Primary breast actinomycosis is a rare condition that has been previously reported in the female breast. Male breast infection is uncommon and most often associated with trauma to the skin or predisposing conditions like diabetes. We report the first case to our knowledge of primary breast actinomycosis in the male breast caused by Actinomycesneuii (A. neuii), a rare strain of Actinomyces. Mammography demonstrated periareolar skin thickening with a mottled pattern. Sonography showed multiple small cystic structures. Definitive diagnosis was made by culture of the nipple discharge.
Actinomycesneuii, Mammogram, Nipple discharge, Sinus tract, Ultrasound
Case Report
A 24-year-old male with a medical history of Human Immunodeficiency Virus (HIV) and syphilis and no history of trauma presented to his primary care physician reporting white left nipple discharge for several years. The patient had undergone bilateral reduction mammoplasty for gynecomastia eight years previously.
On physical examination, there was white purulent discharge from the left nipple with mild periareolar skin thickening. There were no discrete left breast masses or enlarged axillary nodes. Scarring from prior bilateral reduction mammoplasty was evident. The contralateral right breast demonstrated no mass.
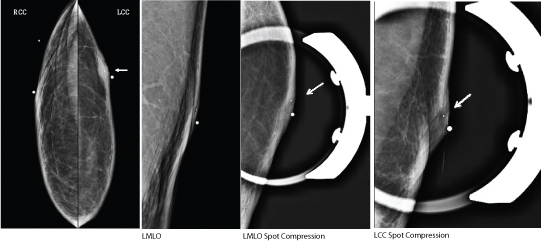
Bilateral digital mammography demonstrated changes consistent with reduction mammoplasty including dermal and fat necrosis calcifications. The nipples were laterally displaced due to surgery [Table/Fig-1a-c]. Compression view of the left nipple demonstrated skin thickening with an internal mottled pattern [Table/Fig-1d,e].
Bilateral mammography including right craniocaudal(RCC) (a), Left Craniocaudal (LCC) (b), Left Medio Lateral Oblique (LMLO) (c), LMLO spot compression (d) and LCC spot compression (e) views. Diagnostic mammogram demonstrated changes related to reduction mammoplasty including displacement of the nipple, skin thickening and dermal calcifications (white arrow). Spot compression views of the left nipple demonstrated enlargement of the left nipple with a mottled pattern and calcifications.
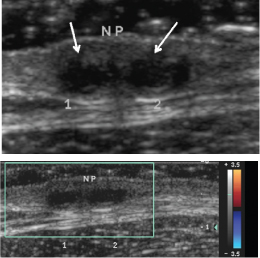
Sonogram of the left breast showed no discrete breast mass. In the subareolar region, there were two adjacent irregular cystic structures measuring 0.5 x 0.4 x 0.4 cm and 0.5 x 0.5 x 0.5 cm consistent with small abscesses [Table/Fig-2 a,b].
Sonogram of the left subareolar breast in longitudinal axis (a) demonstrates two adjacent irregular cystic structures (white arrows) measuring approximately 0.5x0.4x0.4cm and 0.5x 0.5x0.5 cm. Colour Doppler (b) demonstrates no vascular flow.
A culture of the discharge was obtained which was positive for A. neuii. The patient was placed on two weeks of Augmentin and did not return for follow-up.
Discussion
Actinomyces are gram-positive, anaerobic bacteria normally found in oral flora, colon and vagina. Infection typically occurs through breaches in mucosal barriers. Actinomycosis is an indolent, slowly progressive, suppurative granulomatous disease, which often produces draining sinus tracts. It can occur in healthy individuals [1] [Table/Fig-3].
Summary table of primary breast actinomycosis in men.
| Aetiology | Unknown; possible causes include trauma, surgery, lactation, kissing |
| Incidence | Rare |
| Gender Ratio | Cases reported thus far in women; extremely rare in men |
| Age Predilection | Premenopausal women, unknown in men |
| Risk Factors | Usually healthy individuals with no associated diseases |
| Treatment | Treatment of choice is prolonged antibiotic treatment with penicillin. Percutaneous drainage of associated abscess if present. Surgical intervention if medical therapy fails. |
| Prognosis | Excellent |
Actinomycosis can be subdivided into primary and secondary forms. Breast actinomycosis is primary when inoculation occurs through the nipple. Less than 32 cases have been reported since 1893 [1]. Possible causes of primary breast actinomycosis include trauma and infection [2]. Secondary breast actinomycosis is extension of pulmonary infection through the thoracic cage [3] [Table/Fig-3].
