Reproductive health is an important issue for every country, and increasing contraceptive utilisation is one of the Millennium Development Goals. Despite the increase in contraceptive prevalence, most women still have an unmet need for contraception. Furthermore, many women use traditional family planning methods that are less reliable than modern methods [1–8].
Turkey is a country with a population of about 77 million with a young population structure [9]. The total fertility rate between 2003 and 2008 has been almost stable at 2.3 and 2.2, respectively [10]. During the last 20 years, the use of modern contraceptive methods increased from 31% to 46%. However, 27% of women in Turkey are still relying on traditional methods, especially withdrawal (26%) [11]. The level of traditional method use remained unchanged during the last decade. Approximately half of the contraceptive methods are male-controlled, such as coitus interruptus or condom use [10,11]. Despite the social improvements and legal reforms, socioeconomic structures remain male-dominated. Studies from Turkey have shown that partners’ attitudes and approval have an effect on contraceptive practice [12–15]. Six percent of women have an unmet need for contraception. This percentage varies according to geographical location and reaches 14% in the eastern part of the country. The 92 percent of Turkish mothers received obstetric care during pregnancy [11]. Therefore, antenatal care (ANC) may be a window of opportunity to access many women for contraceptive counselling.
In the literature, the integration of family planning education into obstetric care has been suggested to increase postpartum contraception use. The factors contributing to postpartum contraceptive use have been studied previously and include socio-demographic factors, prior experiences, obstetric care service utilisation, and antenatal-postnatal education [16–27]. The differences in the time and type of educational interventions and the heterogeneity of the population have yielded diverse outcomes [16–20]. Lopez et al., reviewed the studies from four countries and suggested that postpartum education increases contraceptive use [18]. Prior study performed by Zerai et al., investigated the role of prenatal care for modern contraceptive use in Bolivia, Egypt and Thailand. They suggested that prenatal care strongly affects subsequent modern method use [21]. The data from the Demographic and Health Survey (DHS) in Kenya showed that ANC service intensity and previous method use were related to postpartum contraception [22]. A study from Nigeria found that multiple antenatal contraceptive counselling sessions increased modern contraceptive use compared to a single postpartum education session [23]. Yee et al., suggested that ideally, counselling includes brief educational sessions presented to patients throughout ANC, but the postpartum period should support and re-evaluate these decisions [24].
Although, the postpartum period is a unique time to reach out to couples to initiate contraception, there are few data regarding the best approach. The majority of the studies have explored antenatal and postnatal counselling separately [21–28]. Few studies have addressed the contraceptive use after both prenatal and postnatal counseling [24,29]. Furthermore, there is no prospectively designed study on this matter. This study evaluated the impact of the addition of individualised postnatal education to antenatal education on modern contraceptive use among Turkish women.
Materials and Methods
Setting
This study was performed in Gölcük, Kocaeli, Turkey. The province of Kocaeli is in Northwestern Turkey and is one of the most densely populated cities and the most industrialized areas of Turkey. Gölcük is a district in the Kocaeli province, with the majority of the people literate, work and live around the health facility. The Gölcük Public Hospital is the only hospital in this district, and its Maternity Unit has an average of 1,300 deliveries annually.
Study Design and Participants
This prospective controlled study was conducted from January 2012 to March 2013 at the Gölcük Public Hospital, Kocaeli, Turkey. The cohort consisted of all pregnant women at more than 24 weeks of gestation (n=250) who was seen for prenatal care between January and February 2012. Each participant received contraceptive education throughout her ANC. The inclusion criteria were the receipt of at least two prenatal contraceptive counselling sessions and delivery of the baby at the same hospital. Women who delivered at another centre (n=16), who underwent postpartum tubal sterilisation (n=2), who had fewer than two prenatal care visits (n=2) or who did not provide consent (n=10) were excluded from the study. A total of 220 women were recruited to participate in the study. [Table/Fig-1] shows the recruitment protocol flow diagram.
Recruitment protocol flow diagram.
