, should patients switch to sulfasalazine or add sulfasalazine to continuing leflunamide?Ann Rheum Dis 2005 64(1):44-51. [Google Scholar]
[7]. Pinto P, Dougados M, Leflunamid in clinical practiceActa Reumatol Port 2006 31(3):215-24. [Google Scholar]
[8]. Chen XC, Liu T, Li JJ, He C, Meng WT, Huang R, Efficacy and safety of leflunomide for the treatment of BK virus-associated haemorrhagic cystitis in allogeneic haematopoietic stem cell transplantation recipientsActa Haematol 2013 130(1):52-56. [Google Scholar]
[9]. Ashrani AA, Ganriel DA, Gajewski JL, Jacobs DR, Weisdorf DJ, Key NS, Pilot study to test the efficacy and safety of activated recombinant factor VII (NovoSeven) in the treatment of refractory haemorrhagic cystitis following high-dose chemotherapyBone Marrow Transplant 2006 38(12):825-28. [Google Scholar]
[10]. Manikandan R, Kumar S, Dorairajan LN, Haemorrhagic cystitis: A challenge to the urologistIndian J Urol 2010 26(2):159-66. [Google Scholar]
[11]. Ohhara M, Okumura S, Tsuboi N, Kanamori S, Yoshida K, Nishimura T, Severe cyclophosphamide haemorrhagic cystitis controlled with transurethral electrocoagulation: a case reportHinyokika Kiyo 1985 31(6):1045-48. [Google Scholar]
[12]. Hong SY, Pyo SJ, Lee HB, Effect of serum urokinase on urine fibrinolytic activityNephron 1990 55:287-291. [Google Scholar]
[13]. Lukasewycz SJ, Smith AR, Rmabachan A, MacMillan ML, Lewis JM, Shukla AR, Intractable haemorrhagic cystitis after haematopoietic stem cell transplantation: Is there a role for early urinary diversion in children?J Urol 2012 188(1):242-46. [Google Scholar]
[14]. Alkan I, Jeschke S, Leeb K, Albquami N, Janetschek G, Treatment of radiation-induced haemorrhagic cystitis with laparoscopic cystoprostatectomyUrol Int 2006 77(2):190-92. [Google Scholar]
[15]. Okeneya T, Kontani K, Komiyama I, Takezaki T, Severe cyclophosphamide-induced haemorrhagic cystitis successfully treated by total cystectomy with ileal neobladder substitution: a case reportJ Urol 1993 150(6):1909-10. [Google Scholar]