The most common species in the breast is Actinomycesisraelii, accounting for 78% of primary breast actinomycosis [1]. Other strains that have been identified as causative pathogens in primary breast actinomycosis include A. viscosus, A. turicensis, and A. radingae [4]. A. europaeus was also recently reported as a causative pathogen in male breast abscess [5]. These species are all anaerobic and appear as branching rods on pathological examination. In contrast, A. neuii is rarely responsible for infections in humans. It represents 17% of all Actinomyces species and differs from the rest of the species because it is aerobic and exhibits non-branching rods on microscopic evaluation. The most common types of infections caused by A. neuii are abscesses and infected atheromas [6]. We present the first case to our knowledge of a rare strain of actinomyces, A. neuii, causing breast abscess formation in a male patient.
Breast actinomycosis typically involves the nipple as the primary site of inoculation. Clinically, patients may have varying presentations including breast mass, skin induration, draining sinus tracts with purulent or bloody discharge, or nipple discharge [2,3]. Association with nipple piercing has been reported in women [7].
Mammographic findings are variable. They include skin thickening, a retroareolar mass, or sinus tract formation characterized mammographically as dense tracts connecting a breast density to the skin. In advanced cases, there may be fibrosis and architectural distortion of the breast tissue. There have been no reported cases of associated calcifications in the breast or axillary adenopathy [2] [Table/Fig-4].
Differential table of focal skin thickening, mass, abscess, and/or sinus tract formation in male breast on imaging.
| Mammographic Appearance | Sonographic Appearance |
|---|
| Primary breast actinomycosis | Localized skin thickening, retroareolar mass or sinus tract formation. Fibrosis and architectural distortion in advanced cases.No associated calcifications [2] or adenopathy. | Abscess, sinus tracts and/or skin thickening.Abscesses often well-defined with no internal Doppler flow [2]. |
| Infectious mastitis | Unilateral breast enlargement with skin and trabecular thickening. Associated abscess may present as irregular mass with or without calcifications. Adenopathy may be evident [9]. | Skin thickening. May have associated abscess presenting as irregular, heterogeneous mass with increased Doppler flow at periphery of lesion [10]. |
| Breast cancer | Can present with skin thickening or retraction +/- architectural distortion or an eccentric mass. May have associated indeterminate calcifications [11] or axillary adenopathy. | Irregular hypoechoic mass, complex cystic mass, skin thickening,Colour Doppler may show increased flow within the mass or just in the tissues surrounding the mass [10] |
| Tuberculosis/Syphilis | Focal skin thickening, coarse stromal texture, sinus tract, or abscess formation.Nodular forms may present as multiple nodular opacities.May or may not have associated axillary adenopathy [7]. | Focal skin thickening. Sinus tract or abscess formation without increased Doppler flow [7].Nodular forms may present as multiple, heterogeneous hypoechoic masses with irregular border or thick-walled cystic lesions with septa. |
Sonographic findings depend on the mammographic characteristics. These range from skin thickening, complex breast masses suggestive of abscess and/or sinus tracts to the skin. When present, abscesses are often well-defined with no internal Doppler flow [2] [Table/Fig-4].
Mammographic and sonographic findings can overlap with other entities such as mastitis and breast cancer. In younger patients, infection or granulomatous disease should be considered. Less common conditions like tuberculosis and syphilis can have similar imaging findings [3] [Table/Fig-4].
Infectious mastitis occurs by a similar mechanism to actinomycosis, extending through the nipple after trauma or surgery. However, infectious mastitis is usually acute and due to more typical organisms such as Staphylococcus aureus. Abscess formation can also be present with infectious mastitis [8]. Abscesses present as irregular, heterogeneous masses with peripheral Doppler flow on sonography [9]. The patient often complains of acute breast swelling and warmth with erythematous skin changes.
Male breast cancer can present with findings similar to breast infection like focal skin thickening and mass. The presence of calcifications within the mass on mammography can be helpful in differentiating tumor from infection [10]. Sonography demonstrates an irregular hypoechoic mass or complex cystic mass. Colour Doppler may show increased flow within the mass or in the periphery. Additional sonographic findings include skin thickening and/or architectural distortion [9]. Clinically, breast cancer can present with nipple ulceration or retraction, which may suggest the diagnosis [10].
Less common entities like tuberculosis and syphilis can have overlapping clinical and imaging features. Mammographic findings in tuberculosis and syphilis include coarse stromal texture, focal skin thickening, sinus tract, or abscess formation. Sonographic findings includefocal skin thickening, sinus tract or abscess formation without increased Doppler flow. Nodular forms may present as multiple, heterogeneous hypoechoic masses with irregular borders [11] [Table/Fig-4].