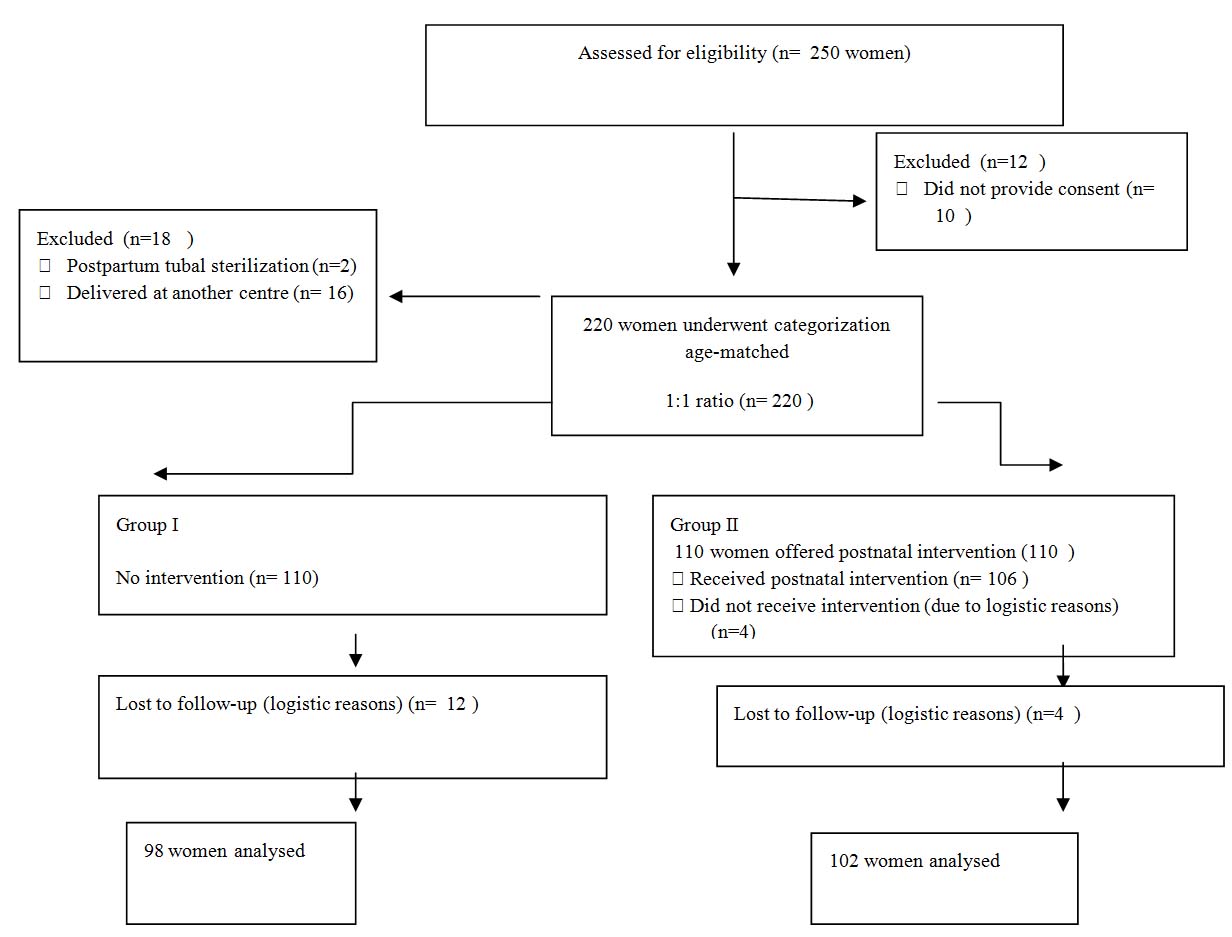
After delivery, women were categorised into two groups. An individual blinded to the study protocol selected the age-matched groups with a 1:1 allocation ratio in the order of date of delivery. No further intervention was performed for Group I (only prenatal education group). Women in Group II were given additional contraceptive education at six weeks after hospital discharge (both antenatal and postnatal education).
Six months after delivery, a telephone interview was conducted, and the contraceptive method was determined. The primary measure outcome was modern contraceptive utilisation {intrauterine device, barrier methods, injectable contraceptives, LAM (Lactational Amenorrhea Method), contraceptive pills}. LAM defined as modern temporary method for women whose menstruation has not returned and exclusively breastfeeding infants less than six months. Traditional methods were coitus interruptus and the calendar method.
This study protocol followed the ethical principles of the Helsinki Declaration and was approved by the Kocaeli University Medical Faculty Institutional Review Board. Written informed consent was obtained from all participants.
Counselling
Contraceptive education was performed by two family planning nurses (NS, MA). The gynaecologist (FV) was in charge of overseeing the team.
Antenatal Counselling: Family planning counselling was given by a nurse to all patients with their partners via informative brief communications during each prenatal examination. This advice included general information about postpartum contraceptive needs, return of fertility after childbirth, contraceptive methods, lactation, and sexual health.
Postpartum Counselling: The individualised family planning counselling at the sixth-week postpartum was performed by a family planning nurse and lasted 30 min. The husbands were allowed to attend this session. The two main components of postpartum counselling were general information (reproductive health, sexual issues, and postpartum contraceptive methods) and problem-oriented support. If couples choose a method, they were offered the same-day assistance in the family planning unit for IUD insertion, free distribution of condoms or contraceptive pills, and injectable contraceptive.
Statistical Analysis
The data were analysed using the Statistical Package for Social Sciences (SPPS) 16 software (SPSS Inc., Chicago, IL, USA) within a 95% confidence interval. The descriptive data were expressed as mean, standard deviation, and a percentage. Comparisons of different variables were performed by the one-way ANOVA test and the χ2-test. The relationships between the data were evaluated using Pearson’s and Spearman’s correlations. The Levene and Welch tests were used to test for homogeneity of variances. The effects of independent and non-parametric variables on the dependent variables were studied using logistic regression analysis.
Results
Participants: A total of 200 women aged 18–43 years were included in the study. Of the participants, 98 women were in Group I, and 102 women were in Group II. The mean age±SD of the women was 27.9±5.3 years in Group I and 28.9±4.3 years in Group II. The characteristics of the participants are presented in [Table/Fig-2]. The comparison of groups for maternal age, parity, previous unintended pregnancies, educational status of patients and their husbands, partners’ support and ANC visits had insignificant differences (p>0.05). The homogeneity of variances were similar (p>0.05). A total of 187 (93.5%) women had more than four ANC visits. The 40% of women planned pregnancy before conception, none desires a child for a time after delivery. Most of the women (n=140, 70%) chose a family planning method with their partners.
Characteristics of participants.
| Group I | Group II | p-value |
|---|
| Maternal age | | | 0.963 |
| <30 Years | 58.2% | 57.8% | |
| ≥30 Years | 41.8% | 42.2% | |
| Number of previous births | | | 0.524 |
| 0-1 Births | 42.8% | 42.2% | |
| 2-4 Births | 54.1% | 52.9% | |
| ≥4 Births | 3.1% | 4.9% | |
| Number of previous abortions | | | 0.740 |
| 0-1 Abortion | 97% | 96% | |
| ≥2 Abortions | 3% | 4% | |
| Antenatal care visits | | | 0.453 |
| 2-4 Visits | 5.1% | 8.1% | |
| ≥ 4 Visits | 94.9% | 91.9% | |
| Educational status | | | 0.790 |
| Primary School | 40,8% | 47.1% | |
| Secondary and High School | 59.2% | 52.9% | |
| Employment | | | 0.773 |
| No | 61,2% | 58.8% | |
| Yes | 38.8% | 41.2% | |
| Husband Education | | | 0.252 |
| Primary School | 28.6% | 21.6% | |
| Secondary and High School | 71.4% | 78.4% | |
| Husband’s support | 70.4% | 69.6% | 0.901 |
The Comparison of Contraceptive Use in Group I versus Group II : The comparison of postpartum contraceptive methods was similar between groups (p >0.05). When all the participants’ contraceptive methods before and after birth were compared, the contraceptive percentages increased significantly in both groups (p<0.05). The comparison of contraceptive methods in Groups I and II presented in [Table/Fig-3].
The comparison of contraceptive methods in Group I and II.
| Group I | Group II | p-value |
|---|
| After pregnancy | | | |
| Modern methods | 48 (49%) | 62 (60.8%) | 0.093 |
| Traditional methods | 46 (47%) | 38 (37.2%) | 0.165 |
| No method | 4 (4%) | 2 (2%) | 0.379 |
| Before pregnancy | | | |
| Modern methods | 40 (40.8%) | 46 (45.1%) | 0.540 |
| Traditional methods | 31 (31.6%) | 33 (32.3%) | 0.913 |
| No method | 27 (27.5%) | 23 (22.5%) | 0.414 |
Of the participants, 55% used modern methods, and 42% used traditional methods, and 3% used no method during the postpartum period. Postpartum contraceptive methods were IUD (n=50, 25%), condom (n=47, 23.5%), pills and injectables (n=10, 5%), LAM (n=3, 1.5%), coitus interruptus (n=70, 35%), and calendar method (n=14, 7%). Women in Group I used IUD (n=19), condom (n=23), pills and injectables (n=5), LAM (n=1), coitus interruptus (n=40), and the calendar method (n=6). Women in Group II used IUD (n=30), condom (n=25), pills and injectables (n=5), LAM (n=2), coitus interruptus (n=30), and the calendar method (n=8).