Distinguishing breast actinomycosis from other infectious entities, chronic mastitis, breast tuberculosis, syphilis, and carcinoma on imaging studies may be challenging. The diagnosis of actinomycosis is rarely suspected prior to tissue sampling or culture of discharge. The method of sampling depends on the clinical presentation and sonographic findings. In instances where there is nipple discharge, culture of the discharge should be performed initially [2]. In the absence of a discharge for culture, percutaneous tissue biopsy or aspiration is often needed to make a definitive diagnosis [11,12]. Solid masses require ultrasound guided core biopsy [2]. Pathologic diagnosis of actinomycosis is made by observing characteristic sulfur granules, which represent bacterial colonies [3].
The prognosis is excellent with antibiotic and/or surgical treatment [6,13]. The treatment of choice for actinomycosis regardless of species is prolonged antibiotic therapy with penicillin [5]. Alternative antibiotic treatments include doxycycline, erythromycin, or clindamycin. If actinomycosis infection presents with abscess formation, it can be managed with percutaneous drainage of the collection and antibiotic treatment. If medical treatment fails, surgical intervention may be required [3] [Table/Fig-3].
Conclusion
Primary breast actinomycosis is unusual and has thus far primarily been reported in the female breast but it can also occur in the male breast. Typical imaging findings include focal skin thickening, abscess and sinus tract formation. Its indolent course may suggest infection secondary to unusual organisms, such as actinomycosis, tuberculosis or syphilis. Symptoms and imaging findings can overlap with other conditions requiring pathology or culture of the nipple discharge to make a definitive diagnosis.
[1]. Thambi R, Devi L, Sheeja S, Poothiode U, Primary breast actinomyces simulating malignancy: a case diagnosed by fine-needle aspiration cytologyJ Cytol 2012 29(3):197-99.PMID: 23112463 [Google Scholar]
[2]. DaieGhazvini R, Zaini Z, Zibafar E, Omidi K, First case report of primary actinomycosis of the breast due to ActinomycesIsraelii from IranActa MedicaIranica 2003 41(2):110-12. [Google Scholar]
[3]. Salmasi A, Asgari M, Khodadadi N, Rezaee A, Primary Actinomycosis of the breast presenting as a breast massBreast Care 2010 5(2):105-07.PMID: 20847823 [Google Scholar]
[4]. Attar KH, Waghorn D, Lyons M, Cunnick G, Rare species of actinomyces as causative pathogens in breast abscessBreast J 2007 13(5):501-05.PMID: 17760673 [Google Scholar]
[5]. Nielsen HL, First Report of Actinomyceseuropaeus bacteraemia result from a breast abscess in a 53 year old manNew Microbes New Infect 2015 7:21-2.PMID: 4477111 [Google Scholar]
[6]. Von Graevenitz A, Actinomycesneuii: review of an unusual infectious agentInfection 2011 39(2):97-100.PMID: 21340579 [Google Scholar]
[7]. Leibman AJ, Misra M, Castaldi M, Breast abscess after nipple piercing: sonographic findings with clinical correlationJ Ultrasound Med 2011 30(9):1303-08.PMID: 21876102 [Google Scholar]
[8]. Iuanow E, Kettler M, Slanetz PJ, Spectrum of disease in the male breastAJR Am J Roentgenol 2011 196(3):W247-59.PMID: 21343472 [Google Scholar]
[9]. Yitta S, Singer CI, Toth HB, Mercado CL, Sonographic appearances of benign and malignant male breast disease with mammographic and pathologic correlationJ Ultrasound Med 2010 29(6):931-47.PMID: 20498468 [Google Scholar]
[10]. Ballesio L, D’Ambrosio I, Ravazzolo N, Angeletti M, Di Pastena F, Tardioli S, Skin thickening as unique pathologic sign of an inflammatory breast cancer: a case report and review of the literatureClin Ter 2011 162(4):351-54.PMID: 21912823 [Google Scholar]
[11]. Sklair-Levy M, Muggia-Sulam M, Mally B, Primary breast tuberculosis diagnosed by sonographically guided core-needle biopsyJ Ultrasound Med 2006 25(10):1357-60.PMID: 16998113 [Google Scholar]
[12]. Farrokh D, Abedi M, Fallah Rastegar Y, Actinomycosis of the breastArch Iran Med 2012 15(11):731-32.PMID: 23102254 [Google Scholar]
[13]. Gómez-Garcés JL, Burillo A, Gil Y, Sáez-Nieto JA, Soft tissue infections caused by Actinomycesneuii, a rare pathogenJ Clin Microbiol 2010 48(4):1508-09.PMID: 20181910 [Google Scholar]