Confounding Factors : Each demographic factor from [Table/Fig-2] was analysed for its correlation with current contraceptive use. The educational status of women and their partners had no significant relation to postpartum contraceptive use (p>0.05). Educational status of women (r: 0.389) and their partners (r: 0.281) related to the number of living children (p<0.05). The results showed that ANC visit intensity (r: 0.313), contraceptive experience (r: 0.175), and husbands’ support (r: 0.283) were related to postpartum contraceptive use (p<0.05). The relevant factors were accepted as possible confounding factors. [Table/Fig-4] shows the logistic regression analysis of confounding factors for postnatal modern contraceptive use in Groups I and II separately. The dependent variable was the postpartum current contraceptive use, and the independent variables were the obstetric care visits, husband’s approval, and prior modern contraceptive use. Logistic regression analysis showed that PPMC was independent of confounding factors in each group.
Postpartum modern contraceptive use in Group I and II. Logistic regression analysis of confounding factors within the groups.
| Exp B | CI | p-value |
|---|
| Group I | | | |
| Partner’s support | 1.5 | 0.6- 3.7 | 0.34 |
| Number of ANC | 0.6 | 0.1-4.4 | 0.686 |
| Past experience with modern contraception | 3.0 | 0.8-10.5 | 0.08 |
| Group II | | | |
| Partner’s support | 1.6 | 0.6-4.0 | 0.257 |
| Number of ANC visits | 3.8 | 0.6-21.2 | 0.122 |
| Past experience with modern contraception | 2.2 | 0.7-6.4 | 0.127 |
Discussion
The present study explored the effects of, the addition of sixth-week postnatal contraceptive counselling to antenatal education on modern contraceptive use. Both interventions, either prenatal or combined prenatal-postnatal, increased postpartum contraceptive use compared to prior contraceptive use. However, the addition of postpartum contraceptive counselling to antenatal one does not improve the prevalence of PPMC significantly.
Postpartum contraception is essential to optimise pregnancy intervals and reduce unplanned pregnancies, thereby reducing maternal and child mortality, but there are few data to suggest the best approach to encourage the use of modern contraceptive methods. Although prior studies have reported the effects of prenatal counselling on postpartum contraceptive use, there are few data about the effect of postnatal counselling in combination with antenatal education [24,29]. Our paper is the first prospective controlled study of the combined effect of pre- and postnatal education on contraceptive use in Turkey. Family planning counselling throughout pregnancy increased contraceptive use, and these results are similar to those of Adanikin et al., [23]. Recently, Zapata et al., analysed retrospective data from the Pregnancy Risk Assessment Monitoring System [29]. Their findings showed that the prevalence of PPMC increased when counselling was provided both during antenatal and postnatal periods [29]. In our study, despite postpartum sixth-week counselling has the advantage of referring couples directly to a family planning unit, the addition of postnatal counselling to antenatal education did not further increase PPMC comparing to only antenatal education.
Education is one of the indicators of woman’s status. Empowerment education enhances woman’s autonomy, social mobility and knowledge. In this study, educational status of women and their partners related to number of living children, but no relation with current contraceptive use. In addition to education, behavioural changes in reproductive health matters, depend on many factors, such as socio-demographic characteristics, community factors, male partners, contraceptive experiences, and health care service quality [4,5]. This study showed that 70% of women needed their husband’s approval for contraceptive decision making. Although the sample size was small and local, the results concerning obstetric care service use and partner’s involvement were similar to previous studies performed in Turkey [12–15]. Previous studies in Turkey show that that partners’ attitudes and approval have an effect on contraceptive practice [12–15]. In this study, the relevant factors of PPMC were obstetric care visit intensity, husband’s support and prior contraceptive experience. Logistic regression analysis showed that PPMC was independent of confounding factors in each group.
Strength and Limitations
Although this paper gave new insight to postpartum contraceptive counselling, the study had some deficits that limit the generalisation of the results. Because a randomisation was not feasible, there might have been a potential risk of bias in patient selection. To minimise bias risk, age-matched women were allocated in a 1:1 ratio according to the order of date of delivery, and potential confounding factors were investigated. Although, the results were adjusted for potential confounding factors, residual bias cannot be excluded. Consequently, randomised controlled trials with modern contraceptive methods as an endpoint are needed to determine the clinical significance of the associations we observed.
Conclusion
The addition of the sixth week postnatal contraceptive counselling to antenatal one does not further improve the prevalence of PPMC. These results suggested that family planning education should be provided to all pregnant women during antenatal care. Future prospective randomized controlled studies of combined counselling are needed.